Research Article - (2022) Volume 0, Issue 0
Glycosylated Hemoglobin as a Predictor of Mortality in Severe Pneumonia by COVID-19
Mario Alberto Gutierrez Villarreal,
Javiera Francisca Marquez Echeverria,
Juan Carlos Mercado Villalba and
Natalia Taborda Taborda
Department of Critical Medicine and Intensive Care, Universidad Simon Boliv,a rAtlantico, Colombia
1General Physician ,Universidad del Norte, Barranquilla, Atlantico, Colombia
General Physician, Universidad Tecnica Privada, Cosmos Cochabamba, Bolivia
Doctor of Epidemiologist Universidad de Sucre, Sincelejo, Colombia
General Physician, Universidad Del Sinu, Monteria, Colombia
General Physician, Universidad Metropolitana de of Barranquilla, Atlantico, Colombia
2General Physician, Fundacion Universiteria San Martin, Pasto, Colombia
*Correspondence:
Isaias Garcerant Campo, Department of Critical Medicine and Intensive Care, Universidad Simon Boliv,a rAtlantico,
Colombia,
Email:
Received: 15-Mar-2022, Manuscript No. IPHSJ-22-12667;
Editor assigned: 18-Mar-2022, Pre QC No. IPHSJ-22-12667(PQ);
Reviewed: 23-Mar-2022, QC No. QC No. IPHSJ-22-12667;
Revised: 25-Mar-2022, Manuscript No. IPHSJ-22-12667(R);
Published:
01-Apr-2022, DOI: 10.36648/1108-7366.22.S6.928
Abstract
Glycosylated haemoglobin is one of the tests used in the diagnosis of diabetes mellitus; knowing their values shows us whether our ƉĂƚŝĞnƚƐ have developed de novo hyperglycaemia or, on the contrary, Suffer from one that had not been diagnosed; this is considered a risk factor for mortality and morbidity in ƉĂƚŝĞnƚƐ with severe pneumonia due to COVID-19 ŝnĨĞcƚŝŽn͘ It is important to know and evaluate their levels from the very moment of admission in order to be able to predict how they could be evolving
Keywords
Glycosylated haemoglobin; Mellitus diabetes;
Severe pneumonia; COVID-19 infection
Introduction
Diabetes mellitus is considered a chronic disorder that will be
characterized by high levels of glucose in the blood due to a
deficiency, either absolute or relative, of the hormone insulin;
This may be due to a deficiency in the action of the producing
cells (pancreatic beta cells) or because the body has created a
resistance to the action of insulin [1]. There are several ways to
diagnose the presence of diabetes mellitus in a patient, among
them we can use fasting glycaemia values greater than 126
mg/dl, blood glucose after the intake of 75 g of glucose at levels
greater than 199 mg/dl and glycosylated haemoglobin (HbA1c)
greater than or equal to 6.5%.
The prevalence of this disease has been increasing over the
years and could be explained by the bad eating habits that we
usually have in our daily lives. According to the Center for
Disease Control and Prevention (CDC) 34.2 million people have
diabetes (10.5% of the US population) of which 26.9 million
people are diagnosed, including 26.8 million adults and
undiagnosed 7.3 million people (21.3% are undiagnosed). In
Colombia, reports indicate that 3 out of every 100 Colombian
inhabitants have diabetes; however, it is believed that the real
number is much higher and those 1 in 10 inhabitants suffer from
it and that is because almost half of the individuals with this
pathology do not know that they are sick.
In December 2019, an infection was unleashed by a new virus
that causes pneumonia. This virus was named by the World
Health Organization (WHO) as Severe Acute Respiratory
Syndrome Corona Virus-2, (SARS-CoV-2) and the disease
COVID-19. And it was not until March 2020 that it was declared
a pandemic due to its rapid spread throughout the world [2].
Throughout all this time, many studies have been carried out
where it has been found that the presence of SARS-CoV-2
pneumonia in patients who have some comorbidities such as
arterial hypertension, cardiovascular diseases, chronic
obstructive pulmonary disease and Diabetes mellitus is
associated with a high rate of complications during the evolution
of the infection that could lead to death in the worst cases
compared to the general population [3].
The presence of acute or chronic hyperglycaemia generates
damage at the endothelial level, which is why it is important to
constantly measure glucose levels in diabetic patients as
predisposing factors for mortality and morbidity in COVID-19 pneumonia, especially plasma levels in the last 3 months
(HbA1c); These altered levels would indicate chronic
hyperglycaemia and thus a higher risk of complications. Our
study is based on determining whether glycosylated
haemoglobin is a predictor of mortality in patients with
COVID-19 pneumonia.
Materials and Methods
An exhaustive literature search was carried out using research sources of academic interest such as articles and scientific guides in Spanish and English published in the last six years, taking as a sample a series of them published in different national and international journals, as well as some databases including PubMed, Elsevier, science direct and sky. The following MESH and DeCs terms were used for the search: glycosylated haemoglobin, COVID 19, hyperglycaemia, diabetes mellitus, among others.
Diabetes in patients with COVID-19
Diabetes mellitus is a chronic inflammatory disease characterized by metabolism and cardiovascular complications [4]. In patients with diabetes, mortality increases due to infectious diseases, especially sepsis and pneumonia. Diabetes mellitus causes a pro-inflammatory state [5]. It has been shown that diabetes not only causes epithelial dysfunction of the pulmonary cilia, increased permeability of the vascular system and even damage and collapse at the alveolar level, but also leads to an abnormal function of the immune system [6]. Respiratory tract infections of bacterial and viral etiology are common in diabetic patients; it is believed to be due to neutrophil dysfunction, decreased T-cell response and alterations in humoral immunity. Regardless of the agent, pneumonia is associated with increased risk of morbidity and mortality in diabetic patients In COVID-19 infections, early interferon responses are suppressed, and then secondary maladaptive, delayed, and exaggerated interferon responses lead to storm of cytokines, resulting in organ damage. Alterations in the functions of the endothelial-epithelial barrier and hypercoagulability in the micro vascular bed lead to a cytokine storm, which is evidence of a poor prognosis of the disease. When COVID-19 and diabetes coexist, the possibility of a cytokine storm leads to organ damage increases exponentially in diabetic patients. A study reported that diabetic patients affected by COVID 19 have more severe inflammation and higher mortality risk [7].
Intra-hospital hyperglycaemia in patients with COVID-19
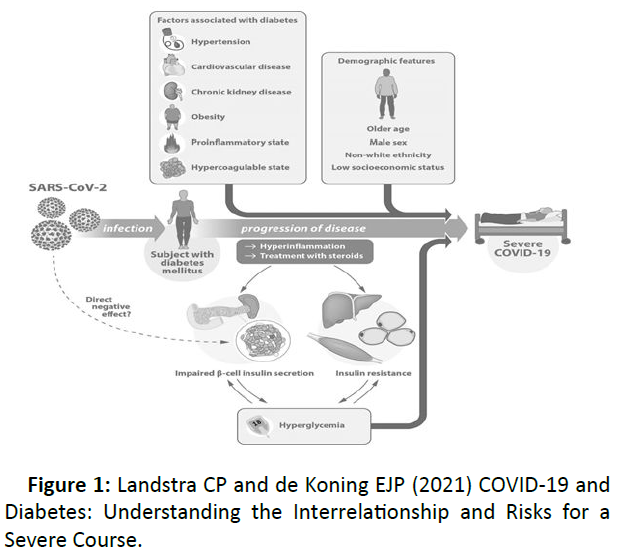
In-hospital hyperglycaemia in patients with and without diabetes has increased dramatically; associated with a hyper inflammatory state, steroid use, and pancreatic beta cell damage by COVID-19, anxiety, diabetes mellitus, and adipose tissue dysfunction. There are certain factors related to the development of hyperglycaemia in these patients (Figure 1) [8].
Figure 1: Landstra CP and de Koning EJP (2021) COVID-19 and Diabetes: Understanding the Interrelationship and Risks for a Severe Course.
Hyperglycaemia induces a chronic low-grade inflammatory state that reduces the activity of neutrophils and macrophage, favouring the growth of intracellular pathogens, also leads to a decrease in the antiviral immune response and increases the replicative capacity of bacteria in the respiratory tract. It has been shown that hyperglycaemia can cause direct glycosylation of proteins, thus altering the structure of the complement, and can cause a cytokine storm [9,10].
There may be two major variants in which in-hospital hyperglycaemia may be present, understood as the presence of blood glucose values greater than 140 mg/dl: one is that it is associated with diabetes mellitus (with or without a previous diagnosis) and another is that it is not (hyperglycaemia due to the stress generated by the COVID-19 infection). Due to this recent relationship, it is essential to know the values of glycosylated haemoglobin in order to know if it is new or old. In patients who are not diabetic and with HbA1c results greater than 6.5%, it suggests a diabetes mellitus that is not of recent evolution and that was not diagnosed prior to hospitalization; which is associated with a worse prognosis of acute respiratory disease caused by the virus. Hyperglycaemia is an important factor for DM patients influencing the incidence and course of sepsis. It is also an important prognostic factor when patients have sepsis and do not have DM [10,11].
Glycosylated haemoglobin and COVID-19
Glycosylated haemoglobin is a valuable test used in the diagnosis and glycaemic control of diabetes mellitus, it refers to the union of glucose with the terminal portion of the beta chain of haemoglobin A, this union is mediated by a chemical reaction enzymatic whose purpose is the formation of glycoproteins, a process that takes place within the red blood cell, depending on the sugar that binds to haemoglobin, different sub fractions of minor or fast haemoglobins will be obtained (HbA1a, HbA1b and HbA1c). Glucose is a molecule with a high percentage of circulation, so haemoglobin is constantly exposed to said binding process, that is, the higher its concentration in the blood, the greater the glycosylated haemoglobin will be. There are many conditions that can alter the values of this test, especially those that affect the blood component of the body, for example, sickle cell anaemia, haemodialysis, erythropoietin therapy, and even Pregnancy [12,13]. Diabetes and COVID-19 can mutually lead to alterations in the immune and respiratory systems. COVID-19 in diabetic patients has been associated with more severe inflammation, hypercoagulability, even low oxygenation, and ultimately higher mortality. Studies have shown that COVID-19 patients with high HbA1c levels may exhibit a higher severity level compared to those without, and the infection itself may also lead to an increased HbA1c level6. Another study showed that patients with high levels of HbA1c developed higher maximum levels of CRP and IL-6 during their stay in the ICU. There was a trend towards higher hospital mortality with the increase in HbA1c9. A study that included 183 patients diagnosed with COVID-19, of these 46 admitted to the hospital, showed that HbA1c ≥ 9% was associated with a significantly higher risk of hospitalization [14]. A meta-analysis reported that severe COVID-19 is associated with increased blood glucose levels. Slightly higher HbA1c was also found in severe COVID-19 patients compared to those with mild COVID-19 [15].
Results and Discussion
Coronavirus disease 2019 has a wide spectrum of clinical
manifestations ranging from asymptomatic infections to severe
respiratory symptoms and even death. Diabetes mellitus is
considered an important risk factor for an adverse outcome in
patients with COVID-19. Diabetes mellitus is a chronic, metabolic
and inflammatory disease that in its pathophysiology
predisposes to the development of infectious diseases because a
state of Chronic hyperglycaemia leads to an alteration of both
humoral and cellular immunity, in addition 1 the microangiopathic
changes of diabetes mellitus are accompanied by
alterations in pulmonary gas diffusion, as well as an abnormal
function of the peripheral airways, which predisposes to a
greater susceptibility to the development of respiratory failure.
Glycosylated haemoglobin is considered a marker used in the
follow-up of patients with diabetes mellitus, which measures
average glycaemic levels over a period of 2 to 3 months and
predicts the development of diabetic complications. Most
studies examining the relationship between blood glucose
control, glycosylated haemoglobin levels, and disease severity
and mortality in individuals with COVID-19 have shown that
good blood glucose control and at or near goal glycosylated
haemoglobin have been associated with a favourable prognosis,
shorter hospitalizations, and lower mortality rate, another study
showed that glycosylated haemoglobin was slightly higher in
individuals with severe COVID-19 than in those with COVID-19
mild 15, a study showed that increased levels of HbA1c are
associated with inflammation, hypercoagulability and low SaO2
in patients with COVID-19, and the mortality rate is higher in
diabetic patients.
Conclusion
As a consequence of the above, we conclude that the use of
glycosylated haemoglobin as a predictor of mortality in the patient infected by the COVID-19 virus is an aspect to consider,
because it offers us a broad history of the person's glycaemic
behaviour, leaving in I manifest to those who have diabetes
mellitus that, as we well know, it is associated with
complications and severity in the course of the infection, taking
this into account, glycosylated haemoglobin would fulfil this
function of foreseeing that fatal scenario in the patient; which
would undoubtedly be very useful information at the time of
choosing the appropriate treatment, which has undoubtedly
meant a great challenge in terms of dealing with the COVID-19
infection. In this sense, we consider that glycosylated
haemoglobin should be part of the diagnostic arsenal and
predictor of mortality in COVID-19 infection.
REFERENCES
- Harreiter J, Roden M (2019) Diabetes diagnosis, screening and DdGiGnoZn Wien Klin Wochenschr 131:6-15.
Indexed at, Crossref
- Bello LG, Salinas JT, Gimenez MB, Flores LE, Ruiz NG et al. (2018) the risk of those who take care of the risk FINDRISK in white Rev virtual. Soc Parag Med Int 3:71-76.
Crossref
- Torres E, Acosta A, Sobarzo P, Perez H (2021) Clinical and laboratory and mortality predictors of with COVID-19. Hosp Rev Science health 3:26-37.
Google Scholar
- Unluguzel Ustun G, Keskin A, Aci R, Arslanbek Erdem M, Ari M et al. (2021) benzene between Hb A1c and Severity of COVID-19. Hemoglobin 45:124-8.
Google Scholar, Crossref
- Fadini GP, Morieri ML, Boscari F, Maran A (2020) Newly-diagnosed diabetes and admission hyperglycaemia predict COVID-19 severity by respiratory. Diabetes Res Clin Pract 168:108374.
Indexed at, Google Scholar, Crossref
- Wang Z, Du Z, Zhu F (2020) Glycosylated hemoglobin is associated with systemic hypercoagulability and prognosis of COVID-19. Diabetes Res Clin Pract J 164:108214.
Indexed at, Google Scholar, Crossref
- Gao Q, Hu Y, Dai Z, Xiao F, Wang J (2020) the Epidemiological of 2019 Novel Coronavirus Diseases (COVID-19) in Jingmen, China. SSRN Electron J 2:113-22.
Indexed at, Google Scholar, Crossref
- Inzunza-Cervantes G, Lopez-Lopez RM, Ornelas-Aguirre JM, Flores Montes GV et al. (2021) In-hospital hyperglycaemia during COVID-19 in with no previous diagnosis of diabetes: report of three cases. Rev Mex Endocrinol Metab Nutr 8:134-142.
Google Scholar
- Oman-Gonzalez A, Rodriguez LA, Builes-Barrera CA, Castro DC, Builes-Montano CE et al. (2021) Diabetes mellitus y COVID-19: propuesta de tratamiento para el control glucemico en el oGmDZ de la pandemia. 34:161-71.
Google Scholar, Crossref
- Klein SJ, Fries D, Kaser S, Mathis S, Thome C et al. (2020) Unrecognized diabetes in COVID-19. Crit Care 24:406.
Indexed at, Google Scholar, Crossref
- Paz Ibarra J (2020) Management of diabetes mellitus in of COVID-19. Medical Peru 37:176-85.
Google Scholar
- Bracho-Nava M, Stepenka-Alvarez V, Sindas-Villasmil M, Rivas De Casal Y, Bozo De Gonzalez M et al. (2015) Glycosylated Hemoglobin or Glycated hemoglobin, which of the two. Biomed 27:521-529.
Google Scholar
- American Diabetes ADA-Standards-of-Medical-CareDiabetes-Care (2021) J Appl Res High Educ. 44:244.
Google Scholar, Crossref
- Merzon E, Green I, Shpigelman M, Vinker S, Raz I et al. (2021) Haemoglobin A1c is a predictor of COVID-19 severity with diabetes. Diabetes Metab Res Rev 37:3398.
Google Scholar, Crossref
- Chen J, Wu C, Wang X, Yu J, Sun Z et al. (2020) The Impact of COVID-19 on Blood Glucose: A Review and Meta-Analysis. Front Endocrinol 11:1-8.
Google Scholar, Crossref
Citation: Citation: Campo IG, Villarreal MAG, Echeverria JFM, Villalba JCM, Taborda NT, Velasquez YLF, et al. (2022) Glycosylated Hemoglobin as a Predictor
of Mortality in Severe Pneumonia by COVID-19. Health Sci J. Vol.16 No.S1:928