Review Article - (2022) Volume 0, Issue 0
Main Musculoskeletal Complications Secondary to Diabetic Neuropathy
Jonathan Gonzalez Walles,
Pastor Leonardo Jurado Escobar,
Oswaldo Pérez Cabra,
Juan Felipe Villegas Lora,
Sebastian Durango Conde,
Angela Lopez Garcia and
Helmy Yaimar Laguado Chacon
General Physician, Universidad Libre, Cali, Colombia, Colombia
General Physician, Universidad del Quindio, Colombia
General Physician, Universidad Industrial Santander, Colombia
General Physician, Universidad del Rosario, Bogota, Colombia
General Physician, Universidad del Norte, Barranquilla, Colombia
1General Physician, Universidad Libre, Cali, Colombia
General Physician, Universidad de Sucre, Sincelejo, Colombia
2General Physician, Universidad de Cartagena, Colombia
General Physician, Universidad de Cartagena, Colombia
*Correspondence:
Luis Eduardo De La Pena Restrepo, General Physician, Universidad Libre, Cali, Colombia,
Colombia,
Email:
Received: 12-Mar-2022, Manuscript No. Iphsj-22-12664;
Editor assigned: 14-Mar-2022, Pre QC No. PreQC No. Iphsj-22-12664(PQ);
Reviewed: 28-Mar-2022, QC No. QC No. Iphsj-22-12664;
Revised: 02-Apr-2022, Manuscript No. Iphsj-22-12664(R);
Published:
11-Apr-2022, DOI: 10.36648/1791-809X.16.S6.927
Abstract
Diabetes mellitus is a chronic metabolic disorder that affects blood glucose levels causing high levels of it (hyperglycemia) associated with a dysfunction in the production and action of insulin that leads to a deficiency of is thus leading to a deficit in metabolism; There are different types of diabetes that are diabetes mellitus type 1, type 2 and gestational diabetes, which are differentiated by different characteristics; This pathology presents different clinical manifestations and multiple chronic complications, which are divided into: a) macro vascular (equivalent to arteriosclerosis), b) micro vascular, which include retinopathy, nephropathy and neuropathy, and c) diabetic foot, which manifests itself in consequence of neuropathy or vascular affection of macroangiopathic origin, which can lead to affecting several systems of the organism such as the musculoskeletal system.
Keywords
Diabetes mellitus, Neuropathy, Neuromuscular complications, Diabetic foot, Neuropathic pain, Deformities
Introduction
Diabetes mellitus is a chronic metabolic disorder that affects blood glucose levels causing high levels of it (hyperglycemia) associated with a dysfunction in the production and action of insulin that leads to a deficiency of is thus leading to a deficit In the metabolism and processing of lipids, proteins and carbohydrates, three main types of type I diabetes mellitus are described, also known as insulin-dependent or juvenile diabetes caused by destruction of the pancreatic beta cell, associated in turn with an absolute deficit of insulin. which requires external administration of insulin on a daily basis, type II diabetes mellitus being the most frequent, given by high levels of glucose in the blood secondary to a resistance to the action of insulin in the beta cells of the pancreas accompanied by a deficient production of insulin by the pancreas and gestational diabetes named after high levels of glucose a in blood that appears during pregnancy and that was not previously diagnosed, this usually resolves after childbirth, and it is common for type diabetes to appear 2 years later, the origin and Etiology of diabetes can be multiple, however, they entail unquestionably to the existence of alterations in the secretion and action of insulin, sensitivity to the action of the hormone, or both at some point in the disease [1].
In those cases in which the symptoms are marked, evident and persistent, accompanied by sufficiently high blood glucose levels, the diagnosis is obvious in most cases. However, we must not forget that, in many cases, the diagnosis is made in patients asymptomatic and through a routine analytical exploration and in many cases it is not diagnosed if not when there are already complications and alterations that affect other systems and organs, which makes the disease more evident, The chronic complications of diabetes are divided into: a) macro vascular (equivalent to arteriosclerosis), complications that generally affect the arteries, giving rise to coronary heart disease, cerebrovascular disease and peripheral vascular disease; b) micro vascular, including retinopathy, nephropathy and neuropathy, and c) diabetic foot, which manifests itself as a consequence of neuropathy or vascular affection of macroangiopathic origin, a very frequent alteration in these patients that affects their quality of life and it can lead to extreme circumstances such as limb amputation in reference to irreversible damage that evolves seriously [1-3]
Among micro vascular conditions, diabetic neuropathy is the most common of the complications caused by diabetes, it classifies a heterogeneous group of conditions that affect the nervous system and that presents various clinical manifestations that affect the quality of life of the patient, and the Diabetic neuropathy in turn is currently classified into 3 groups: Diffuse neuropathies: encompassing symmetrical distal polyneuropathies of thin, thick, and mixed fibers. Mon neuropathies: encompassing cranial or peripheral nerve mononeuropathies or mononeuritis multiplex.
Polyradiopathies or radiculopathy: which includes lumbosacral radiculopathy, proximal motor amyotrophic and thoracic radiculopathy? In turn, another group of anatomical alterations at the cardiovascular, gastrointestinal, urogenital and sudomotor dysfunction levels is described, among another range of classifications and neuropathic alterations that affect the diabetic patient but that occur to a lesser extent such as root plexus neuropathies, painful neuropathy acute smallfiber neuropathies, usually induced by treatment, chronic inflammatory demyelinating polyneuropathy and compressive neuropathies
Likewise, due to this complication, certain deformities and anatomical alterations usually appear in the individual, prevalent in the diabetic population, such as hammer toes, claw toes, which are characterized by hyperextension of the metatarsophalangeal joint with the presence of flexion at the distal interphalangeal level. and proximal, which can be accompanied by stiffness and which in turn can evolve to retraction of the flexors and as a result, the joint becomes deformed and stiff and ankylosed, this alteration usually produces intense pain, cavus foot can also occur , equine foot, alterations at the joint level and, in general, mostly podalic deformities frequently presented in these patients, it is explained that the appearance of these bone deformities in this population arise from chronic hyperglycemia caused by the alteration at the insulin level explained above , which produces glycosylation of proteins ines found in the joints and soft tissues, resulting in stiffness and thickening of the ligaments and capsular structures, thus favouring the appearance of these deformities, it is also associated with the weakness and atrophy of these areas due to motor neuropathy [2-4].
The appearances of these deformities at the bone level are usually accompanied in turn by loss of sensitivity, pain and a marked motor deficit, in addition to this large group of complications, several studies have reported that diabetes is associated with an increase in bone density. Individuals, associated with an alteration in the formation of collagen fibers, leading to a reduction in the formation of protein extracellular matrix and mineralization, also associated with a suppression of genes related to the maturation of osteoblasts, generating a significant impact in the mortality and morbidity of diabetic patients [5-7].
High levels of advanced glycation end products (AGEs) and their accumulation play a crucial role in the development of diabetes-related complications. High levels of AGE have been found in various tissues and have been associated with low tissue turnover in tendons, skin, amyloid plaques, or cartilage. The accumulation at the bone level reduces the activity of osteoblasts, alters osteoclast genesis and reduces mineralization due to the binding of AGE products to specific receptors (RAGE). Collagen from the extracellular matrix, modified with AGE, is more difficult to remove by hydrolases, which increases bone fragility, which is why the presence of AGE interferes with the interaction between bone cells and the extracellular matrix. Therefore, excess glycosylation affects bone properties, and this effect is first evident at the cortical level, since AGEs (such as pentosidine) accumulate in sites with less bone turnover [7].
This is why it is recommended to place a high emphasis on these alterations, since neuropathy is one of the most frequent complications in diabetic patients, especially in type II, and it is necessary to carry out screening and follow-up in these same ones, since they can have an adverse effect. Serious in the living conditions of each patient, making a timely diagnosis of diabetes and adequate treatment would greatly reduce the presence of micro vascular complications such as neuropathy a posteriori, as well as the macro vascular complications that occur in these patients [6, 8].
Methodology
To carry out this article, a bibliographic search was carried out in various databases such as Elsevier, Scielo, Medline, PubMed, Science Direct and Ovid, thus selecting original articles, case reports and bibliographic reviews from 2013 to 2019, in Spanish and English. using MeSH terms: diabetic neuropathy, complications, musculoskeletal, diabetes mellitus and the Boolean operators and or. Thus including all the documents that will deal with osteomuscular complications secondary to diabetic neuropathy, the data found were between 12-28 records, thus using 21 articles for the preparation of this document.
Results
A study carried out in Mexico in a first level unit, 70 patients with type 2 DM were studied, in which the female sex predominated 70% (95% CI; 59.3-80.7), with an average age of 63.24±4.37 years (95% CI; 61.18-65.31). Of the patients studied, the predominant BMI was grade 1 obesity in 40.0% (95% CI; 28.5-51.5), followed by overweight with 30.0% (95% CI; 19.3-40.7) [9, 11].
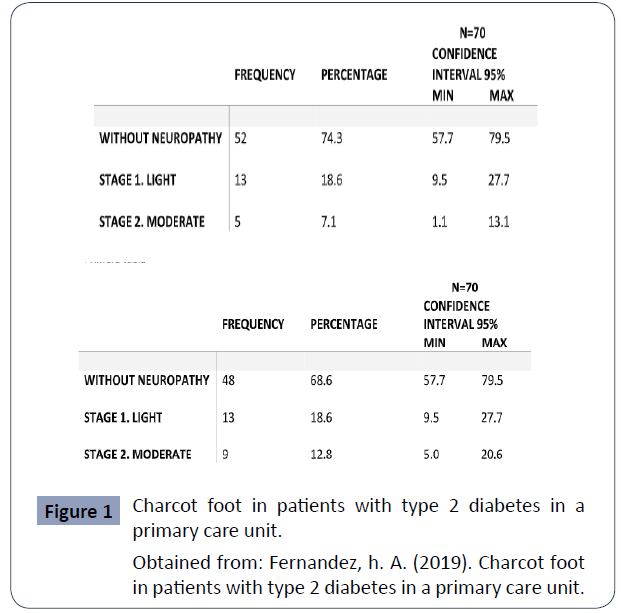
From the Michigan test, it was found that 18.6% (959.5-27.7 CI)presented mild neuropathy and 12.8% (95% CI; 5.0-20.6) were found in moderate stage [10, 11].
In 18.6% (95% CI; 9.5-27.7) of the studied patients presented slight neuropathy from the monofilament scale and 128 hz tuning fork (Figure 1).
Figure 1 Charcot foot in patients with type 2 diabetes in a primary care unit.
Obtained from: Fernandez, h. A. (2019). Charcot foot in patients with type 2 diabetes in a primary care unit.
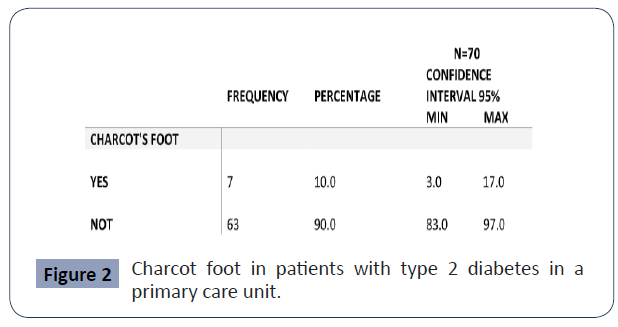
Of the 70 patients studied, 7 patients, that is, 10.0% (95% CI; 3.0-17.2) have Charcot foot. Of the patients who presented monofilament scale and tuning fork with neuropathy, 38.9% presented positive radiological study for Charcot's Foot, and 61.6% of patients with monofilament and positive tuning fork did not present evidence of Charcot's foot in the study, with a chi square of 22.4 and a significant [9-11] (Figure 2).
Figure 2 Charcot foot in patients with type 2 diabetes in a primary care unit.
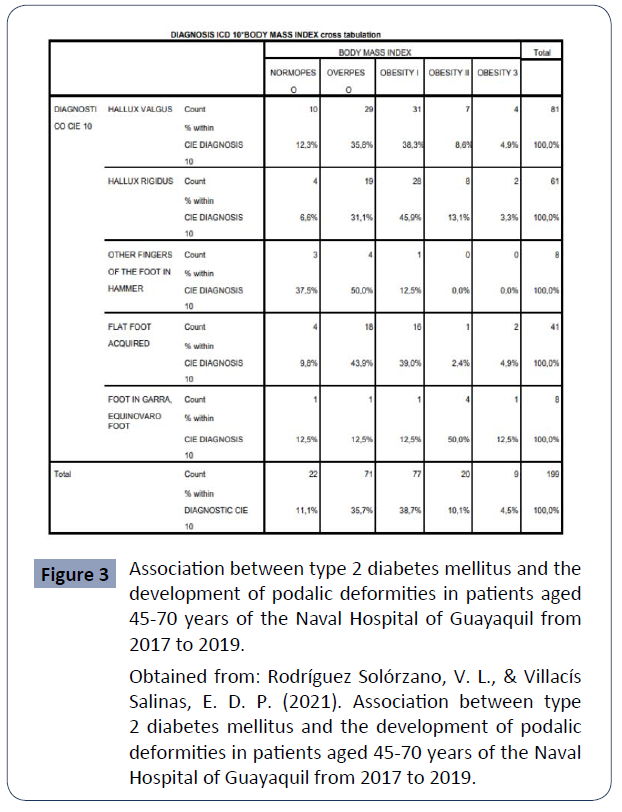
An investigation whose main focus was the determination of the foot deformities of patients with type 2 diabetes and the factors related to it, where it is evident that, when analysing the prevalence of cases according to the type of malformation developed, the most prevalent was Hallux Valgus with 40.7% of the cases (n=81), followed by Hallux Rigidus with 30.7% of the sample (n=61), making these the most frequent malformations evidenced [12].
Correlation analysis between body mass index and developed podalic deformity is performed. It is observed that, among the cases of body mass reported within the category of Overweight and Obesity Grade I, they have the highest concentration of cases of podalic deformities, especially Hallux Valgus and Hallux Rigidus. Therefore, a direct relationship between the body mass index and the development of this type of deformities is determined. (p<0.05) [13, 14].
Correlation analysis between body mass index and developed podalic deformity, the prevalence of cases was reported according to body mass index, where Grade I Obesity stood out as the most frequently reported in these patients, with 38.7% of the cases, and in turn, it was determined that there is a direct relationship with the development of deformities, especially Hallux Valgus [12,15] (Figure 3).
Figure 3 Association between type 2 diabetes mellitus and the development of podalic deformities in patients aged 45-70 years of the Naval Hospital of Guayaquil from 2017 to 2019.
Obtained from: Rodríguez Solórzano, V. L., & Villacís Salinas, E. D. P. (2021). Association between type 2 diabetes mellitus and the development of podalic
deformities in patients aged 45-70 years of the Nava Hospital of Guayaquil from 2017 to 2019.
On the other hand, carpal tunnel syndrome is a neuropathy due to entrapment of the median nerve, in its course through the channel, at the level of the wrist. It is characterized by pain and paresthesias in the area of distribution corresponding to the nerve (big finger, index finger, middle finger and the lateral half of the ring finger). It worsens at night, and sometimes radiates to the forearm; although neuropathy mainly affects the lower limbs, it can also appear in the hands. When the symptoms and signs in the hands become evident, the affectation in the feet is generally advanced [16].
“Trigger finger” has been reported in different studies. Also known as flexor tenosynovitis, it manifests as a phenomenon of blocking the flexo-extension of the finger. On physical examination, the nodule may be palpable at the base of the affected finger. In diabetics, it usually affects several fingers, among the most frequent, the first, third and fourth. The prevalence of trigger finger in subjects with diabetes varies between 5-36%, compared to the general population, which only affects 2%. It is associated with the evolution of the disease, glycaemic control and micro vascular complications [17, 18].
Discussion
Diabetes over time, given its evolution in poorly controlled patients, and adding their advanced age, becomes a risk factor for the appearance of complications such as diabetic neuropathy [19].
In the United States, Law, G. et al. (2020), determined Hallux Valgus as the most prevalent deformity in their study, corresponding to a prevalence that reached 43.2%. Likewise, Couselo, I. et al (2018), in a study carried out in Cuba, determined this deformity as the most frequent, with 48.6% of the sample.
The prevalence of cases in patients according to body mass index was reported, where Obesity Grade I stood out in results, as the most frequently reported, with 38.7% of cases, and in turn, it was determined that there is a direct relationship with the development of deformities, especially Hallux Valgus. Cardona, D. et al. (2018) in Colombia conducted a study to determine the factors associated with musculoskeletal complications in patients with Diabetes Mellitus, including foot deformities. Within his study, he reported a body mass index greater than 30 kg/m2 as the most frequent in the cases included as a sample, with 69.4% . In a group studied, glycated hemoglobin and fasting glucose prevailed in uncontrolled figures, which propitiate, from physiological changes, the development of chronic complications of DM, such is the case of diabetic foot; It would then be necessary to carry out a cohort in patients with glycated hemoglobin control, for its assessment and prevention.
In a study carried out to evaluate Charcot foot based on the Michigan test, which consists of a test and a simple physical examination of the foot, a prevalence of 31.4% of alteration was found in this test, lower than that reported in studies previous national studies in Mexico where they have found a prevalence of 69% and 60% respectively. However, it is emphasized that the Michigan test is only the beginning of the screening to determine alterations in the biomechanics of the foot, and should not be used for its diagnosis [9].
Charcot foot has a high prevalence, of 10%, in first level care units, for which emphasis should be placed on measures to detect sensory and anatomical changes in the foot, for its comprehensive treatment in a comprehensive manner. Timely and prevent its progression to physical limitation.
Conclusion
Among the micro vascular conditions of diabetes mellitus, diabetic neuropathy is the most common of the complications caused by diabetes, this condition affects the nervous system and presents various clinical manifestations that affect the quality of life of the patient, among which we can highlight in a large percentage to musculoskeletal conditions such as deformations at the foot level such as hallux valgus, charcot foot or diabetic foot that greatly affect the quality of life of patients, so an early diagnosis and management of this pathology to reduce the appearance of these complications.
REFERENCES
- Conde A, Paredes C, Castillo R (2002) NeuropatÃa diabética, Rev hosp Gral Dr M Gea Gonzalez, marz 5:1.
Google Scholar
- Pedroza H, Braver J, Rolim L, Schmid H, Calsolari M et al. (2019) neuropatia diabética 9:72.
Google Scholar
- Hodelin E, Maynard R, Hodelin H, Maynard G (2018) complicaciones cronicas de la diabetes mellitus tipo II e adultos mayores. Revista información cientÃfica junio 97.
Indexed at, Google Scholar
- Estévez A, Garcia Y, Licea M, Fundora A, Alvarez H (2013)  Identificación de las deformidades podálicas en personas con diabetes mellitus, una estrategia para prevenir amputaciones, Revista cubana de endocrinóloga junio 24.
Indexed at, Google Scholar
- Botas M, Cervell D, Rodriguez A, Vicente S, Fernandez I (2017) Actualización en el diagnóstico y tratamiento de la neuropatÃa diabética periférica, AngiologÃa mayo 69.
Indexed at, Google Scholar
- Jodar E (2017) diabetes y hueso una relación inesperada. rev osteoporos metab miner 9.
Indexed at, Google Scholar, Crossref
- Garcia M, Muñoz M (2012) diabetes mellitus tipo II y osteoporosis, rev osteoporos metab miner 4.
Google Scholar
- Samper D, Monerris M, Homs M Soler M (2010) etiologÃa y manejo de la neuropatÃa diabética dolorosa. rev soc Esp dolor Junio 17.
Indexed at, Google Scholar, Crossref
- Alvarez E, Mena K, Faget O, Conesa A, Dominguez E (2015) El pie de riesgo de acuerdo con su estratificación en pacientes con diabetes mellitus. Rev Cubana Endocrinol 26:2.
Indexed at, Google Scholar
- Fernandez h A (2019) Pie de charcot en los pacientes con diabetes tipo 2 de una unidad de primer nivel de atención.
Google Scholar
- Fernández IC, Prieto JMR (2018) Riesgo de pie diabético y déficit de autocuidados en pacientes con Diabetes Mellitus Tipo 2. EnfermerÃa Universitaria Marzo 15.
Google Scholar
- Garbey DLC, Despaigne LV, Cardona JCC, Ãlvarez EZ, Salvá AR (2018) Pie de riesgo en personas con diabetes mellitus de tipo 2 en la Atención Primaria de Salud durante Medisan 21.
Google Scholar
- Wagner Hirschfield Emilio WHP (2016) Hallux valgus en el adulto: conceptos actuales y revisión del tema. Revista Chilena de Ortopedia y TraumatologÃa 57.
Indexed at, Google Scholar, Crossref
- Pandey A, Usman K, Reddy H, Gutch M, Jain N, et al. (2013) Prevalence of hand disorders in type 2 diabetes mellitus and its correlation with microvascular complications. Ann Med Health Sci Res 3:349-354.
Indexed at, Google Scholar, Crossref
- Ulrich Illgner U, Netten J, Droste C, Meiners T, Postema K et al. (2014) Diabetic Charcot Neuroarthropathy of the Hand: Clinical Course, Diagnosis, and Treatment Options. Diabetes Care 37:e91-e92.
Indexed at, Google Scholar, Crossref
- Bus SA, Lavery LA, Monteiroâ?Soares M, Rasmussen A, Raspovic A et al. (2020) International Working Group on the Diabetic Foot. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev 36:e3269.
Indexed at, Google Scholar, Crossref
- Holleman F (2014) Acute and chronic complications of diabetes. Diapedia 31:9.
Google Scholar, Crossref
- Gin Way Law, Zhang KT, Yeo NEM, Koo K, Rikhraj IS (2020) Results of Hallux Valgus Surgery in Diabetic Patients With Good Glycemic Control. FAI 41:945-953.
Indexed at, Google Scholar, Crossref
- Garbey DLC, Despaigne LV, Cardona JCC, Ãlvarez EZ, Salvá AR (2018) Pie de riesgo en personas con diabetes mellitus de tipo 2 en la Atención Primaria de. Salud durante Medisan 21.
Google Scholar
Citation: Citation: De La Peña Restrepo LE, González Walles J, Jurado Escobar PL, Pérez Cabra O, Villegas Lora JF, et al. (2022) Main Musculoskeletal Complications Secondary to Diabetic Neuropathy. Health Sci J. Vol. 16 No. S6: 927.