Luciana Fortes Tosto Dias1,2*, Rogerio Luiz de Araujo Vian2,3, Pedro Miguel Nunes2,3, Henrique Esteves Magalhaes2,4, Claudiane da Silva Maia do Carmo,2,5,6, Eduardo Costa Figueiredo Passos2and Luciano Rodrigues Neves2,8
1Unorp, University Center North Paulista, Sao Jose do Rio Preto, SP, Brazil
2Unipos, Post graduate and Continuing Education, Street Ipiranga, 3460, Sao Jose do Rio Preto SP, Brazil
3Santa Casa Hospital, Bucomaxillo Facial Traumatology Center, Ribeirso Preto/SP, Brazil
4Sorridente Clinic, Monte Carmelo/Coromandel/Catalao, Brazil
5IMMNES, Implantology Center, Macapa/AP, Brazil
6GOE, Minor Oral-Macapa/AP, Brazil
7Medical School of Ribeirao Preto, FMRP-USP, Sao Paulo, Brazil
8Cano Neves Dentistry Clinic, Palmital/SP, Brazil
- *Corresponding Author:
- Luciana Fortes Tosto Dias
Unorp/Unipos, Post graduate and Continuing Education
Street Ipiranga, Sao Jose do Rio Preto SP
Brazil
Tel: +55 (17) 988037459
E-mail: m.zotarelli@gmail.com
Received date: 01 May 2019 Accepted date: 14 May 2019 Published date: 21 May 2019
Citation: Dias LFT, Vian RLA, Nunes PM, Magalhaes HE, Carmo CSM, et al. (2019) Major Considerations on the Clinical, Epidemiological, Histopathological and Therapeutic Aspects of Ameloblastomas: A Systematic Review. Health Sci J Vol.13.No.3:655. DOI: 10.36648/1791-809X.1000655
Copyright: © 2019 Dias LFT, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Keywords
Ameloblastoma; Clinical aspects; Epidemiology; Histopathology; Odontogenic tumour
Introduction
Ameloblastoma is a benign epithelial tumor of odontogenic origin being one of the most frequent [1-4]. First described in 1868 by Broca, from the beginning, it aroused a great controversy about its origin and synonymy.
This neoplasm initially received the name of adamandine epithelioma, proposed by Broca, due to its probable odontogenic etiology [5,6]. From the earliest reports, ameloblastoma was synonymous with the following terms: adamantine epithelioma, basal cell tumor, adamantinoma, epithelial odontoma, adamantinoblastoma, adamantine cystadenoma, epithelial adamantinoma, and carcinoma of dental germ residues [5].
Currently, the most widely used and accepted name is ameloblastoma, according to the World Health Organization (WHO) [3,4]. Ameloblastoma accounts for 10% to 30% of all odontogenic tumors [1]. Although benign histologically, it has infiltrative growth with a high local destruction power, which requires more careful and often radical therapeutic intervention [7].
Due to its incidence and its clinical behavior, ameloblastoma has been attracting interest from health researchers and clinicians. Thus, this study aimed to carry out a review of the literature, from 2003 to 2019 on the origin, epidemiology, clinical characteristics, imaging, histopathological and ameloblastoma treatment.
Methods
Eligibility and study design
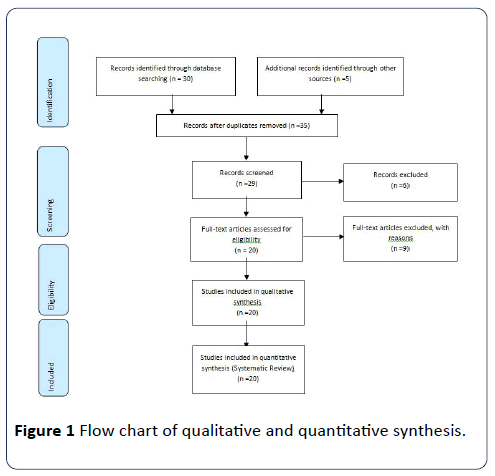
Following literary search criteria with the use of the MeSH Terms that were cited in the item on "Search strategies", a total of 35 clinical studies that were submitted to the eligibility analysis were checked, and after that, 20 studies were selected, following the rules of systematic review-PRISMA (Transparent reporting of systematic reviews and meta-analysis-https:// www.prisma-statement.org/). Studies from 2003 to 2019 were analyzed.
Search strategy and information sources
The search strategy was performed in PubMed, Embase, Ovid and Cochrane Library, Web of Science, ScienceDirect Journals (Elsevier), Scopus (Elsevier), OneFile (Gale) followed the following steps: search for mesh terms: Ameloblastoma, Clinical aspects, Epidemiology, Histopathology, Odontogenic tumor and use of boolean "and" between mesh terms and "or" among historical findings. All references are registered in EndNote (Figure 1).
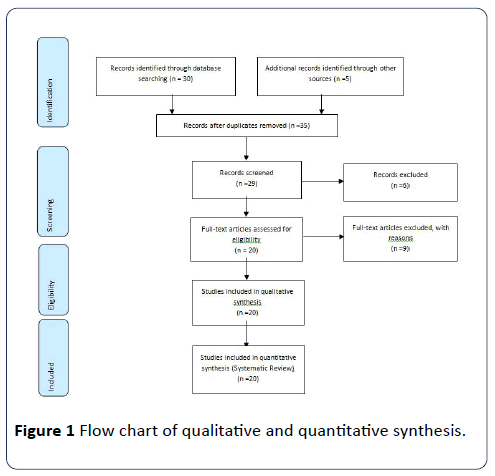
Figure 1: Flow chart of qualitative and quantitative synthesis.
Literature Review-Major Findings
The ameloblastoma is a tissue tumor of the enamel organ, which does not differentiate to the point of forming enamel, benign and of ectodermal origin [1,2]. Clinical behavior may be considered between benign and malignant, slow but persistent growth, and infiltration in adjacent tissues are some features of this tumor [3].
As to its origin, it is sought to explain the genesis of ameloblastoma from remnants of the dental blade of the enamel and sheath of Hertwig, from the epithelium of the enamel organ, from the epithelium of odontogenic cysts, mainly the dentiger, from basal cells of the epithelium of the buccal mucosa that, by invagination or ectopia, remain inside the bone [4].
According to its clinical characteristics, ameloblastoma corresponds to 1% of the tumors and cysts present in the jaw region [4-7]. The region of greatest incidence of this type of tumor is in the mandible, usually in the posterior region (molar region) and ascending branch, during the third and fourth decades of life [8]. Regarding gender, the literature is controversial, with no consensus on predominance in women or men [9,10].
Ameloblastoma is divided into three clinical types: multicystic, unicystic and peripheral [11]. Being the prevalence of multicystic, representing 85% of the cases, which may have an invasive action, with a high rate of recurrence if the treatment is not correct [9]. The unicístico represents 14% of the cases, possessing a low rate of relapse. The peripheral-type is the rarest, representing 1% of the cases, and occurs only in the region of soft tissues around the teeth [7,12-18].
Ameloblastomas are divided into three biological variants: cystic, solid and peripheral. The cystic variant is biologically less aggressive and has a better response than the solid and peripheral variants [10,19].
The evolution of ameloblastoma is very slow, and its initial diagnosis is difficult [12]. Small lesions of these tumors in the early stage are usually diagnosed by clinical radiographs. The phase in which the patient and the professional perceive the tumor usually is a more advanced stage, where edema and volume increase occurs, with facial asymmetry, which may already be in an advanced stage. Generally, paresthesias and pain are rarely reported, making it even more difficult to diagnose the tumor [13].
As for the radiographic characteristics, the majority of ameloblastomas may present radiographically multiocular or uniocular types with cortical expansion [14]. Most often, they present radiolucent multicystic lesions, forming patterns known as 'honeycomb' when the loculations are small or 'soap bubbles' when large [15]. Uniocular radiolucent lesions usually appear around the crown of an included tooth and may be confused with dentigerous cysts. They may present a root resorption area, mainly in the lower molar region [16].
Histologically, five types of ameloblastomas are described: follicular, plexiform, acanthomatous, basal cells and granulosa cells [17]. The follicular and plexiform variants are the most observed. In the first, the epithelial islets are dispersed in the conjunctive stroma of variable density, constituted by palisadearranged columnar cells [17]. In the second, uniform, branched stromal strands are observed. Frequently, the follicular and plexiform types are found in cords in the same tumor. Changes in the basic structure of the tumor, such as squamous metaplasia or the presence of granular cells, can be found [17].
The most frequently encountered histological patterns are follicular and plexiform. The follicular ameloblastoma presents islands of tumor cells (similar to the normal dental follicle), immersed in the stroma of fibrous connective tissue. In the plexiform, the odontogenic epithelium is arranged in long strands that seem to involve the stroma. These cords present cells with reverse polarization involving cells similar to the starry lattice [18].
In a study conducted by Anjos et al. [9] in 2003 41 cases of solid ameloblastoma were evaluated. The histological patterns were plexiform in 13 cases (31.71%), follicular in seven (17.07%), desmoplastic in four (9.75%), acanthomatous, basal cells and granulosa cells in one case (2.44%), two histological patterns were observed in 14 cases (34.14%). In the 20-year age group, there were 8 cases, in the age group of 20 to 50, there were 26 cases and 13 cases over 50 years.
In the follicular type, it is possible to notice the presence of islands or sheets of epithelial cells that exhibit similar morphology to the pre-ameloblasts when located in the periphery. When these epithelial structures are arranged in anastomosed cords, the term used to denote them is plexiform ameloblastoma. The presence of abundant squamous areas defines the acanthomatous type, while lesions similar to basal cell carcinoma of the skin are termed basal cell ameloblastoma [13].
The radiographic differential diagnosis of ameloblastoma includes fibrous dysplasia in its radiolucent phase, central giant cell lesion, myxoma, odontoma, dentigerous cyst, keratocyst and brown tumor lesions of hyperparathyroidism [19].
In cases where ameloblastoma involves a retained or impacted tooth, the differential diagnosis of the neoplasm is made with the dentigerous cyst. The diagnosis of ameloblastoma is given based on anamnesis, physical and radiographic examinations, and biopsy. To obtain the final diagnosis, incisional biopsy is performed, followed by histopathological examination of the specimen [20].
Multilocular ameloblastomas have higher relapse rates than unilocular ones. Therefore, the true margin of the tumor often extends beyond the apparent clinical or radiographic margin [2]. The attempt to remove the tumor by curettage may leave small islands of the tumor in the bone, which later manifest as recurrences [15].
The best form of treatment is controversial. For Santos et al. [16], ameloblastoma tends to infiltrate bone trabeculae from the bone at the periphery of the lesion before bone resorption becomes evident radiographically, causing patients to be treated for various recurrences.
The treatment of ameloblastoma can be conservative or radical. The conservative form varies from simple curettage, followed by cryotherapy [6]. The latter is a method that is employed only in some cases in small lesions, with intact mandibular base, and in patients who can be followed for long periods of time. Radical surgical treatment involves total removal of the lesion, with a safety margin that often results in the amputation of part of the patient's mandible (hemimandibulectomy). The attempt to remove the tumor by curettage can, unfortunately, leave small islands of the tumor in the bone, which later manifest as recurrences [14].
According to Fernandes et al. [5], cases of curettage treatment lead to early recurrences, since it removes only part of the neoplasia and also induces the implantation of neoplastic cells in other areas. According to the authors, all the cases of ameloblastoma submitted to curettage redicivated in the period of 1 to 15 years. Of the cases of partial mandibulectomy, four relapsed in the period of 3 to 15 years. Of the cases submitted to hemimandibulectomy, one case recurred 24 years after surgery.
For Santos et al. [16], radical surgical treatment is the therapy chosen for all types of ameloblastomas. Even in the more advanced stages of this disease, technological resources and new techniques of craniofacial surgery, allow the radical surgical treatment with a great probability of cure. Conservative surgical treatment (curettage and enucleations) should be avoided even in the early stages or in unicystic ameloblastomas. Radiotherapy can only be used when combined with surgery for lesions with severe soft tissue involvement and is contraindicated when there is a possibility of osteoradionecrosis and malignant transformation.
As described by Saddy [10], the choice of appropriate treatment, due to the aggressive and relapsing potential of ameloblastomas, is very complex, with the use of very radical therapies. However, the recurrence rate verified by this author did not present a significant difference in relation to the type of treatment. This observed that, in patients treated with resection, the recurrence was 27.3%; treated with curettage was 25%, and cryotherapy 29.7%. In relation to limits, there was a higher rate of relapse in infiltrative ameloblastomas (57.1%).
According to Nakamura et al. [17], conservative treatment, such as marsupialization and enucleation, followed by adequate bone curettage, proved to be quite efficient, reducing the need for surgical resection and reinforcing the indication of conservative treatments for ameloblastomas.
Fernandes et al. [5] evaluated the treatment performed in 12 patients of the Buccomaxillofacial Surgery Service of Hupe/Uerj between 1990 and 1997. Ten ameloblastomas of the multicystic type and 2 of the unicystic type were diagnosed. Multicystic were treated by curettage (2 cases), marginal resection (6 cases) and segmental resection (2 cases) and unicystic type submitted to curettage treatment. Only 2 cases of multicystic ameloblastoma treated with curettage presented recurrences. It has been concluded that curettage, although effective in the treatment of unicystic ameloblastomas, is not efficient in the treatment of multicystic ameloblastomas.
Martins et al. [6] carried out a study on the results of the treatment of solid ameloblastomas with the cryosurgery technique with liquid nitrogen spray, which minimizes the relapsing effects of this tumor. Thirty-six patients from the Department of Stomatology of the Hospital of Cancer A. C. Camargo, in São Paulo, with a mean age of 31 years, were evaluated for a period of 20 years. During this period, patients performed routine exams such as radiographic examination. In 30.6% of them, there were recurrences ranging from 14 months to 10 years after the initial treatment. It is concluded that cryosurgery can reduce the recurrence of solid ameloblastomas and the initial indication of resection.
Discussion
In the present literature review study and according to the articles evaluated, there were no controversies regarding the clinical, epidemiological, histopathological and therapeutic aspects of ameloblastoma.
It was observed that clinically, ameloblastoma corresponds to 1% of the tumors and cysts present in the jaw region [1-3]. The region of greatest incidence of this type of tumor is in the mandible, usually in the posterior region (molar region) and ascending branch, during the third and fourth decades of life [7]. Regarding gender, in the literature consulted, there is no consensus on the predominance of women or men [9,10,18].
The evaluated articles showed that ameloblastoma is divided into three biological variants: cystic, solid and peripheral. Its evolution is very slow, and its initial diagnosis is difficult [11,19]. Regarding the radiographic characteristics, the review of the literature performed in this study found that ameloblastomas can present radiographically multiocular or uniocular types with cortical expansion. Most often, they present radiolucent multicystic lesions, forming patterns known as 'honeycomb' when the loculations are small or 'soap bubbles' when large. Single uniocular radiolucent lesions usually appear around the crown of an included tooth and may be confused with dentigerous cysts [6].
As to its origin, the literature reviewed in this work, showed a great variety of suggestions, but Neville and collaborators in 2009 [7] seek to explain in a simple and clear way the genesis of ameloblastoma from remnants of the dental blade of the enamel and sheath organ-from the epithelium of the enamel organ, from the epithelium of odontogenic cysts, mainly the dentiger, from basal cells of the buccal mucosa epithelium which, by invagination or ectopia, remain inside the bone.
The histological characteristics describe the presence of five types of ameloblastomas: follicular, plexiform, acanthomatous, basal cells and granulosa cells, a fact that coincides in several texts reviewed in this study [6,7,9,10].
It was noted that histological variants of follicular and plexiform type are the most observed in cases of ameloblastoma [12,20]. In the follicular type, the epithelial islets are dispersed in the connective stroma of variable density, constituted by palisade arranged columnar cells [13]. Already the plexiform form, the cellular cords are uniform and branched in the stroma. In some texts, citations were found on modifications of the basic structure of the tumor, such as squamous metaplasia or the presence of granular cells [13].
In the present review, we identified the presence of squamous areas when described the histopathological characteristics of ameloblastomas, which is typified as acanthomatous, while lesions similar to basal cell carcinoma of the skin are called basal cell ameloblastoma [13].
As for the treatment form of ameloblastoma, the present review found controversy among the authors studied [14]. As ameloblastoma tends to infiltrate the bone trabeculae of the spongy bone at the periphery of the lesion, before bone resorption becomes evident radiographically, these should be treated in several ways [15,16].
As for the mode of treatment of ameloblastoma, it may be conservative or radical. The conservative form varies from simple curettage followed by cryotherapy [17]. The latter is a method that is employed only in some cases in small lesions, with intact mandibular base, and in patients who can be followed for long periods of time. Radical surgical treatment, however, implies the total removal of the lesion, with a margin of safety that often results in the amputation of part of the patient's jaw. The attempt to remove the tumor by curettage may leave small islands of the tumor in the bone, which later manifest as recurrences [17].
It was evident in the present review that the incidence, aggressive clinical behavior, high relapse rate, sometimes mutilating surgical treatment, the various histological types and the possibility of malignization of ameloblastoma have already been much discussed and well presented in the reviewed literature in present work. Being explicit that the dentist is able to easily diagnose ameloblastoma, so that he can trace his treatment and prognosis.
Conclusion
Ameloblastoma is a tissue tumor of the enamel organ, benign and of ectodermal origin and corresponds to 1% of the tumors and cysts present in the region of the jaws. The region of greatest incidence of this type of tumor is in the mandible, usually in the posterior region (molar region) and ascending branch. The highest incidence during the third and fourth decades of life. There is no prevalence of sex. It is divided into three clinical types: multicystic, unicystic and peripheral, being the prevalence of multicystic, representing 85% of the cases. They may present multiocular or uniocular types. Histologically, five types of ameloblastomas are described: follicular, plexiform, acanthomatous, basal cells and granulosa cells; follicular and plexiform variants are the most observed. The treatment of ameloblastoma can be conservative or radical. Treatment with curettage leads to early recurrences. Radical surgical treatment is the therapy chosen for all types of ameloblastomas.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgement
We appreciate greatly the UNIPOS graduate for support and also UNORP of Sao Jose do Rio Preto/SP for the support.
24487
References
- Singh R, Gupta M, Chatterjee S, Arora KS (2019) Hybrid ameloblastoma: a mystified histopathological entity. BMJ Case Rep12: e229834.
- Kosanwat T, Poomsawat S, Juengsomjit R (2019) Ameloblastic carcinoma ex ameloblastoma of the maxilla. J Oral Maxillofac Pathol 23: 58-62.
- McLean-Holden AC, Bishop JA, Kessler HP, Myers LL, Radwan AM, et al. (2019) Spindle-cell variant of ameloblastic carcinoma: a report of 3 cases and demonstration of epithelial-mesenchymal transition in tumor progression. Oral Surg Oral Med Oral Pathol Oral Radiol 12: S2212-4403.
- Oh KY, Cho SD, Yoon HJ, Lee JI, Ahn SH, et al. (2019) High prevalence of BRAF V600E mutations in Korean patients with ameloblastoma: Clinicopathological significance and correlation with epithelial-mesenchymal transition. J Oral Pathol Med 19: 1-10.
- Fernandes KPS, Bussadori SK, Martins MAT, Rosa et al. (2007) Ameloblastoma: Revisao de literature. Rev Con Saude, Sao Paulo Scientific Information System 6: 269-278.
- D’Agostino A, Fior A, Pacino GA, Bedogni A, Santis D, et al. (2003) Retrospective evaluation on the surgical treatment of jaw bones ameloblastic lesions. Experience with 20 clinical cases. Minerva stomatologica 50: 1-7.
- Neville BW (2009) Patologia Oral e Maxilofacial. Rio de Janeiro: Elsevier.
- Medeiros M (2008) Ameloblastoma of the anterior mandible. Rev Bras Otorrinolaringol 74: 478.
- Anjos ED (2003) Clinical-pathological study of ameloblastomas: case analysis. Rev Bras Odontol 60: 224-228.
- Saddy MS (2003) Retrospective study of the radiographic aspects of ameloblastoma. Disseration [Master Thesis]. Sao Paulo: Faculdade de Odontologia USP.
- Ramesh RS (2010) Unicystic ameloblastoma of the mandible, Head Neck Oncol 2: 1.
- Gomes CC (2010) Current concepts of ameloblastoma pathogenesis. J Oral Pathol Med 39: 585-591.
- Junior OAR (2007) Ameloblastoma: Review of literature. Rev. Con Saude, Sao Paulo 6: 269-278.
- Pozo AJ (2006) Unicystic ameloblastoma, bases of conservative treatment. Presentation of a clinical case and update of the bibliography.
- Santos LM, Lima JRS, Morais LC (2003) Ameloblastoma - literature review and case report. BCI. Rev Bras CirurImplant, Porto Alegre 7: 18-21.
- Nakamura N (2003) Comparison of long-term results between different approaches to ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93: 13-20.
- Pereira FAC (2010) Clinical and demographic characteristics of ameloblastomas in a population of Bahia, Brazil. Rev Odonto Cienc 3: 250-255.
- Vasconcellos RH (2008) Ameloblastoma em mandíbula. Rev Bras Otorrinolaringol 3: 478.
- Costa KD (2004) Ameloblastoma of the mandible: Report of two cases. Rev Radiol Bras 37: 465-468.