Keywords
Biological agents; Disinfection; Emergency relief
Introduction
In Brazil, mobile prehospital care, called Mobile Emergency Care Service (MECS), was standardized from 2003. This service aims to provide relief to people in urgent situations, transporting the victim to a health service. health integrated with SUS to a location closer to prehospital care, thus ensuring primary care [1]. By locomotion or removal of patients in ambulances, it may assist in the spread of microorganisms and even contamination of them, since in ambulances can be found contact points of microorganisms on inanimate surfaces on mattresses, doorknobs, bars, hands and ceilings [2]. Currently, the control of infectious diseases has become increasingly difficult due to the evolution of microorganisms [2]. Different microorganisms like bacteria, fungi, and viruses cause these infections. The group of pathogens that stands out is the bacteria that constitute the human flora and that normally do not cause risks to the healthy individual, related to their low virulence. However, in individuals with the compromised clinical picture, these microorganisms may bring some harm to their health [3]. To control microorganisms on inanimate surfaces, disinfection is recommended through the use of antiseptic solutions such as: 70% ethyl alcohol, with or without 2% glycerin; formic aldehyde and soap in 1% to 10% solution; 10% PVPI detergent solution (1% active iodine); 4% chlorhexidine detergent solution with 4% ethyl alcohol; 0.5 or 1% iodinated alcohol solution (70% ethyl alcohol, with or without 2% glycerin); and 0.5% sodium hypochlorite solution or Dakin solution [4]. Moriyta [4] defines disinfection as a process by which pathogenic germs are particularly destroyed and/or inactivated their toxin or inhibit their development. For Barbin Filho [5] disinfection is the process applied to inert surfaces, eliminating pathogenic bioagents in vegetative form, but not guaranteeing the total elimination of bacterial spores. No studies were found in the literature assessing the amount of microbial contamination before and after disinfection on the surface of mattresses, door handles, hand bars, and ambulance ceilings. Thus, it was decided to perform microbiological evaluation of these inanimate surfaces through the following objectives: To evaluate the microbiological conditions before and after the disinfection of mattresses, hand bars, doorknobs and ceilings in ambulances of the mobile emergency care service of the municipality of Fernandópolis/ SP, to classify the frequency of positive and negative cultures in mattresses, doorknobs, hand bars and ceilings before and after disinfection, to identify the total frequency of positivity and negativity of seeded plaques according to macroscopy performed before and after disinfection. Mattresses, door handles, hand bars, and ceilings, and to evaluate the effectiveness of the “disinfection” procedure performed by the MECS nursing team.
Materials and Methods
This is descriptive research and experimental analysis in a microbiology laboratory on microbiological conditions before and after disinfection of mattresses, door handles, hand bars and ceilings in ambulances at the Mobile Emergency Care Service (MECS) in the interior of São Paulo. The present study was conducted at the MECS de Fernandópolis headquarters and at the Microbiology Laboratory of the University Brazil - Fernandópolis Campus after the proper authorization of the Fernandópolis Municipal Health Secretary, who was also the MECS Fernandópolis Manager at the time of the study. Fernandópolis Campus Director-General.
Culture mediums
The culture media used for the experiment were Sabouraud- Dextrose Agar (ASD, OXOID®), and Bloodless Soy Tripticasein Agar (TSA, OXOID®) media, after preparation and sterilization, 20 mL of the medium is deposited on each plate. Petri dishes and incubated at 28°C for 24 hours. To prepare Soy Tripticasein Agar (TSA, OXOID®) culture medium with blood, 300 mL of this medium and 5 mL of sheep blood (0.5%) were homogenized for 30 seconds, once solidified, the media were incubated. at 28°C for a period of 24 hours to macroscopically identify the growth of contaminants in the media. The absence of colonies in these media means that they are fit for use.
Specimen collection
The collection procedure was performed three times, twice in June and once in July 2012. The collection took place before and after disinfection on surfaces of mattresses, knobs, hand bars, and ceilings. Disinfection was performed by the nursing staff. The collection was performed with sterile swabs and inoculated into a test tube containing 5 mL of saline (NaCl, 0.5%). After collection, contamination of any kind was avoided, so the material was transported to the laboratory in isothermal boxes and the material was immediately cultured. The collected specimens were cultured in Sabouraud-Dextrose Agar and Blood-free Soy Tripticasein Agar, incubated at 28°C for 24 to 72 hours, when the growth of the microorganisms was verified by the presence of colonies.
Mattress material collection
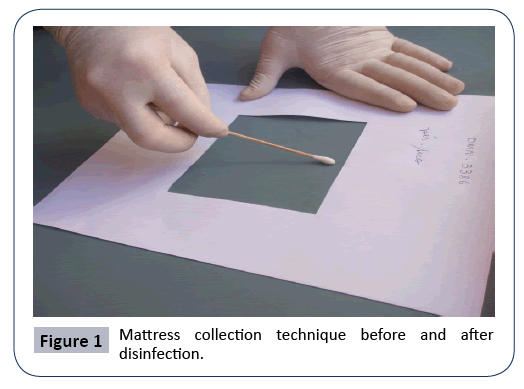
The mattresses were divided into 3 areas: headboard, middle, and feet, demarcated with quadrants measuring 100 cm2. This demarcation was placed in the ventral surface layer of the mattresses. Specimen collection was through the sterile swab by wiping right and left by rotating the swab within the quadrant, as shown in Figure 1.
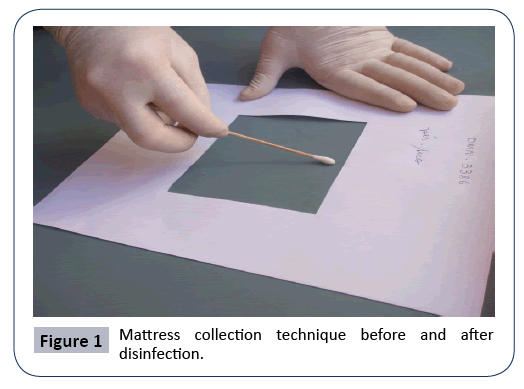
Figure 1: Mattress collection technique before and after disinfection.
Handle material collection
The samples were collected from the outer and inner surfaces, as each door has two doorknobs, one that opens on the outside and one that opens on the inside. Specimen collection was by means of a sterile swab rubbing to the right and left rotating the swab. With the swab, it allows collecting in places where disinfection does not reach, facilitating the sampling of bioagents in those places.
Hand bar material collection
The hand bars are located on the ceiling inside the ambulance. When the ambulance is moving, the bar serves as a support for professionals. Specimen collection was by means of the sterile swab rubbing to the right and left by rotating the swab covering all ends of it.
Ambulance ceiling material collection
The ceiling was divided into 3 parts: anterior, middle and posterior. Sterile swabs were used, scrubbing right and left by rotating the swab, covering the ends and places where disinfection does not reach.
Specimen growing
Specimens collected before and after disinfection were inoculated in culture medium (ASD, OXOID®) and (TSA, OXOID®) with blood and (TSA, OXOID®) without blood in Petri dishes and incubated at 28°C for 24 to 72 hours Blood (TSA) media were placed into an anaerobic jar and incubated at 28°C for a 24 hour period for anaerobic microorganism growth. After incubation time, the macroscopic appearance of the colonies on the surface of the Petri dishes was observed, being classified as positive/presence and negative/absence of colonies. Positive cultures were employed for the preparation of Gram staining slides for identification of bacterial types and methylene blue for identification of fungi. Bacteria identified as gram-negative bacilli were picked on methylene blue eosin agar medium, used for isolation and differentiation of Escherichia coli, other gramnegative microorganisms were also identified by biochemical tests.
“Disinfection” process performed by MECS nursing staff
In the study, the disinfection technique performed by the MECS nursing team was observed. This process is to provide the customer with security and also for healthcare professionals working in the mobile unit. This method aims to reduce pathogenic bioagents by taking into account the mechanical and chemical action, being essential elements for the disinfection procedure. The MECS nursing team performs two types of cleaning: the “competitor” that is performed after customer service, being performed daily and in some parts of the mobile unit and some equipment after its use and also the “terminal” cleaning that is performed on weekends, cleaning all mobile unit components and equipment. The application method is simple and fast, being performed by mechanical action, that is, by manual friction associated with the detergent-disinfectant solution and finally, 70% alcohol is used. These two types of cleaning are performed to remove dirt, with the primary purpose of preventing the spread of pathogenic bioagents that colonize the surfaces of materials and equipment of the mobile unit.
Results
The research was conducted on 2 mattresses, 8 door handles, 2 hand bars and 2 ceilings. Sowing and development of pathogenic bioagents in the plates allowed comparisons to be made before and after disinfection regarding the positivity and total negativity of Petri dishes; frequency classification of positive and negative cultures and also the evaluation of the effectiveness of disinfection performed by the MECS team. In the study, the bacteria identified with gram stain were: gram-positive bacilli, gram-negative bacilli, and Bacilli genera, Pseudômonas sp. Escherichia coli, Clostridium sp, Micrococcus sp, Staphylococcus sp, Streptococcus sp. The identified fungi were: Arpergillus flavus, Aspergillus niger, Epidermophyton sp, Candida sp, Penicillium sp, Trichophyton rubrum.
Frequency of positive and negative cultures
540 seeded plates were used, (270 plates were used before disinfection and 270 plates after disinfection). To standardize the reading of the plates, the following names were established: absent/negative colonies (AC): plaque without colony growth and present/positive colonies (PC): plaque with colony growth of the 540 plates sown with specimens collected from mattresses, doorknobs, hand bars and roofs, 130 plates (24.07%) resulted in no colonies, i.e. negative cultures and 410 plates (75.93%) resulted in presence of colonies in positive cultures. Of the total negative cultures (24.07%), 7.03% corresponded before disinfection and 17.04% corresponded to the collection after disinfection. Of the total positive cultures (75.93%), 42.97% corresponded to samples obtained before disinfection and 32.96% after disinfection (Table 1). In the analysis on post-disinfection sampling, there was a reduction in only 17.04% of the cultures, which is a worrying result, since disinfection must be effective in its action, thus ensuring infection control for clients using the product mobile health care service.
Table 1 Total frequency of positive and negative cultures before and after disinfection of which: absent/negative colonies (AC); and present/positive colonies (PC).
| Before |
After |
Total |
| PC |
AC |
PC |
AC |
PC |
AC |
| 232 |
38 |
178 |
92 |
410 |
130 |
| 42.97% |
7.03% |
32.96% |
17.04% |
75.93% |
24.07% |
From the 2 mattresses materials were harvested which were sown on (108 plates), 8 door handles (288 plates), 2 hand bars (36 plates) and 2 roofs (108 plates) a total of 540 plates were examined before and after disinfection. Table 2 shows that 270 plaques sown before disinfection resulted in 42.97% in the presence of colonies and 7.03% in the absence of colonies. The other 270 plaques performed after disinfection resulted in 32.96% in the presence of colonies and 17.04% in the absence of colonies (Table 2).
Table 2 Frequency of positive and negative cultures on mattresses, door handles, bars and ceilings before and after disinfection of which: absent/negative colonies (AC); and present/positive colonies (PC).
| Mattresses |
Doorknobs |
Bar |
Ceilings |
Total |
|
| Before |
After |
Before |
After |
Before |
After |
Before |
After |
Before |
After |
|
| PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
| 37 |
17 |
31 |
23 |
128 |
16 |
94 |
50 |
17 |
1 |
13 |
5 |
50 |
4 |
40 |
14 |
232 |
38 |
178 |
92 |
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
42,97% |
7,03% |
32,96% |
17,04% |
The effectiveness of the disinfection procedure on mattresses, door handles, hand bars and ceilings was made possible by macroscopic comparison of Petri dishes. For disinfection, 270 plates were harvested on 2 mattresses (54 plates), 8 door handles (144 plates), 2 hand bars (18 plates) and 2 ceilings (54 plates). In the mattresses were found 23 plates without colonies and 31 plates with presence of colonies, while in the knobs 50 plates without colonies and 94 plates with presence of colonies, in the hand bars were 5 plates without colonies and 13 plates. Presence of colonies and on the roofs, 14 colony-free plates and 40 colony-presence plates were found. The absence of colonies prior to disinfection can be explained due to concurrent cleaning performed by the nursing staff. This cleaning is performed daily, after customer service, and is performed on some parts of the mobile unit and some equipment after use (Table 3).
Table 3 Full identification of the frequency of colonies present and absent in ASD, TSA without blood and TSA with blood media performed before and after disinfection of which: absent/negative colonies (AC); and present/positive colonies (PC).
| Medium TSA |
Medium ASD |
Medium TSA with Blood |
Total |
| Before |
After |
Before |
After |
Before |
After |
Before |
After |
| PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
PC |
AC |
| 86 |
4 |
85 |
5 |
59 |
31 |
9 |
81 |
87 |
3 |
84 |
6 |
232 |
38 |
178 |
92 |
Discussion
The study provides important contributions regarding disinfection of mattresses, door handles, hand bars, ambulance ceilings in which the microbial load was characterized before and after disinfection. After colony growth, the number of positive plaques after disinfection was of concern. The presence of colonies was 65.92% showing that disinfection was inefficient to eliminate the microorganisms, although manual, the antiseptic “70% ethyl alcohol” was used. This antiseptic acts on a variety of pathogenic bioagents and are recommended in all healthcare settings. Negative signs 14.07% before disinfection can be explained by the periodic performance of concurrent cleaning, it is performed after customer care, cleaning only the materials and equipment used in pre-hospital care. The 85.93% of positive cultures before disinfection represents a worrying number, this percentage should be lower due to the concurrent cleaning performed daily. This comparison also shows that concurrent cleaning was not effective inhibition of pathogenic bioagents proliferation after the visits. Andrade, et al. [6] conducted a study on microbiological evaluation in hospital mattresses before and after their infection. In this study, 52 mattresses were investigated, totaling 520 plates, of which 514 (98.8%) resulted in positive cultures, of which 259 corresponded before cleaning and 255 after cleaning, with only a reduction of positive cultures in 4 plates. Scott and Bloomfield [7] performed a comparison of cleaning on the efficiency of disinfectants in different domestic environments with soap and water and the application of phenolic disinfectants and hypochlorite. The results indicated the inefficiency of the nonrinse soap and water mixture in relation to the other products under the same conditions. The application of disinfectants, hypochlorite, and phenolic produced an increase of clean sites to 38% and 76%. Chemicals found in markets may offer better resources to health professionals, but it brings insecurity about which product is the most suitable. There are many guidelines in the literature, becoming conflicting between one choice and another. For when choosing the product is extremely important to analyze what would be the other factors that would be contributing to the reduction of pathogenic bioagents after terminal cleaning of mattresses. Consideration should also be given to how the cleaning procedure should be performed, as it can be foreseen that several factors may interfere with its final result [6]. Bloomfield and Scott [8] cite several studies that show the inefficiency of the cleaning procedure with only soap and water without proper rinsing in running water. The authors explain that decontamination thorough cleaning by mechanical action, that is, only by friction in soap and water, will be effective if rigorously applied in conjunction with a rinsing process. The same authors found that after 90 to 180 minutes, many of the sites became recontaminated, for this reason, they were attributed to the type of cloth used for cleaning, as excess moisture makes the material soaked, or also the poor choice of chemical. Resulting in reduced microbial action, not destroying species found on the surface. Diaz and Rojas [9] warn that all hospital surfaces should be clean and special attention should be given, as the authors explain that the force of gravity facilitates the deposition of dirt and the proliferation of bioagents. pathogenic. The presence of Escherichia coli, Staphylococcus sp, Clostridium sp, Micrococcus sp, Streptococcus sp. Pseudomonas sp and fungi such as Arpergillus flavus, Aspergillus niger, Trichophyton rubrum, Epidermophyton sp, Penicillium sp, Candida sp at the Urgent Emergency Care Service in the city of Fernandópolis serve as a warning, as the ambulance health team can carry pathogenic bioagents. to the patients attended. The presence of these pathogens in the hands of health professionals can survive for a long period of time, and these pathogenic bioagents appear to be associated with outbreaks of infection in healthcare settings [10-12]. The study was not the search for "sterility" of mattresses, door handles, hand bars, ceilings, but rather a significant decrease of microorganisms, however, however, the results of this research suggest that disinfection was not efficient in removing microorganisms. -organisms, allowing the locomotion of residual pathogenic bioagents to other points, creating the possibility of contamination of health agents and clients attended by MECS.
Conclusion
To avoid contamination of the customer at the time of transportation or transportation through the use of materials and equipment from the ambulance to the next SUS service, it is necessary to create protocols or implement new disinfection practices in the materials and equipment of the mobile unit. sensitizing health professionals to their care practice in order to reduce the transfer of pathogens between healthcare professional, client and mobile car. It is also necessary for the health professional to be aware of the actual conditions of the mechanism of action of antiseptics and disinfectants for disinfection, taking into account the nature of the material and the area to be disinfected, and may require a material and/or an area to wash and scrub before application of the disinfectant, as it may have its microbiological action diminished or inactive in the presence of antiseptics and disinfectants. But, for this event, it is necessary to work proficiently from the entire professional team, because the responsibility to prevent and control the infection rests with the entire MECS team. It is hoped that the results obtained will be able to make new decisions in health services management, in order to introduce changes in the disinfection activity, seeking to improve its technique and ensure the safety of MECS users.
25255
References
- Brazil (2006) Ministry of Health; National emergency policy. (3rded.) Brasilia; Ministry of Health.
- Lopes LHC, Alonso da Costa MFBN, Noronha KMA (2005) Nursing routines on ambulance cleaning and disinfection: a literature review. In: IX Latin American Meeting of Scientific Initiation and V Latin American Graduate Meeting, 2005, Paraíba. Annals. University of Vale do Paraíba 379-382.
- Levy CE (2003) Clinical microbiology manual for infection control in health services.
- Moriya T, Modena JLP (2008) Asepsis and antisepsis: sterilization techniques. Medicine (Ribeirão Preto) 41: 265-273.
- Barbin-Filho A (2006) Cleaning and disinfecting surfaces in health services. Infection Control Commission of SMS Ribeirão Preto-SP 6-27.
- Andrade DDE, Angerami ELS, Padovani CR (2000) Microbiological condition of hospital beds before and after cleaning. Rev Public Health 34: 163-169.
- Scott E, Bloomfield SF (1985) The bacteriological investigation of the effectiveness of cleaning and disinfection procedures for toilet hygiene. Journal Appl Bacteriol 59: 291-297.
- Bloomfield SF, Scott E (1997) Cross-contamination and infection in the domestic environment and the role of chemical disinfectants. Journal Appl Microbiol 83: 1-9.
- Diaz CAA, Rojas FJC (1996) Cleaning process in the hospital. All Hosp 126: 49-53.
- Fernandes AT, Fernandes MOV, Son NM (2000) Hospital infection and its interfaces in the Health area. São Paulo: Atheneu
- Wagenvoort JH, Sluijsman W, Penders RJ (2000) Better environmental survival of outbreak vs. sporadic MRSA isolates. Journal of Hospital Infection 45: 231-234.
- Lemmen SW, Hafner H, Zolldann D (2004) Distribution of multi-resistant Gram-negative versus Gram-positive bacteria in the hospital inanimate environment. Journal of Hospital Infection 56: 191-197.