Research - (2023) Volume 17, Issue 9
Knowledge sharing practice and associated factors among health professionals in Ethiopia
Addisalem Workie Demsash1*,
Atsede Mazengia2 and
Binyam Tilahun2
1Mettu University, College of Health Science, Department of Health Informatics, Ethiopia
2University of Gondar College of Medicine and Health Sciences, Institute of Public Health, Department of Health Informatics, Ethiopia
*Correspondence:
Addisalem Workie Demsash, Mettu University, College of Health Science, Department of Health Informatics,
Ethiopia,
Email:
Received: 03-Sep-2023, Manuscript No. Iphsj-23-14030;
Editor assigned: 05-Sep-2023, Pre QC No. Iphsj-23-14030(PQ);
Reviewed: 19-Sep-2023, QC No. Iphsj-23-14030;
Revised: 23-Sep-2023, Manuscript No. Iphsj-23-14030(R);
Published:
30-Sep-2023, DOI: 10.36648/1791- 809X.17.9.1056
Abstract
Background: Numerous health data and information are generated in the routine
activity of health facilities. These numerous health data and experiences are input for
information, experience, and knowledge sharing, and learning. Therefore, this study
aimed to assess knowledge-sharing practice and identify its associated factors among
health professionals.
Methods: A stratified simple random sampling technique among 423 samples was
conducted with an institutional-based cross-sectional study design. A pretested
self-administered questionnaire and STATA version 15 software were used for data
processing and analysis. Descriptive statistics and a multivariable logistic regression
model were applied to assess the strength of the association between dependent and
independent variables. A variable with a p-value <0.05 with 95% CI was considered as
a cut point.
Results: 423 respondents participated in this study. Health professionals’ knowledgesharing
practice was 65.01% (95% CI: 60.46-69.56). In multivariable logistic regression
analysis, awareness AOR=2.44, 95% CI= [1.32-4.50], willingness AOR=1.96, 95%
CI= [1.10-3.53], loss of knowledge power AOR=0.192, 95% CI= [.12-.32], availability
of health information resource AOR=2.00, 95% CI= [1.56-5.38], and opportunity
AOR=2.91, 95% CI= [1.71-4.95] were significantly associated with knowledge sharing
practice.
Conclusions: Health professionals’ knowledge-sharing practice was good, but not
optimal. Stakeholders needed to work on knowledge-sharing opportunities and
resource allocation to promote health professionals' knowledge-sharing practices, and
professionals recommended being willing for sharing experience and information.
Keywords
Knowledge sharing; Practice; Health professionals; Ethiopia
Introduction
In the healthcare industry, the routine practice of health
professionals generates a vast amount of health data
and information. Recording patients' socio-demographic
characteristics, diagnosis and treatment, laboratory tests and
medical imaging examinations and confirmation of the results,
drug, medication and prescriptions, clinical notes, and practices
are all part of a health professional's daily practice in a healthcare
facility [1]. So, health professionals may have their own set of best
experiences that they follow daily.
Identifying relevance, ethical soundness, effective and efficient
experience, knowledge, and sharing are all steps for health
professionals to learn from one another, resulting in success,
duplication, and healthcare sustainability [2]. Therefore, experience and knowledge are advancements in a particular
process, approach, or technique sufficient to replace and update
an existing practice [3], demonstrate individuals’ ability to work
well, and provide quality care [4]. Countries' experience with
health program planning, implementation, and monitoring of
health service delivery is an experience. As a result, daily-based
practices and experiences are documented and disseminated to
provide genuine opportunities for knowledge acquisition and
continuous learning through feedback and reflection for more
effective health interventions [5].
Since knowledge encompasses experience, daily-based practices,
values, contextual information, and insights, knowledge should
be well documented, organized, managed, and shared to create
further insights among health professionals for better evaluation
and interpretation of new health information [6]. Knowledge is created and exists in the human mind and normal behaviors,
procedures, and organizational standards [7]. So, health
professionals can share relevant and accurate health information
[8] from healthcare institutions’ experiences and colleagues’
skills [9, 10] to have a shared understanding of the recycling use
of information [11-13].
In the healthcare process, there are challenges such as
uncertainty in clinical decision-making (14), inaccessibility [15, 16], inconsistency [17] of credible evidence, an escalation of
health professionals' information needs [18] and inaccessibility
of accurate information [19]. When the pandemic arises [20],
many rumours and false news stories circulated on social media
[21]. During the emergence of new cases, experts might not
have sufficient experience [21], and patients are not well served
and don’t receive attractive treatments. These make them lose
their lives and develop adverse events due to knowledge-sharing
delays This is a sign of a marvellous amount of experience, medical
resources, and knowledge wastage in healthcare origination
Therefore, knowledge sharing is an important mechanism to gain
accurate knowledge and experience from credible sources to
reduce the challenges.
There has been a lot of research done on health professionals'
knowledge-sharing practices worldwide In studies conducted in
Ghana, health professionals’ knowledge-sharing is not attractive
Furthermore, evidence showed that 56.3% of health professionals
had encountered challenges in accessing health information and
experience in Ireland and 61% of health professionals had limited
expertise and knowledge-sharing practice in China.
In Ethiopia, most studies show low health information, knowledge,
and experience-sharing levels among health professionals [18].
The results showed that knowledge sharing about infection
prevention and adult cardiopulmonary resuscitation (CPR) in
Ethiopia is low and not ideal, respectively [19]. There are factors
associated with knowledge sharing among health professionals
for such unremarkable knowledge-sharing practices. Some of
them are lack of expertise, absence of formal knowledge-sharing
mechanism misunderstanding the importance and the best ways
of knowledge-sharing mechanism working experience monthly
salary low educational status level of motivation job satisfaction
and trust among colleagues willingness and awareness resource
allocation supportive leadership and opportunities [21] and
rewarding and recognition system Besides the low level of
knowledge-sharing practice, there is limited evidence on the
knowledge-sharing practice of health professionals working in
a specialized teaching hospital in Ethiopia. Therefore, this study
aimed to assess knowledge-sharing practices among health
professionals and identify associated factors.
Methods
Study design and settings
An institutional-based cross-sectional study design was conducted
to determine the knowledge-sharing level and identify associated
factors at the University of Gondar referral hospital. University of
Gondar Referral Hospital (UoGRH) is one of the hospitals among
the medical schools in Ethiopia. UoGRH was established in 1954 as a public health college and training institute and is 738 km far
from the capital city of Ethiopia, Addis Abeba UoGRH provides a
full range of healthcare services for all communities. According
to the human resource information, the hospital has 1336 health
professionals during the data collection period.
Study subject and inclusion criteria
All health professionals who are permanently working at the
UoGRH were the study's target population. Health professionals
available during the data collection period were included in the
study population. However, health professionals who had less
than six months of work experience and were not available
during the data collection period were excluded.
Sampling and sample size calculation
The single population proportion formula determined the sample
size We were using 50.3% of health professionals knowledge
sharing from the previous similar study as prevalence Standard
deviation (Zα/2 = 1.96), and margin of error (d=5%) at a 95%
confidence level. The total sample size with the adjustment of
none response rate (10%) was 423. The 423 respondents were
chosen using a stratified random sampling procedure, and the
sample was stratified by the department of work. Then, based
on the number of healthcare professionals in each service area,
the selection was proportionally allocated to the service area
to assess their knowledge-sharing practice. After proportionally
distributing samples in each service area, each department's
respondents were chosen using a random sampling procedure.
Variables of the study
The dependent variable studied was knowledge sharing. At the
same time, the independent variables include various sociodemographic
characteristics (age, sex, educational status, and
experience), individual factors (willingness, openness, awareness,
perceived loss of knowledge), organizational factors (supportive
leadership, resource allocation, and opportunities), knowledge
source (teamwork, health information resource availability of
report and documentation), and ICT and communication channel.
Operational definitions
Knowledge-sharing practice was measured using twelve closedended
questions with Likert scale response options ranging from
strongly disagree to strongly agree. The score on the mean and
above shows knowledge-sharing practice, and below the mean
shows the absence of knowledge-sharing practice among health
professionals.
Awareness of knowledge-sharing practices was measured by
four closed-ended Likert scale questions with response options
ranging from strongly disagree to strongly agree. The scores on
the mean and above show the presence of awareness, and the
value below the mean score indicates unawareness of knowledgesharing
practice.
Opportunity for knowledge sharing was measured with four
closed-ended questions, and the response to each question was
Likert scale ranging from strongly disagrees to strongly agree.
The scores with the mean and above show the opportunity for
knowledge sharing; otherwise, there is no opportunity.
Data collection procedure
Two-day intensive training on the study's objectives, data
collection techniques, and respondents’ rights were given to four
data collectors and three supervisors before data collection. A
clear, unambiguous, self-administered questionnaire was used
to collect the required data. It was adopted from similar articles
with some modifications in line with the study's objectives. The
tool contains questions about knowledge sharing and associated
factors such as socio-demographic characteristics, individual and
organizational factors, communication channels, and sources
of knowledge. A pretest was done on 5% of the total sample
at the Koladiba district hospital to ensure the consistency and
validity of the questionnaire. The knowledge-sharing practice's
Cronbach alpha rating was 0.89, indicating that the questionnaire
is extremely reliable.
Ethical clearance and consent to participation
All methods were carried out by following the Helsinki declaration.
Ethical approval was obtained from the ethical review board
of the University of Gondar College of Medicine and Health
Science, Institute of public health, with reference number Ref No
/IPH/837/6/2012. The purpose and aim of the study were clearly
explained to the study participants to avoid any confusion and
to make sure that the study was only for the stated objectives.
Then, informed verbal consent was obtained from the study
participants before the data collection. Any information related
to the study subject was kept in its confidential. Hence, there was
no human participation issue.
Data analysis
The data were entered into Epi info software version 7 for data
cleaning and coding, and Stata software version 15 was used for
data processing and analysis. A descriptive analysis was done to
describe the knowledge-sharing practice and socio-demographic
characteristics. Variables in the Bivariable logistic regression
analysis with p-value <0.02 were considered for further analysis.
Multivariable logistic regression was done to know the relation
between dependent and independent variables. Finally, variables
with a p-value ≤ 0.05 were considered factors associated with
knowledge sharing. Crude and adjusted odds ratios with 95%CI
were calculated to measure the strength of association between
the dependent and independent variables.
Results
Socio-demographic characteristics
Four hundred twenty-three (423) health professionals
participated in this study. Of the total respondents, 222 of 423
(52.48%) respondents were male, and more than two-thirds
(66.90%) of the respondents were degree and diploma holders.
Nearly three-fourth (74.70%) of health professionals were under
the age group of 21-30 years, and nearly one-third (29.08%) of
health professionals were general practitioners and specialties
next to nurse professionals (39.24%). The majority (83.92%) of
health professionals had ten and less than years of experience
(Table 1).
| Variable |
Category |
Frequency (n) |
Percent (%) |
| Sex |
Female |
201 |
47.52 |
| Male |
222 |
52.48 |
| Educational level |
Degree and below |
283 |
66.9 |
| Master |
17 |
4.02 |
| Gp and above |
123 |
29.08 |
| Age (in years) |
21-30 Years |
316 |
74.7 |
| 31-40 Years |
93 |
21.99 |
| >40 Years |
14 |
3.31 |
| Professions |
Nurse |
166 |
39.24 |
| Pharmacy |
22 |
5.2 |
| Laboratory |
39 |
9.22 |
| Doctors |
123 |
29.08 |
| Midwifery |
51 |
12.06 |
| Other |
22 |
5.2 |
| Experience |
<=10 years |
355 |
83.92 |
| >10 years |
68 |
16.08 |
Table 1. Socio-demographic characteristics of health professionals.
Knowledge sharing among health professionals
Of the total health professionals, 65.01% (95% CI: 60.46-69.56)
of health professionals had health knowledge-sharing practices,
whereas 34.99% of health professionals had no knowledgesharing
practice (Table 2).
Organizational and individual factors for
knowledge sharing
From the perspective of organizational factors, only 261 of 423
(61.70%) respondents had extrinsic motivation for knowledge
sharing. However, 226 of 423 (53.43%), 265 of 423 (62.65%),
and 285 of 423 (67.38%) health professionals revealed that they
had not the opportunity, supportive leadership, and resource
allocation for knowledge-sharing practice, respectively. More
than half of the 423 (52.25%) health professionals were satisfied
according to induvial factors. 388 of 423 (91.73%), 352 of 423
(83.22%), 334 of 423 (78.96%), 342 of 423 (80.85%), and 244 of 423
(57.68%) of the respondents had trust, awareness, willingness,
intrinsic motivation and openness about the knowledge sharing
practice respectively. However, 423 % of respondents perceive
knowledge power-sharing loss (Table 2).
| Variable |
Category |
Frequency (#) |
Percent (%) |
| Knowledge sharing practice |
Yes |
275 |
65.01 |
| No |
148 |
34.99 |
| Extrinsic motivation |
Yes |
261 |
61.7 |
| No |
162 |
38.3 |
| Opportunity |
Yes |
197 |
46.57 |
| No |
226 |
53.43 |
| Supportive leadership |
Yes |
158 |
37.35 |
| No |
265 |
62.65 |
| Resource allocation |
Yes |
138 |
32.62 |
| No |
285 |
67.38 |
| Job satisfaction |
Yes |
221 |
52.25 |
| No |
202 |
47.75 |
| Trust |
Yes |
388 |
91.73 |
| No |
35 |
8.27 |
| Awareness |
Yes |
352 |
83.22 |
| No |
71 |
16.78 |
| Willingness |
Yes |
334 |
78.96 |
| No |
89 |
21.04 |
| Perceived loss of knowledge power |
Yes |
186 |
43.97 |
| No |
237 |
56.03 |
| Intrinsic motivation |
Yes |
342 |
80.85 |
| No |
81 |
19.15 |
| Openness |
Yes |
251 |
59.34 |
|
No |
172 |
40.66 |
Table 2. Organizational and individual factors for knowledge sharing.
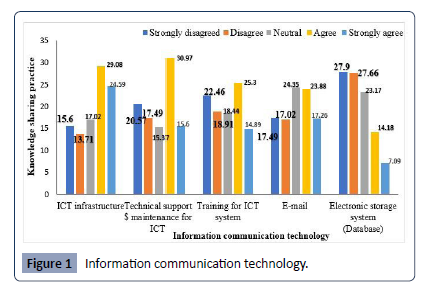
Information communication technology (ICT)
Regarding ICT, 53.67% of the respondents agreed/strongly agreed
on the availability of ICT infrastructure in the hospital, 46.57%
of the respondents agreed/strongly decided on the presence of
technical support and maintenance of the ICT system and 15.37%
of respondents were indifferent. 41.14% of the respondents
agreed/strongly agreed that they use email for communication.
Alternatively, 55.56% of health professionals disagreed/strongly
disagreed with the presence of a knowledge repository system
(database) to access knowledge. The remaining 23.17% of the
respondents were neutral, and 40.19% of health professionals
agreed/strongly agreed that there was training for ICT, whereas
18.44% were neutral (Figure 1).
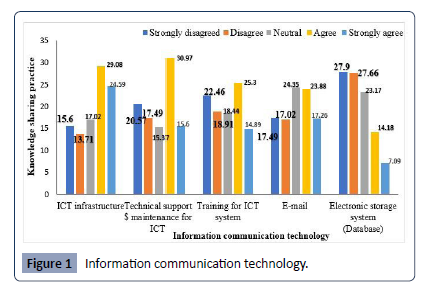
Figure 1: Information communication technology.
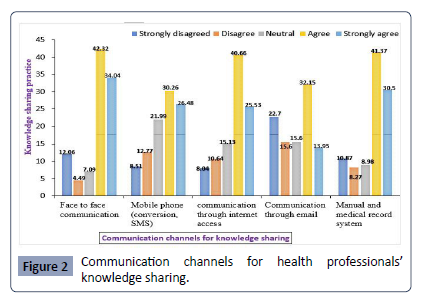
Regarding the communication channels, 76.36% and 71.87% of respondents indicated that face-to-face communication, manual,
and medical record system was the major communication channels
for knowledge-sharing practice in the hospital, respectively.
56.74% of health professionals stated that using mobile phones
for conversion and SMS text messages serves as communication
channels for knowledge-sharing practice purposes. 66.19%
of health professionals indicate that accessing the internet is
another communication channel to share knowledge. Still, only
46.1% of health professionals confirmed that using email is one
of the channels for knowledge-sharing practice in the hospital
(Figure 2).
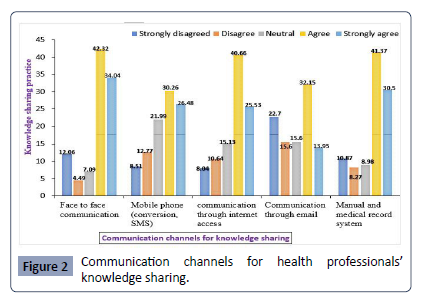
Figure 2: Communication channels for health professionals’
knowledge sharing.
Source of knowledge sharing
Of the total respondents, 298 of 423 (70.45%) and 341 of 423 (80.61%) health professionals indicated that teamwork and health
information resources were the major sources of knowledge in
the study area. 49.41% and 48.46% of respondents revealed that
reviewing the reported and documented files is also a knowledge
source at the University of Gondar hospital (Table 3).
Source of knowledge sharing |
Response |
Frequency |
Percent |
| Teamwork |
Yes |
298 |
70.45 |
| No |
125 |
29.55 |
| Reported file |
Yes |
209 |
49.41 |
| No |
214 |
50.59 |
| Documented file |
Yes |
218 |
51.54 |
| No |
205 |
48.46 |
| Health information resources |
Yes |
341 |
80.61 |
| No |
82 |
19.39 |
Table3. Major source of knowledge at the University of Gondar referral hospital.
Factors associated with the knowledge-sharing
practice
A total of 23 variables were entered into the binary logistic
regression model. From these variables, extrinsic motivation,
openness awareness, supportive leadership, willingness,
resource allocation, information, communication technology
(ICT), perceived loss of knowledge power, job satisfaction,
communication channels, opportunity, and the available health
information were turned out to be significant factors associated
with knowledge sharing practice from the Bivariable analysis.
However, in multivariable logistic regression analysis, awareness,
willingness, perceived loss of knowledge, power, opportunity,
and availability of health information resources were identified
as significant factors.
Respondents aware of the knowledge-sharing practice were
2.4 [AOR=2.44, 95%CI (1.32-4.50)] times more likely to share
knowledge than their encounter parts. Health professionals
willing to share knowledge were 2.00 [AOR=1.96, 95%CI (1.10-
3.53)] times more likely to share knowledge than those who
weren’t willing. Respondents with a perceived loss of knowledge
power were 81% [AOR=0.19, 95%CI (.12-.32)] less likely to
share knowledge than those who had not a perceived loss of
knowledge power. Respondents who have availability of health information resources (HIRs) and the opportunity for knowledgesharing
practice were 3 [AOR=2.00, 95%CI (1.56-5.38)] and 2.9
[AOR=2.91, 95%CI (1.71-4.95)] times higher to share knowledge
than their encounter parts respectively (Table 4).
| Variables |
|
Knowledge sharing practice |
|
COR-95%CI |
AOR-95%CI |
| No |
Yes |
| Awareness |
Yes |
109 (25.77%) |
243(57.45%) |
2.72(1.62-4.57)* |
2.44 (1.32-4.50) ** |
| No |
39(9.22%) |
32(7.57%) |
1 |
1 |
| Willingness |
Yes |
104(24.59%) |
230(54.37%) |
2.16 (1.34-3.48)* |
1.96 (1.10-3.53) ** |
| No |
44(10.40%) |
45(10.64%) |
1 |
1 |
| PLKP |
Yes |
101(23.88%) |
85(20.09%) |
.21(.14-.32)* |
.19 (.12-.32) ** |
| No |
47(11.11%) |
190(44.92%) |
1 |
1 |
| Job satisfaction |
Yes |
63(14.89%) |
158(37.35%) |
1.82(1.22-2.73) |
1.53 (.91-2.55) |
| No |
85(20.09%) |
117(27.66%) |
1 |
1 |
| Extrinsic motivation |
Yes |
73(17.26%) |
188(44.44%) |
2.22(1.47-3.35) |
1.51 (.89-2.56) |
| No |
75(17.73%) |
87(20.57%) |
1 |
1 |
| Openness |
Yes |
67(15.84%) |
184(43.50%) |
2.44(1.62-3.68) |
1.52 (.91-2.56) |
| No |
81(19.15%) |
91(21.51%) |
1 |
1 |
| Opportunity |
Yes |
41(9.69%) |
156(36.88%) |
3.42(2.22-5.27)* |
2.91 (1.71-4.95) ** |
| No |
107(25.30%) |
119(28.13%) |
1 |
1 |
| Supportive leadership |
Yes |
44(10.40%) |
114(26.95%) |
1.67(1.10-2.56) |
1.21(.70-2.10) |
| No |
104(24.59%) |
161(38.06%) |
1 |
1 |
| Resource allocation |
Yes |
29(6.86%) |
109(25.77%) |
2.69(1.68-4.32) |
.96 (.52-1.78) |
|
No |
119(28.13%) |
166(39.24 %) |
1 |
1 |
| ICT available |
Yes |
62(14.66%) |
160(37.83%) |
1.93(1.29-2.89) |
1.61(.98-2.65) |
| No |
86(20.33%) |
115(27.19%) |
1 |
1 |
HIRs
Availability |
Yes |
95(22.46%) |
246(58.16%) |
4.73(2.84-7.89)* |
3.00(1.56-5.38) ** |
| No |
53(12.53%) |
29(6.86%) |
1 |
1 |
| Communication channels |
Yes |
109(25.77%) |
231(54.61%) |
1.88(1.15-3.06) |
1.00(.51-1.92) |
| No |
39(9.22%) |
44(10.40%) |
1 |
1 |
| * Significant in COR at 95% CI, ** Significant in AOR at 95% CI , 1: Reference category |
Table 4. Bivariable and multivariable analysis of selected variables associated with the knowledge-sharing practice.
Discussion
In this study, the knowledge-sharing practice among health
professionals was 65.01% (95% CI: 60.46-69.56). This finding aligns
with a study done in Public Hospitals in North Showa But, this
finding is higher than the study done in different parts of Ethiopia
the possible reasons might be the difference in awareness,
willingness, ICT access, and presence of communication channels.
The odds of health professionals who have awareness about
knowledge sharing are 2.4 times higher to share knowledge
than those who don’t have an understanding. This finding is
supported by the report from St. Peter’s and Felege Hiwot’s
hospitals. This could be due to the presence of teamwork
(70.45%), availability of ICTs infrastructure (53.67%), and the
presence of different knowledge dissemination channels such
as face-to-face communication (76.36%), presence of manual
or electronic medical record systems (71.87%) for reviewing and
sharing experience in the study area. The odds of respondents
who are willing to share knowledge are 2.00 times higher to share
knowledge than those who are unwilling to knowledge-sharing.
This result is supported by studies done in Felege Hiwot referral
hospital and Malaysia; this might be due to the presence of trust
among staff (91.73), the presence of internet access (66.19%) in the hospital, their intrinsic motivation (80.85%), and extrinsic
motivation (61.70%) in the study area. In addition, using their
mobile phone (56.74%) for knowledge-sharing purposes lets
them get a consultation from their colleagues about how they
treat and diagnose the patients through SMS text messaging and
phone conversations.
This study reveals that health professionals who perceive they
lose power while sharing knowledge are 80.8% times less than
those who don’t sense they lose control while sharing knowledge.
This finding is consistent with the study done at Jordan Hospital
this may be due to misunderstandings about the significance and
benefits of knowledge sharing. Some health professionals are also
afraid that they will lose their position in the organization due to
sharing their knowledge with their colleagues. Since knowledge
is the most valuable property of the organization to deliver
excellent and better healthcare services to achieve organizational
objectives. But, the organization's absence of resource allocation
(67.38%) and poor supportive leadership (62.65%) don’t create
positive competition.
The number of respondents who have knowledge-sharing
opportunities is 2.91 times higher to share knowledge than those
who didn’t have a chance. This finding is supported by the report
from Gonji, Kolella, Felege Hiwot, and Mekelle hospitals, This
might be due to teamwork (70.45%) because teamwork is the
locus of both interaction patterns and intragroup communication.
The presence of informal knowledge-sharing opportunities
(60.52%) in this study area and the existence of motivation help health professionals to share knowledge.
Concerning health information resources, 80.61% of the
respondents confirmed that they have the availability of health
information resources for knowledge sharing. This finding is
higher than the studies done at North Showa and Addisabeba,
This may be due to the inadequate absence of health information
resources for knowledge-sharing activities and the availability
of books, workshops, guidelines, and the internet as a source
for knowledge-sharing in this study. Furthermore, the variation
might be due to sampling size differences.
Limitations and strengths of this study
Since the study was conducted cross-sectionally, the temporal
relationship in the multivariable logistic regression might occur.
The study would serve as input for policymakers and stakeholders to address health professional knowledge-sharing inquiries and
would serve as a baseline for future studies.
Conclusion
The level of knowledge-sharing practice among health
professionals was more than but not optimal. Awareness,
willingness, health information resources, perceived loss of
knowledge, power, and opportunity were significantly associated
with the knowledge-sharing practice. Sharing opportunities,
allocation of resources, and loss of knowledge power were not
adequate for knowledge-sharing practices. Stakeholders needed
to increase the opportunities and resources for knowledgesharing
practice, and health professionals share their experiences
and information they have with their colleagues for the best
patient care practice.
References
- Dash S, Shakyawar SK, Sharma M, Kaushik S (2019) big data in healthcare: management, analysis, and prospects. Journal of Big Data. 6: 1-25.
Google Scholar, Crossref
- Al-Rasheed A, Berri J (2016) Knowledge management of best practices in a collaborative environment. Int J Adv Comp Sci App IJACSA 7.
Google Scholar
- Dalkir K (2013) Knowledge management in theory and practice: Routledge.
Google Scholar
- Rabinowicz S, Chinapah V (2014) Good practices in the pursuit of sustainable rural transformation. J Edu Res 4: 7-23.
Indexed at, Google Scholar
- Organization (2017) WH A guide to identifying and documenting best practices in family planning programs.
Google Scholar
- Oliver GR (2013) A tenth-anniversary assessment of Davenport and Prusak (1998/2000) Working Knowledge: Practitioner approaches knowledge in organizations. Knowledge Management Research & Practice 11: 10-22.
Indexed at, Google Scholar
- Choo CW (1996) Knowing organization: How organizations use information to construct meaning, create knowledge and make decisions. Int J Inf Manag 16:329-340.
Google Scholar
- Hoegl M, Parboteeah KP, Munson CL (2003) Team‐level antecedents of individuals' knowledge networks Decision Sciences. 34:741-70.
Indexed at, Google Scholar, Crossref
- Andualem M, Kebede G, Kumie A (2013) Information needs and seeking behavior among health professionals working at public hospitals and health centers in Bahir Dar, Ethiopia. BMC health services research 13: 534.
Indexed at, Google Scholar, Crossref
- Areekkuzhiyil S (2019) Factors Determining the Knowledge Sharing Practices among Graduate Students in Kerala: An Empirical Analysis.
Indexed at, Google Scholar
- Gordon AN, Hinson RE (2007) towards a sustainable framework for computer-based health information systems (CHIS) for developed countries (LDCs). Int J Health Care Quality Assurance.
Google Scholar
- Li J, Wang J (2006) Motion compensation for wave measurement by X-band marine navigation radar. HAIYANG JISHU 25: 31.
Indexed at, Google Scholar, Crossref
- Grol R (2001) Successes and failures in the implementation of evidence-based guidelines for clinical practice. Medical care II46-II54.
Indexed at, Crossref
- Timmermans S, Angell A (2001) Evidence-based medicine, clinical uncertainty, and learning from the doctor. J Health Social Behavior 342-59.
Indexed at
- Grol R (2001) Successes and failures in the implementation of evidence-based guidelines for clinical practice. Medical care 39: II-46-II-54.
Indexed at, Google Scholar
- Schuster MA, McGlynn EA, Brook RH (1998) how good is the quality of health care in the United States? The Milbank Quarterly 76: 517-63.
Google Scholar, Crossref
- Khong TK, Missouris CG, Murda'h M, MacGregor GA (1998) The use of HMG Co-A reductase inhibitors following acute myocardial infarction in hospital practice. Postgraduate Med J 74: 600-601.
Google Scholar
- Zeng Q, Cimino JJ (1997) editors Linking a clinical system to heterogeneous information resources. Proceedings of the AMIA Annual Fall Symposium: American Medical Informatics Association.
Google Scholar
- Stroetmann B, Aisenbrey A (2012) Medical knowledge management in the healthcare industry. World Academy of Science, Engineering, and Technology 64:557-562.
Indexed at, Google Scholar, Crossref
- Huynh TL (2020) The COVID-19 risk perception: A survey on socioeconomics and media attention. Econ Bull 40: 758-764.
Google Scholar
- Syed S (2008) Health knowledge management: The art of possible. Faculty of Computer Science, Dalhousie University, Canada.
Google Scholar
Citation: Demsash AW, Mazengia A, Tilahun
B (2023) Knowledge Sharing Practice
and Associated Factors among Health
Professionals in Ethiopia. Health Sci J. Vol. 17
No. 9: 1056.