Keywords
Total serum Homocysteine (tHcy), high density cholesterol lipoproteins (HDL-C),low density cholesterol lipoproteins (LDL-C),triglycerides (TG), paraoxonase-1 (PON1)
Introduction
Homocysteine (tHcy) is a sulfur containing aminoacid which is converted into methionine in the presence of folic acid and vitamin B12 [1].
Hcy concentration is considered to depend on genetic and environmental factors, such as nutritional habits [2].
An elevated plasma level of total homocysteine (tHcy) has long been known as an independent predictor of cardiovascular disease (CVD). However, in the absence of a clear mechanism linking tHcy to CVD, there has been an ongoing debate about whether this relationship is one of cause and effect or whether an elevated level of plasma tHcy is an epiphenomenon, reflecting the presence of some other proatherogenic factor that is actually responsible for the CVD [3].
Clinical studies of patients with coronary artery disease (CAD) reveal a negative correlation between plasma levels of Hcy and HDL-C. A prospective study evaluating survival of patients with angiographically defined CAD found increased mortality and decreased HDL-C in patients with the highest Hcy levels. Thus high Hcy predicts all-cause mortality in CAD, independent of traditional risk factors [4].
Recent studies have provided supporting data showing that plasma Hcy is negatively correlated with HDL-C levels in patients with myocardial infarction and CAD [5,6].
On the basis of the above mentioned data we measured levels of tHcy, LDL-C, HDL-C and triglycerides (TG) in the sera of adult patients of ICU in a Cardiology Department of a Hospital of Athens in order to calculate possible correlations between these parameters.
Materials and Methods
The present study was approved by the Greek Ethics Committee, according to Helsinki declaration (1989).
Blood was drown immediately after the admittance of the patients. Blood was centrifuged and kept to -20°C, in order to avoid false release of Hcy. All determinations were performed on the same day.
Determination of Hcy was performed using fluorescence polarization immunoassay (FPIA) and IMX analyzer. Sensitivity of the method was 0.50 μmol/l.
Levels of TG, HDL-C and LDL-C were measured in by using enzymic and chromatometric methods in a biochemical analyzer Olympus AG640 Medicon.
Statistical evaluation of the results was performed by using non parametric method (Mann-Whitney) and correlation factors Pearson were evaluated for all parameters measured.
Results
a. Descriptives
94 patients (51 men, 43 women) 48- 66 years aged took part in our study. All patients a sample population from the Greater Metropolitan area of Athens, suffered from acute cardiovascular events were admitted to the Intensive Care Unit (ICU), Cardiology Department , Sotiria Hospital of Athens.
b. Statistics
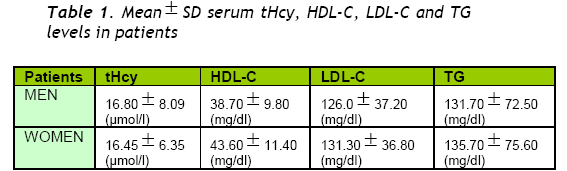
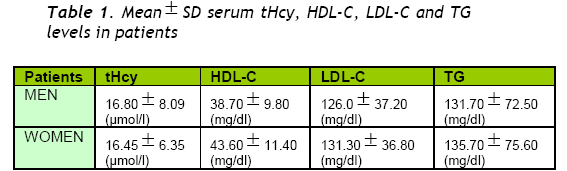
Mean value of tHcy was 16.65+7.55 μmol/l well above the normal range of 9.9- 10.6 μmol/l given in bibliography [7,8]. Mean value of tHcy for men was 16.8+8.09 μmol/l and for women 16.45+6.35μmol/l.
Mean value of HDL-C was 40.9+10.78 mg/dl in all patients (38.7+9.8 mg/dl in men and 43.6+11.4 mg/dl in women). Mean value of TG was 133.5+73.5 mg/dl (131.7+72.5 mg/dl in men and 135.7+75.6 mg/dl in women).
Mean value of LDL-C was 128.4+36.9 mg/dl in all patients (126.0+37.2 mg/dl in men and 131.3+36.8 mg/dl in women (Table 1).
Statistically significant correlation was not found between levels of tHcy and TG or LDLC.
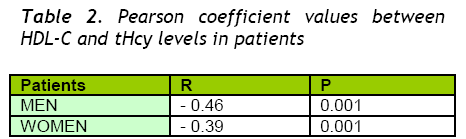
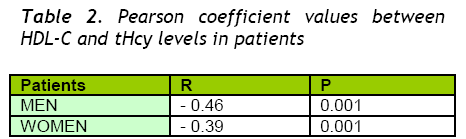
On the contrary, we found negative correlation between tHcy and HDL-C. Pearson coefficient was r=-0.42 (r=-0.46 for men and r=-0.39 for women) (Table 2).
Discussion
Cardiovascular disease is the first cause of death in Greece, with increasing incidence, from 218 to 304 per 100000 during 1980-1987. 9 Alteration in plasma lipoprotein subclass distributions affect mainly atherosclerosis risk. Low plasma HDL-C (hypo-a-lipoproteinemia) is well documented as a risk factor for atherosclerosis. HDLs have several properties that may contribute to their antiatherogenic potential. The best known of these relates to their ability to promote the efflux of cholesterol from cells, including macrophages in the artery wall [10].
HDLs may also protect by virtue of antioxidant, antithrombotic and antiinflammatory properties. The antioxidant properties of HDLs involve activity of compounds such as paraoxonase1 (PON1) [11-15]. that cotransport with HDLs, although apoA-I has also been shown to have antioxidant properties.
Antiinflammatory effects of HDLs include an ability to inhibit both the cytokine induced and the CRP-induced expression of adhesion proteins in endothelial cell. They also correct endothelial dysfunction probably by inducing the synthesis of nitric oxide and most recently have been shown to promote endothelial repair [16].
On the other hand PON1, a multifunctional antioxidative factor, is the major component of HDL-C, which protects from the oxidation of LDL-C [11-13] and was found significantly decreased as HDL-C in stroke patients [16].
As already stated an extra atherogenic risk factor which is not directly related to fat consumption is homocysteine Whatever mechanism is the dominating procedure early findings suggest that a low concentration of HDL-C may explain why people with elevated levels of homocysteine are at increased risk of developing cardiovascular disease.
The relationship between high levels of serum homocysteine and the manifestation of cardiovascular disease is confirmed by the results of the present study, as the significant percentage of ICU patients found with high levels of tHcy (Table 1).
As also shown in Table 1, there was found no statistically significant difference between tHcy levels in men and women.
No statistically significant correlation between TG, LDL-C and tHcy was found, while a negative correlation (r=-0.42) between tHcy and HDL-C levels is detected. This negative correlation is more evident in the group of men vs women (r=-0.46) (Table 2).
Conclusions
1. A negative statistically correlation was evaluated between serum tHcy levels and the concentration of HDL-C in ICU patients
2. No statistical correlation found between the level of serum tHcy and LDL-C and TG serum concentrations
3. A slight but evident difference is detected in the negative correlation (HDL-C and tHcy) between men and women.
Present preliminary findings emphasize once more the need for preventive control of tHcy levels along with the routine lipoprotein fraction determination.
These assays should not be restricted only to high risk age groups, but be also performed in healthy individuals as early as possible. A more detailed investigation within the same group of patients is under way including the HDL-C protein component PON1 as an extra useful biochemical marker.
3605
References
- Malinow M.R, Kang SS, Taylor L.M, Wong P.W. Prevalence I hyperhomocysteinemia in patients with peripheral arterial occlusive disease. Circulation 1989 ;79:1180-88.
- Frosst P, Blom H.J, Milos R. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolatereductase. Nat Genet 1995;10: 111-3
- Barter P.J, Rye K-A. Homocysteine and cardiovascular disease. Circulation research 2006;99: 565 4. Wang H, Tan H, Yang F. Mechanisms in homocysteine-induced vascular disease. Drug Discov Today (dish Mech) 2005;2: 25-31
- Wang H, Tan H, Yang F. Mechanisms inhomocysteine-induced vascular disease.Drug Discov Today (dish Mech) 2005;2:25-31
- Liao D, Tan H, Hui R. Hyperhomocysteinemia decreases HDL by inhibiting apoA-I synthesis and enhancing HDL-C clearance. Circulation; 112 (suppl II) 2005; II-109
- Michael L.G, Genest J.J, Rosen R. Elevated homocysteine reduces apolipoprotein A-I expression in hyperhomocysteinemic mice and in males with CAD. Circulation Res 2006;98: 564- 571
- Doshi S.N, McDowell I.F, Moat S.J. Folic acid improves endothelial function in coronary artery disease via mechanisms largely independent of homocysteine lowering. Circulation 2002;105: 22-26
- Cesari M, Zanchetta M, Burlina A. Hyperhomocysteinemia is inversely related with left ventricular ejection fraction and predicts cardiovascular mortality in high-risk coronary artery disease hypertensives. ArteriosclerThrombVascBiol 2005;25:115-121
- Chimonas E.T. The treatment of coronaryheart disease ; an update. Part 2.Mortality trends and main causes ofdeath in the Greek population. Curr MedRes Opin 001;17:27-33
- 10. Barter B.J, Nicholls S, Rye K.A .Antiinflammatory properties of HDL. CircRes 2004; 95:764-772.
- Lakshman M.R, Gottipati C.S, NarasimhanS.J, Munoz J, Marmillot P, Nylen E.S.Correlation of serum PON1 and HCTL andantioxidant capacity of HDL-C with theseverity of cardiovascular disease inpersons with type 2 diabetes mellitus.Metabolism 2006; 55(9):1201-6.
- Bettowski J. Protein homocysteinylation:a new mechanism of atherogenesis? PostHig Med Dosw 2005; 59:392-404
- Bergmeir C, Siekmeir R, Gross W.Distribution spectrum of PON1 activity inHDL fractions. Clin. Chem 2004; 50:2309-15.
- Karikas G.A., Kriebardis A, Schulpis K,Samara I, Papachristodoulou M,Fytou-Pallikari A. Paraoxonase activitiesand serum homocysteine. ClinicalBiochemistry 2005; 38, p750.
- Karikas G, Kriebardis A, Samara I,Schulpis K, Papachristodoulou M, Fytou-Pallikari A Serum homocysteine levelsand paraoxonase1 activity in preschoolaged children in Greece. Clin. Chem. &Lab. Med; 44(5):623-27, 2006.
- Tso C, Martinic G. High-densitylipoprotein enhance progenitor-mediatedendothelium repair in mice. Arterioscl.Thromb. Vasc. Biol 2006;26: 1144-1149.