Lais Bomediano de Souza1, Emanuela Ribeiro2, Fernando Silva2, Marinice Duarte da Ponte2, Roberto Carvalho2, Hadassa Louback Paranhos1, Jose Luis Braga de Aquino1, Vania Aparecida Leandro Merhi1, Idiberto José Zotarelli Filho3*, Elisa Teixeira Mendes1,2
1Faculty of Medicine, Pontifical Catholic University of Campinas, PUC, Brazil
2Campinas Maternity Hospital, Campinas/SP, Brazil
3Post Graduate and Continuing Education (UniPOS), Street Ipiranga, 3460, Sao Jose do Rio Preto SP, Brazil
- *Corresponding Author:
- Idiberto Jose Zotarelli Filho, MSc., Ph.D
UniPOS - Post Graduate and Continuing Education
Street Ipiranga, 3460
Sao Jose do Rio Preto SP, Brazil 15020-040
Tel: +55(17) 98166-6537
E-mail: m.zotarelli@gmail.com; scientificresearch@unipos.com.br
Received date: July 23, 2019; Accepted date: August 09, 2019; Published date: August 16, 2019
Citation: de Souza LB, Ribeiro E, Silva F, da Ponte MD, Carvalho R, et al. (2019) Hospital Outbreak of Respiratory Syncytial Virus in Neonatal Intensive Care Unit. What is the Risk of Admitting External Patients? Health Sci J 13:4. DOI: 10.21767/1791-809X.100670. DOI: 10.36648/1791-809X.1000670
Keywords
Hospital outbreak; Respiratory syncytial virus; Neonatal; ICU
Introduction
Respiratory syncytial virus (RSV) is the main etiological agent responsible for respiratory tract infection in newborns (NB), infants and children [1]. The typical clinical picture of the infection includes nasal congestion, coryza, fever, cough, tachypnea, and dyspnea accompanied by wheezing, characteristic of bronchiolitis and the most common complication of the disease [2]. The main risk factors for developing severe conditions in infants are prematurity, congenital heart disease, chronic lung disease of prematurity and immunodeficiencies [3,4].
The virus has an incubation period of 4 to 6 days and high transmissibility, with the capacity to remain viable on surfaces for hours [5]. Therefore, in the seasonal period hospital outbreaks are frequent [6].
RSV outbreaks have great relevance in hospital settings, especially in neonatal ICU, where there are a large number of vulnerable patients and a high risk of in-hospital cross-transmission [6]. The number of outbreaks in neonatal ICU by viral infections is significant and the RSV accounts for 17.19%, according to the literature [7]. Neonates infected with RSV at the hospital have several risk factors for poor prognosis, with 13.5% mortality [7].
The metropolitan region of Campinas registered, in 2017, an RSV epidemic in the seasonal period (Secretaria de Saude-Campinas) [8]. During this period, the Maternity Hospital of Campinas admitted 32 NB infected with RSV and recorded an outbreak of 12 cases of in-hospital transmission.
The objective of this study was to report an outbreak of RSV occurring in the Neonatal ICU and to discuss the risk of contact of premature and vulnerable newborns with community-acquired viruses.
Methods
Study design
From the retrospective review of medical records, data were collected to analyze clinical factors, severity, and prognosis. The variables included were: gestational age (GA), birth weight, presence of comorbidities, signs, and symptoms, length of hospital stay, use of mechanical ventilation, use of mechanical ventilation, use of vasoactive drugs, laboratory abnormalities and clinical outcome discharge or death). Based on the collected data, it was decided to divide the infected population into two groups: those who were infected in the community (external) and those who were infected in the unit, who was hospitalized from birth (internal).
This study reports the hospital outbreak of RSV in the Neonatal ICU (Intensive Care Unit) of Campinas Maternity Hospital during the seasonal period (April-August) of 2017, through the review of medical records and data collection of all patients admitted to the unit with positive nasal lavage for RSV (n=44).
The metropolitan region of Campinas, with 3.2 million inhabitants, has as reference the Maternity Hospital of Campinas for the accomplishment of low and high-risk deliveries and hospitalization of neonates with indication of intensive care in the neonatal period; the unit receives patients transferred from other hospitals and neonates born at the Maternidade de Campinas for up to 28 days of life. The hospital has 212 beds for pregnant and puerperal women, 36 vacancies in the Neonatal ICU and 25 vacancies in a semi-intensive neonatal unit, on separate floors.
The laboratory analysis was performed by nasal washes for RSV test using the immunochromatographic method (Alere-Abbott ®) for all neonates hospitalized in the Neonatal ICU every 48 hours, including those already positive.
High respiratory symptoms were defined as coryza, nasal obstruction, sneezing, coughing, and hoarseness. Low respiratory symptoms were considered: fatigue, dyspnea, tachypnea, respiratory effort and signs of reduction of vesicular murmur, wheezing, rales, and fall of SatO2. The NB included in the study was all those with a positive nasal lavage result (Alere-Abbott ®).
Statistical Analysis
Statistical analysis was performed with chi-square variables in the categorical variables and t-student for the continuous variables, the analyzes were performed with the Epiinfo 7.2.2.6 program, p<0.05 was considered significant.
Ethics
The study was approved by the Ethics and Reference Research Committee (CEP).
Results
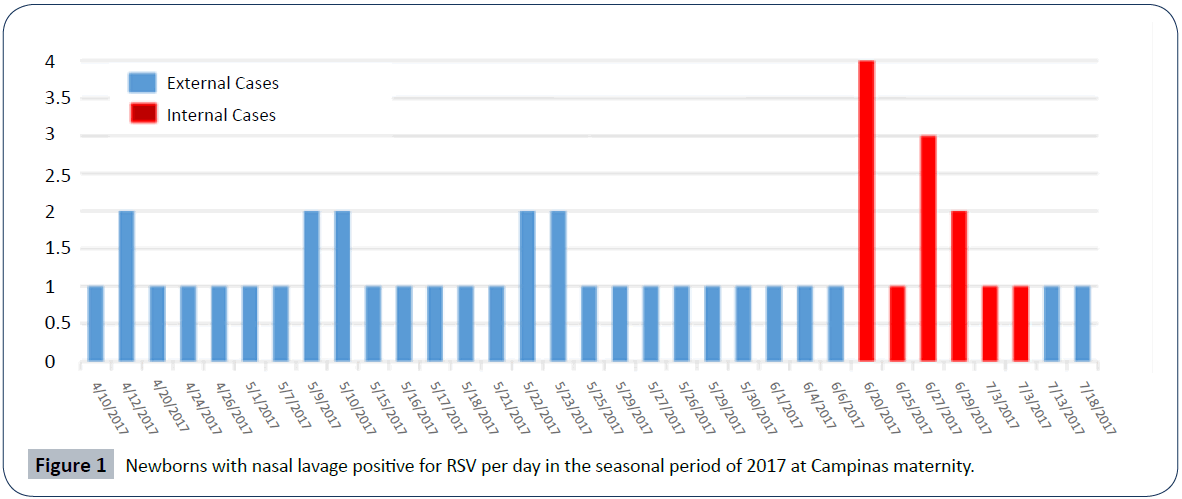
In April 2017 a RSV epidemic occurred in the Campinas region and 32 newborns from the community were admitted to the maternity ward. On June 20, the first case of in-hospital transmission of the virus was detected, followed by another 11 infections of neonates hospitalized at the unit (Figure 1). During the outbreak, several hospital infection control measures were adopted, including a cohort of patients and staff for positive cases of RSV and respiratory symptoms, exchange of alcoholic products for hand hygiene, daily training on good practices and blocking new hospitalizations of pregnant women and transfers of newborns.
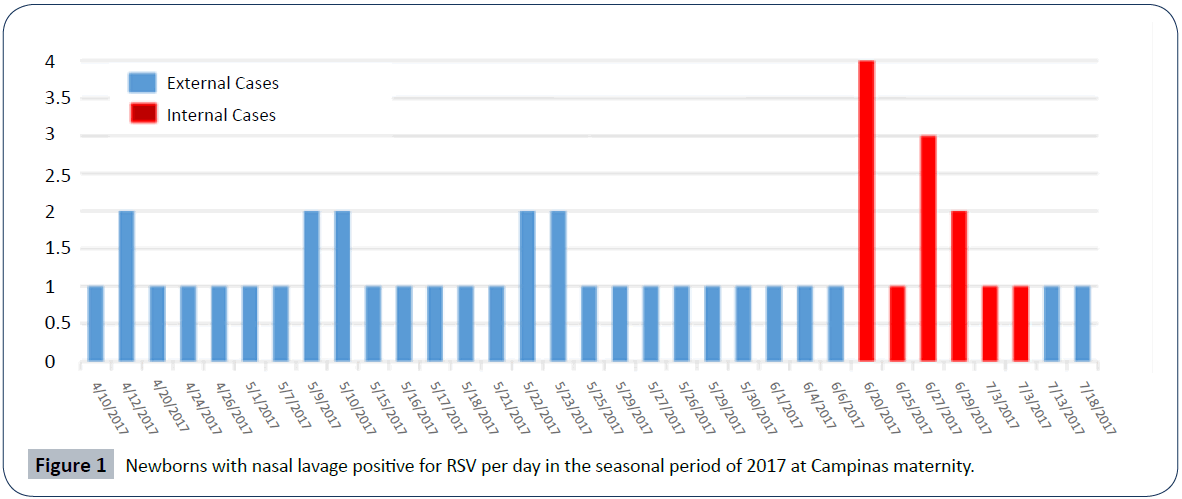
Figure 1: Newborns with nasal lavage positive for RSV per day in the seasonal period of 2017 at Campinas maternity.
The mean gestational age (GI) was 35 weeks and 5 days, with 20.4% of newborns born less than 32 weeks. The minimum GI was 24 weeks and 5 days and maximum of 41 weeks and 1 day. The presence of comorbidities was found in 29.5%. There was a need for mechanical ventilation in 43.1% and vasoactive drugs in 18.1%. The presence of clinical symptoms was in approximately 91%, and high symptoms were present in 31.8% and symptoms low in 68.1%. Regarding origin, 73% (32) were external and 27% (12) internal (Table 1).
Table 1 Characteristics of newborns infected with RSV during the outbreak at campinas maternity, 2017.
| Variables |
N (%) |
| Mean Gestational Age (max-min) |
37 weeks and 5 days (41s1d - 24s5d) |
| Women |
22 (50%) |
| Male |
22 (50%) |
| Comorbidities |
13 (29.5%) |
| Premature <32 weeks |
9 (20.4%) |
| Internal NB |
12 (27%) |
| External NB |
32 (73%) |
| Clinical Symptoms |
40 (90.9%) |
| Upper Respiratory Symptoms |
14 (31.8%) |
| Low Respiratory Symptoms |
30 (68.1%) |
| Mechanical ventilation |
19 (43.1%) |
| Vasoactive drug |
8 (18.1%) |
| Death |
1 (2.2%) |
The prior clinical condition of the newborns varied according to their origin: most of the infants from the community were previously healthy and full-term infants, unlike internal infants, who presented with comorbidities and extreme prematurity. The comparison between the two groups (internal vs. external NB), described in Table 2, shows differences in relation to risk factors, prognosis and clinical presentation. The mean GI of the external ones was 38 weeks and 2 days whereas the internal GI was 29 weeks and 1 day (p<0.001), and of the 12 internal NB 61% were extreme premature (p<0.001). The mean birth weight was 3105.9 g in the external and 1132.9 g in the internal, and the maximum birth weight of the internal NB was 655 g (Table 2).
Table 2 Clinical comparison between internal and external NB, infected by RSV during the outbreak at Campinas Maternity, 2017.
| Features |
NB external% (N) |
NB internal% (N) |
p |
| Premature (<37 weeks) |
13.3% (4) |
91.6% (11) |
< 0.001 |
| Comorbidities |
3.13% (1) |
100% (12) |
< 0.001 |
| Upper Respiratory Symptoms |
93.75% (30) |
8.3% (1) |
<0.001 |
| Low Respiratory Symptoms |
62.5% (20) |
75% (9) |
0.29 |
| Mechanical Ventilation (VM) |
37.50% (12) |
58.33% (7) |
0.18 |
| Asymptomatic |
0 |
25% (3) |
0.03 |
| Length of hospitalization days - Mean (change) |
11.3 (3-49) |
81.4 (21-150) |
<0.001 |
| Time of VM days Mean (range) |
1.9 (0-8) |
17.2 (11-59) |
<0.001 |
The clinical presentation of the viral infection also varied between the two groups: high respiratory symptoms were more prevalent in external NB, while low respiratory signs and symptoms were the main manifestations of internal NB (Table 3).
Table 3 Most prevalent manifestations in internal and external NB.
| Internal |
N (%) |
| Reduced MV |
7 (58.3%) |
| Respiratory Effort |
7 (58.3%) |
| Adventitious Noises |
5 (41.6%) |
| Asymptomatic |
3 (25%) |
| External |
N (%) |
| Cough |
27 (84.3%) |
| Respiratory Effort |
20 (62.5%) |
| Fever |
14 (43.7%) |
| Nasal obstruction |
11 (34.3%) |
Mechanical ventilation time and hospitalization time were higher in internal patients, both with statistical significance (0.03 and <0.001, respectively). The presence of comorbidities was 100% in the internal patients and 3.1% in the internal ones (p<0.001) (Table 2).
All NB with Centers for Disease Control and Prevention (CDC, 2010) to receive Palivizumab had the application performed. A death associated with infection occurred in the inpatients group (8.3%) [9].
Discussion
Acute viral bronchiolitis caused by RSV can be a manifestation of high severity in neonates, especially those hospitalized in neonatal intensive care units who present risk factors that compromise the severity of the disease, such as extreme prematurity, heart disease and pneumopathies associated with prematurity [1]. The occurrence of an outbreak in this scenario has catastrophic consequences, seriously compromising the prognosis of an already vulnerable population [2,3].
The manifestations due to RSV infection are variable according to the patient: previously healthy NB from the community present, for the most part, classic symptoms of bronchiolitis and high-risk premature newborns may present atypical symptoms [10]. In our series, the internal NB presented a non-specific respiratory clinical picture, ranging from asymptomatic cases to significant ventilatory worsening, with a significant risk of poor respiratory evolution and longer hospitalization time (Table 2). Authors consider that the positive respiratory virus in asymptomatic patients does not necessarily represent an infection, and the RN can only be colonized, maintaining a possible source of cross-transmission in the unit; therefore surveillance should be universal and precocious, reducing the risk of outbreaks with devastating consequences [10,11].
Caserta et al. [12] emphasize the risk of newborn infants, term or preterm, coming from the community, hospitalized in neonatal ICU, due to the transmission of respiratory and gastrointestinal viruses. As observed in the Maternity outbreak, the prognosis and evolution of internal patients was less favorable, with an approximate 8-fold longer hospitalization time and a 10-fold longer mechanical ventilation time, which is according to literature data also demonstrated this elevated risk in internal NB [10].
In our sample, 1 death was recorded among 44 cases (2.2%), which, according to the literature, was a relatively low number, since the risk of death in patients at risk for RSV is 13% and arrives to 35% in Adenovirus infection [7].
Outbreak measures described in the literature were performed, except for the use of universal Palivizumab to reduce transmissibility, described in some reports [6,7,13]. However, Palivizumab was performed in all patients with indications for prophylaxis.
Viral outbreaks in neonatal ICU ((Intensive Care Unit) can reach the extreme of the need to prevent new hospitalizations, a fact that occurred in our service, seriously impacting the access to delivery of pregnant women in the public health service [7]. In addition, the financial impact may be irrecoverable, especially in public and philanthropic hospitals. Halassa et al. [14] attributed a US$ 1.2 million in outbreak of U.S. outbreak in 2005. Hospital outbreaks of RSV at Campinas Maternity brought clinical consequences to patients, but also had a financial impact on the institution and temporary reduction of number of vacancies in a community referral service. Despite being extremely important and prevalent, the role of viruses in hospital infections is neglected epidemiologically [7].
Conclusion
We consider it necessary to reassess the insecure practice of admitting NB external, and therefore, with community microorganisms, in the ICU-Neonatal, where there are preterm patients, with numerous comorbidities and extremely vulnerable. We believe that alternatively, admission to intensive pediatric units would be the most recommendable for this situation; however, we believe that this impact should be better evaluated in future studies.
24630
References
- Heinonen S, Suvari L, Gissler M, Pitkanen O, Andersson S, et al. (2019) Transient tachypnea of the newborn is associated with an increased risk of hospitalization due to respiratory syncytial virus bronchiolitis. Pediatr Infect Dis J 38: 419-421.
- Munoz FM, Jamieson DJ (2019) Maternal immunization. Obstet Gynecol 133: 739-753.
- Paes B, Kim D, Saleem M, Wong S, Mitchell I, et al. (2019) Respiratory syncytial virus prophylaxis in infants with congenital airway anomalies compared to standard indications and complex medical disorders. Eur J Pediatr 178: 377-385.
- Stein RT, Bont LJ, Zar H, Polack FP, Park C, et al. Respiratory syncytial virus hospitalization and mortality: Systematic review and meta-analysis. Pediatr Pulmonol 52: 556-569.
- Walsh EE (2017) Respiratory syncytial virus infection: an illness for all ages. Clin Chest Med 38: 29-36.
- French CE, Mckenzie BC, Coope C, Rajanaidu S, Paranthaman K, et al. (2016) Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systematic review. Influenza Other Respir Viruses 10: 268-290.
- Civardi E, Tzialla C, Baldanti F, Strocchio L, Manzoni P, et al. (2013) Viral outbreaks in neonatal intensive care units: What we do not know. Am J Infect Control 41: 854-856.
- Centers for Disease Control and Prevention (CDC) (2010) Prevention of Perinatal Group B Streptococcal Disease. A Public Health Perspective. MMWR 59: 1-36.
- Bennett NJ, Tabarani CM, Bartholoma NM, Wang D, Huang D, et al. (2012) Incidence and implications of unrecognized viral respiratory tract infections in premature infants during their birth hospitalization: a prospective surveillance study in two neonatal intensive care units. J Pediatr 161: 814-818.
- Elbadawi LI, Haupt T, Reisdorf E, Danz T, Davis JP (2015) Use and interpretation of a rapid respiratory syncytial virus antigen detection test among infants hospitalized in a neonatal intensive care unit-wisconsin. MMWR 64: 857-860.
- Caserta MT, Yang H, Gill SR, Holden-Wiltse J, Pryhuber G (2017) Viral Respiratory Infections in Pre-term Infants During and After Hospitalization. J Pediatr 182: 53-58.
- Quach C, Shah R, Rubin LG (2016) Burden of Healthcare-Associated Viral Respiratory Infections in Children's Hospitals. J Pediatric Infect Dis Soc 7: 18-24.
- Halassa NB, Williams JV, Wilson GJ, Walsh WF, Schaffner W, et al. (2005) Medical and economic impact of a respiratory syncytial virus outbreak in a neonatal intensive care unit. Pediatr Infect Dis J 24: 1040-1044.