Keywords
Nurses' characteristics, nurses' attitudes, death, care of dying, terminal ill patients.
Introduction
Palliative care is described as a way to meet the physical, mental, and spiritual needs of people who are terminally ill and dying [1]. Providing good palliative care requires an inner commitment from the nurses who are involved, that depends on how these nurses view death and persons who are dying. Nurses' view toward caring for dying person could be described by their attitude [2]. According to Peters et al., [3] attitude is formed as a result of evaluating a particular entity with some degree of favor or disfavor and are expected to change over the time by experience. These attitudes are attached to human emotions, and to actions. In this case, death and caring of dying patients.
The care of death and dying patients is a challenge for nurses that has raised a special interest in the recent years [4]. Nurses are frequently exposed to the care of death and dying. This experience often giving rise to anxiety and undesired attitudes that reflect on the quality of patient's care [3]. A study used a convenience sample of 403 nurses from a private hospital and the Visiting Nurse Association Hospice Division, Rooda et al., [5] found that nurses with greater fear of death exhibit fewer positive attitude regarding caring for dying patients. Contact with terminally ill patients was a strong predictor of nurses' attitude.
Nurses' demographic and experiential characteristics and previous education can change and shape their attitudes toward care for dying patients [6]. In a study, Dunn et al., [7] found that nurses with greater exposure to dying patients reported more positive attitudes. A comprehensive study where 115 undergraduate students enrolled in a semester-long educational program related to death, Frommelt [8] found that the intervention group developed more positive attitudes toward death as compared with the control group. Recent work done by Wessel and Rutledge [9] indicated that a video-, reading-, and writing-based intervention education was positively affected attitudes of homecare and hospice nurses toward death.
Understanding nurses' attitudes in a specific situations can therefore predict the quality of EOL care that patients may receive [10]. A study of 410 pediatric nurses, Feudtner et al., [11] concluded that nurses with more years in practice, more hours of palliative care education, and higher hope scores were more comfortable caring for dying children. Similar results was also obtained in a comprehensive cancer center in New York, where, Lange et al., [12] found that nursing experience and age were the variables most likely to predict nurses' attitudes toward death and caring for dying patients.
In palliative care, research studies have indicated that, to provide quality EOL care and establish meaningful and supportive relationships with patients and their families, healthcare providers must be comfortable with death and dying [8,13]. Communication with patients and their families regarding all aspects of their care, in particular EOL care, is critical. However, training in communication generally is lacking [14].
For a change to occur, adequate EOL education is necessary.6 The theoretical education should be individualized and culturally sensitive in order to positively influence the nurses' attitude and promote professional development [2]. In a recent study, Khader [15] found that educational program on Jordanian nurses' attitude toward care of death and dying is highly effective in guiding nurses and improving their care. Moreover, application of a specific standardized educational programs, as EOL nursing education consortium, can change nurses' attitudes toward death and dying and help nurses to cope with the scene and thoughts of death and dying [6].
The previously mentioned studies showed that the value of exploring the influence of nurses' characteristics on their attitudes toward death and caring for dying patients is obvious. However, limited studies found in Jordan exploring how Jordanian nurses caring for terminal ill patients view death and the care of dying. Hence, the purpose of the present study was to assess how Jordanian nurses providing care for terminal ill patients feel about death and caring for dying patients and to examine any relationships between their attitudes and certain nursing characteristics.
Methodology
Study design: A descriptive, quantitative design was utilized for conducting the current study to accomplish its purpose.
Setting: The study was conducted in a public Hospital- the largest governmental hospital in Jordan-Amman. This hospital is a comprehensive health institute providing health services to a large segment of population in Jordan. It also has a separate department (oncology units) for providing supportive care and pain and symptom relief to cancer patients at the end of life.
Population and sample: The study population was consisted of all Jordanian nurses responsible for providing care during the terminal stage of person's life. The study covered a convenience sample of 155 nurses involved with the care of dying patients. All subjects agreed to participate in the study after being informed about the goals of the research.
Instruments: The following two instruments were utilized for the purpose of this study:
The Frommelt Attitude toward Care of the Dying (FATCOD) scale: Is a 30 item tool using a five-point likert scale to indicate respondents' attitudes toward caring for dying patients. The scale consists of an equal number of positively and negatively worded statements with response options of strongly disagree, disagree, uncertain, agree, and strongly agree. Positive items are scored one (strongly disagree) to five (strongly agree). Scores are reversed for negative items. possible scores can range from 30-150. A higher score indicates a more positive attitude toward caring for dying patients.
The Death Attitude Profile-Revised (DAP-R): Is a 32 items scale that used to measure nurses' attitudes toward death. The scale is comprised of five subscales to determine respondents' feelings of (a) fear of death—negative thoughts and feelings about death, (b) death avoidance—avoidance of thoughts of death as much as possible, (c) neutral acceptance—death is neither welcomed nor feared, (d) approach acceptance—death is viewed as a passageway to happy afterlife, and (e) escape acceptance—death is viewed as an escape from a painful existence.
Validity and Reliability
The (FATCOD) scale was used to assess the nurses' attitudes toward caring for dying patients. And the (DAP-R) was used to measure nurses' attitudes toward death. These two scales have been used by several researchers to examine the attitude toward death or attitude toward caring for dying people [5,7,9,16] Payne et al., [17] also used the (DAP-R) scale to compare the level of death anxiety and coping responses in palliative care and accident and emergency nurses. These two scales were originally developed in an American culture, which was different from the Jordanian cultural context. In this study, both scales were translated into Arabic. The validity of both scales had been assessed through a content and face validity in Jordanian culture. Specialized people in the field of palliative and care of dying had reviewed both scales. They had agreed upon a reasonable representation of the questions on the scales of death and dying in Jordanian cultural context. The reliability of both scales was tested by assessing the internal consistency. The internal consistency for both scales was relatively excellent (Cronbakh Alpha for FATCOD = 0.90; DAP-R= 0.86).
Data Collection Procedure: Once an official permission was obtained from the Ministry of Health and the selected hospital. Registered nurses working with terminal ill patients throughout the hospital were invited to participate in the study. The participants were approached and informed about the purpose of the study before being asked to participate. The voluntary nature of their participation was emphasized and the steps to ensure confidentiality and anonymity were detailed. Participants' consent was assured by their willingness to complete and return the questionnaires. Data were collected from June 2010 to August 2010. Completion of the instruments took approximately 10-15 minutes and no compensation was provided to the participants.
Data analysis: Preliminary data analysis was conducted to describe the demographic data of the study sample via the mean, and standard deviation. The t-test and f-test were computed to examine the relationships between nurses' attitudes toward care of dying and death and demographic factors, with post-hoc testing using the LSD test.
Results
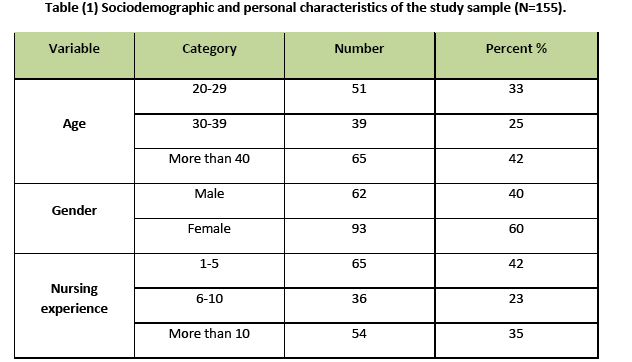
Table one shows the sociodemographic characteristics of the study sample. Most of the study sample was more than forty years old. 93 were females and 62 were males. In respect to nursing experience, the majority of the study sample has 1-5 years experience in nursing, accounting for (42%). Thirty six subjects have 6-10 years experience, and the remaining has more than 10 years nursing experience.
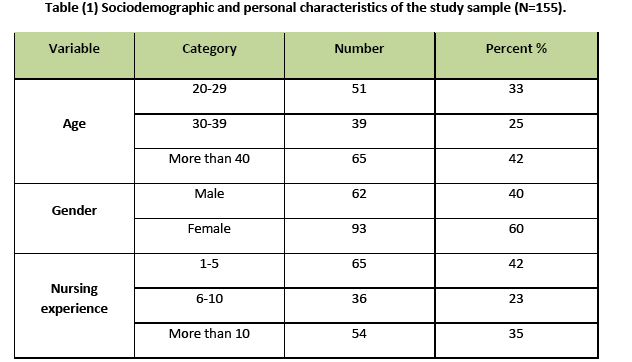
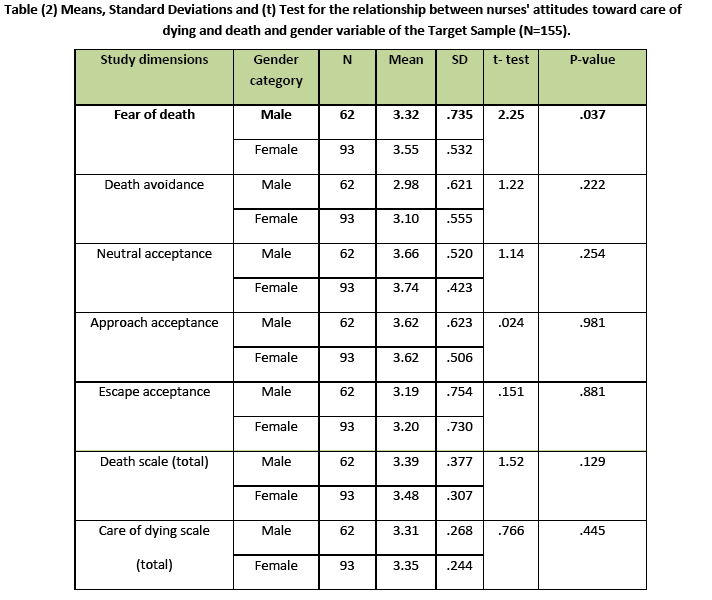
Table two demonstrates mean scores with standard deviations for the relationship between nurses' attitudes toward care of dying and death and gender variable of the target Sample. The analysis of results on death scale shows that there are no significant differences among the gender groups on the total scores. Meanwhile, significant difference exists in the fear of death subscale (p=.037) to the favor of females, suggesting that females has a tendency to exhibit fear of death toward care of dying patient. On the care of dying scale, the Table also reveals that there is no statistical significant difference between females and males. Although, the highest mean was given for females, indicating that they have positive attitudes toward the care of dying patients.
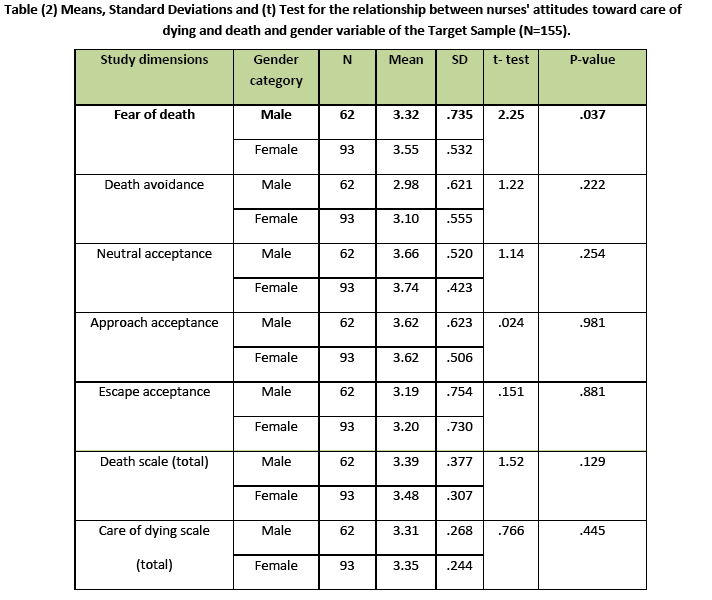
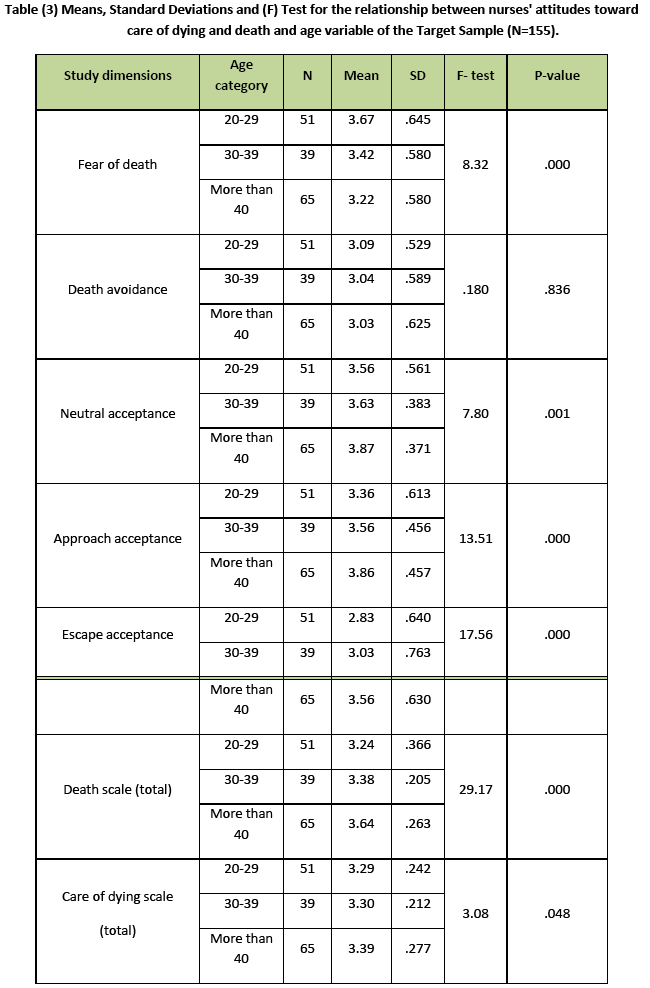
Table three demonstrates mean scores with standard deviations for the relationship between nurses' attitudes toward care of dying and death and age variable of the target Sample. The analysis of results using (F) test shows that there are significant differences among age groups on the total scores of death scale (p=.000) and fear of death, neutral-acceptance, approach–acceptance, and escape- acceptance subscales, (p=.000), (p=.001), (p=.000), (p=.000)&(p=.000) respectively. Post-hoc testing reveals that (RNs) aged 20-29 years score higher on fear of death subscale (p=.000) indicating that younger R.Ns exhibit negative thoughts and feelings toward death than the oldest subsets of RNs. In addition, nurses aged more than 40 years scored higher on death neutral-acceptance than those aged 20-29 years (p=.000) and 30-39 years (p=.008) suggesting that older RNs have a tendency to view death with a neutral mindset, neither welcoming nor fearing from death. They also scored higher on approach (p=.000), and escape acceptance (p=.001) subscales than the other younger subsets. Indicating that older RNs were likely to view death as a passage to a blessed place and view death as an escape from painful experience. On the care of dying scale, a significant relationship between nurses' attitudes and the age demographic factor is present (p=0.048).
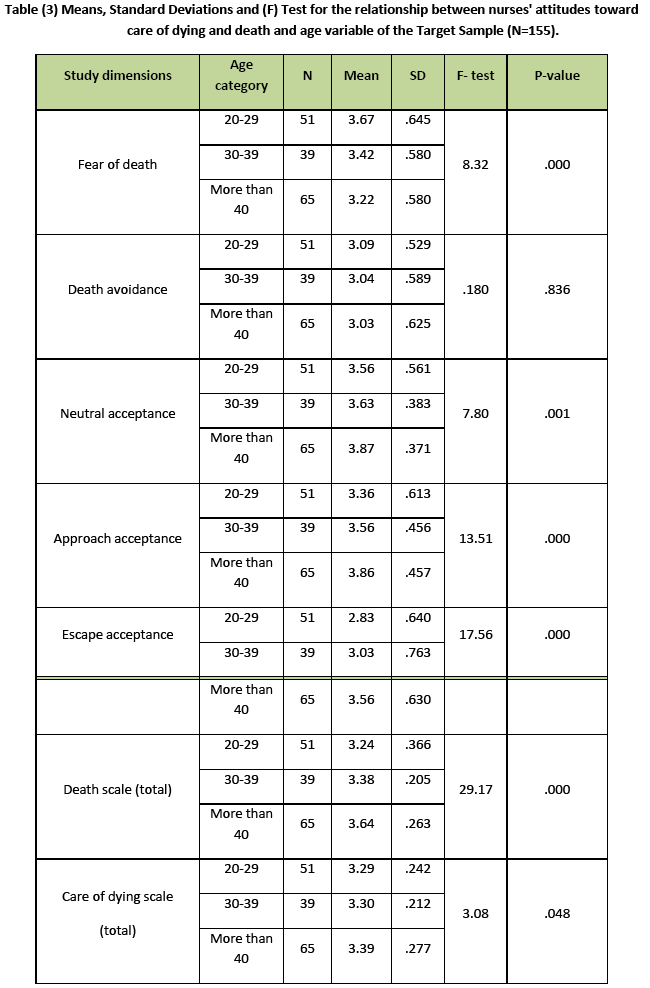
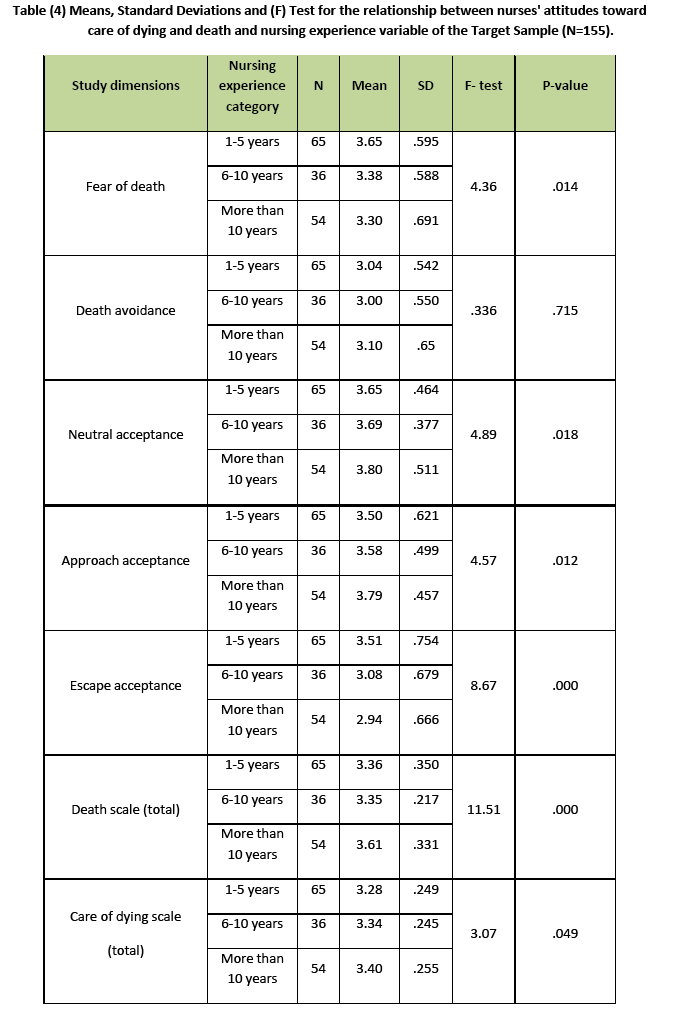
Table four demonstrates mean scores with standard deviations for the relationship between nurses' attitudes toward care of dying and death and working experience variable of the target Sample. The analysis of results using (f) test shows that there are significant differences among working experience groups on the total scores of death scale for RNs with 10 years experience and more (p=.000), and approach acceptance (p=.012) and neutral acceptance subscales(p=.018).
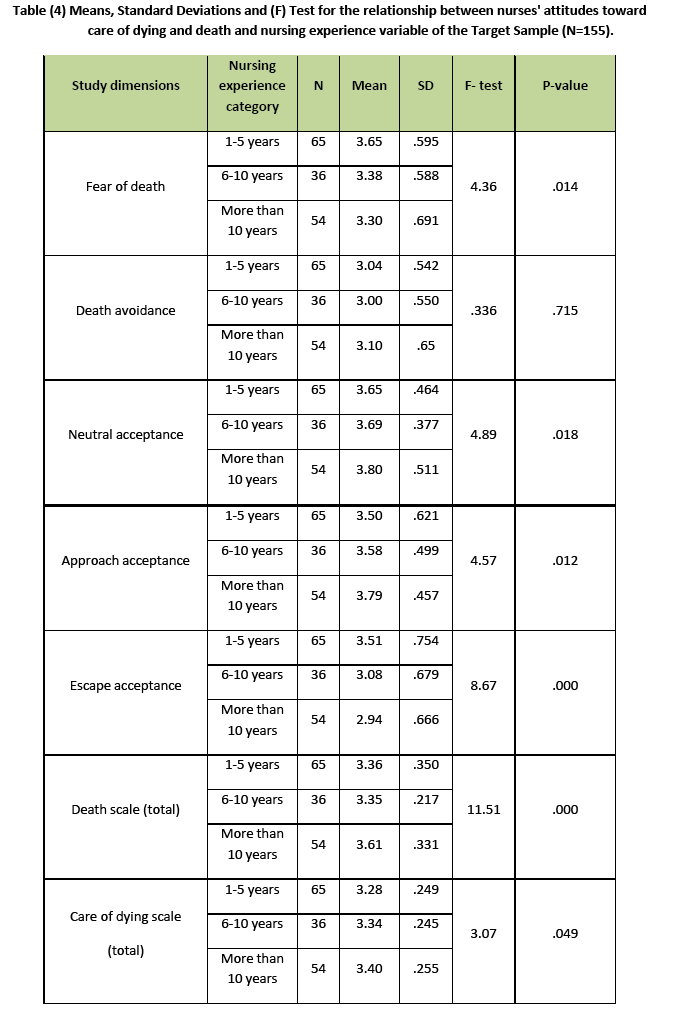
Meanwhile RNs with 1-5 years experience are significantly differ on fear of death (p=.014) and escape acceptance subscales (p=.000). The Table also shows that scores did not significantly differ on the death avoidance subscale. Post-hoc testing reveals that RNs with 10 years experience and more scores higher on approach acceptance (p=.003) and neutral acceptance subscales (p=.009) than other counterparts, indicating that RNs with more experience view death as a passage to afterlife. They also have a tendency to view death with a neutral mindset, neither welcoming nor fearing death. In addition, RNs with 1-5 years experience years scored higher on fear of death (p=.000) and escape acceptance subscales (p=.017). Suggesting that RNs with the least experience were likely to exhibit fear of death and view death as an escape from painful existence.
On the care of dying scale, there are significant differences between nurses' attitudes and the working experience demographic factor. RNs with 10 years experience and above scored higher than RNs with 1-5 years experience (p=.014). This indicated that greater exposure and experience in working with dying patients correlated to more positive attitudes in caring for dying patients.
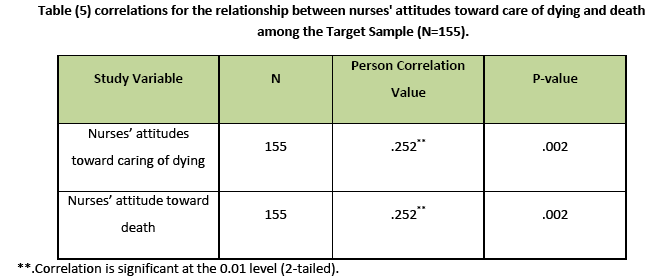
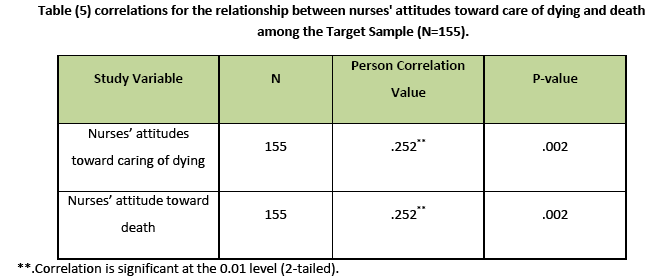
Table five shows significant correlations between nurses' attitudes toward death and caring for dying patients (p=.002), indicating that nurses with greater exposure to dying patients reported more positive attitude toward death. It was found that experience with individuals who were dying have an influence on changing attitude toward death.
Discussion
In the present study, years of experience as an RN and age are strong indicators of showing positive attitudes toward caring for death and dying patients. This finding is consistent with Lange et al., [12] using a similar but larger group of nurses working in a comprehensive cancer center in Newyork. They concluded that RNs with more work experience tended to have more positive attitudes toward death and caring for dying patients. Our results also agree with those of Khader [15]. He reported that age, wards, and recent death experience are associated significantly with nurses' attitudes toward caring of dying. Also, this study strongly support the findings of Dunn et al., [7] Viewing death from a neutral or escape perspective correlates with more positive attitudes toward caring for dying patients and their families. This leads to improved patient outcomes and satisfaction for their patients, family, and nurse providing EOL care. Findings from this study also support a study conducted by Feudnter et al. [11] They reported that nurses with more years of nursing practice, more hours of palliative care education and higher levels of hope were more comfortable in providing care to dying children and their families, had less difficulty talking about death and dying, and showed increased levels of palliative care competency . The findings of the present study support other research [17-19] that found positive relationship between experience and caring for dying patients. This because nurses exposed to dying patients briefly, their coping develop and their skills improve [20]. The more exposure to death and dying, the more awareness of ones own emotions.
Findings of the present study reflected that age has a significant influence on nurses’ toward death and dying [12,21]. It was found that younger RNs tend to report higher levels of fear than do their middle and older subsets of RNs [22]. This is clear if young RN has not seen someone die before they become a nurse. It will reflect on their attitudes toward caring for dying patients; as revealed by previous research [7].
One of the intriguing and disparate findings of the present study was that no significant relationships were found between nurses' attitudes toward care of dying and death and gender factor. Meanwhile, significant difference exists in the fear of dying subscale (p=.037) to the favor of females, suggesting that females has a tendency to exhibit fear of death toward care of dying patient.This result is congruent with a study by Abdel-khalek and Al-Kandari [22]. And contradicting a study by Barrere et al., [21]. This is explained by the close relationship of personality characteristics of femininity with anxiety, thus fearing of death.
Previous studies [9,10,14] have showed that the lack of training in communication and education resulted in uncomfortable attitude with death and dying. Suggesting an urgent need of incorporating into the new RNs employee orientation course as well as hospital training programs.
Limitations
Some limitation of this study should be noted. Particularly, the fact that this study was based on a convenience sample that may not be representative of RNs working with terminal patients at large, there might have been a selection bias that diminish the generalizability of the findings. Therefore, future studies should use random subjects. Another limitation is that, the study used two instruments designed in the American cultural context, which is different from the Jordanian cultural context. Therefore, a content validity of the scales was done. It was found that cultural issues such as questions about religiosity were general and could be applied both in the Muslim and Christian context.
Implications
This study provides health care agencies and academic institutions valuable insights about how certain nurses’ demographics (age, gender, nursing experience, and others) influence nurses’ attitudes towards caring for death and dying patients. As revealed in this study, older registered nurses with more experience tended to have more positive attitudes toward death and caring for dying patients. Therefore, the addition of certain educational courses at nursing faculties and developing continuing educational programs at hospitals along with experiences with terminal patients enhances nurses’ positive attitudes of caring of dying patients and makes the journey from novice to expert nurse a rewarding experience. Moreover, integrating concepts of death, dying and end of life care in all nursing theoretical and practical areas will reflect on quality of care provided during the terminal stage of person's life.
Conclusion
As revealed in this study, older registered nurses with more experience tended to have more positive attitudes toward death and caring for dying patients. RNs without this experience had more negative attitudes, reported more feelings of fear toward death, and avoided thoughts of death as much as possible. Therefore, the need to educate the youngest and less experienced nurses caring for dying patients is warranted. Thus, improving quality care to dying patients and their families.
Recommendation
In light of the findings of the current research, the following recommendations were suggested:
1. This study remark that nurses will be responsible for the care of a larger population of dying patients in the future and, therefore, the need to be educated about death and care of dying patients is warranted.
2. The researchers do believe that strong faith and satisfactory salaries contribute to closer relations and understanding between nurses in one hand and the patients and their families in the other. Therefore, investigation of the influence of the religious belief, and economic status on nurses' attitudes toward death and care of dying is needed.
2813
References
- Bingly A, Clark D. A comparative review of palliative care development in six countries represented by the Middle East cancer Consortium. Journal of pain and symptom management 2009;37(3):287-296.
- Iranmanesh S, Axelsson K, Haggstrom K, Savenstedt S. Caring for dying people: Attitudes among Iranian and Swedish nursing students. Journal of Palliative care. 2010;16(3):147-153.
- Peters L, Payne S, Connor M, McDermott F, Hood K, Morphet J. How death anxiety impact nurses' caring at the end of life: A review of literature. Open Nurs J.2013;7:14-17.
- Roman EM, Sorribes E, Ezquerro O. Nurses’ attitudes to terminally ill patients. Journal of Advanced Nursing 2001;34(3):338-345.
- Rooda LA, Clements R, Jordan ML. Nurses' attitudes toward death and caring for dying patients. Oncology Nursing Forum 1999;26(10):1683-1687.
- Khader K, Jarrah S, Alasad J. Influences of nurses’ characteristics and education on their attitudes towards death and dying: A review of literature. International Journal of Nursing and Midwifery 2010;2(1):1-9.
- Dunn KS, Otten C, Stephens E. Nursing experience and the care of dying patients. Oncology Nursing Forum 2005;32(1): 97-104.
- Frommelt KH. Attitudes toward care of the terminally ill: An educational intervention. American Journal of Hospice and Palliative Care 2003; 20(1): 13-22.
- Wessel EM, Rutledge DN. Homecare and hospice nurses’ attitudes toward death and caring of dying: Effects of palliative care education. Journal of Hospice and Palliative nursing 2005;7(4): 212-218.
- Frommelt KH. The effect of death education on nurses' attitudes toward caring for terminally ill persons and their families. American Journal of Hospice and Palliative Care 1991;8(3): 37-43.
- Feudtner C, Santucci G, Feinstein JS, Snyder CR, Rourke MT, Kang TI. Hopeful thinking and level of comfort regarding providing pediatric palliative care: A survey of hospital nurses. Pediatrics 2007;119(1): e186-e192.
- Lange M, Thom B, Kline N. Assessing nurses' attitudes toward death and caring of dying patients in a comprehensive cancer centers. Oncology Nursing Forum 2008;35(5):955-959.
- Kane JR, Hellsten MB, Clodsmith A. Human suffering: The need for relationship in practice end-of-life care. Journal of Pediatric Oncology Nursing 2004;21(3):180-185.
- Merchaert I, Libert Y, Razavi D. Communication skills training in cancer care: Where are we and where are going? Current Opinion in Oncology 2005;17(4):319-330.
- Khader K. The effectiveness of an educational program on Jordanian nurses' attitudes toward caring for dying patients. Unpublished doctoral disertation. The University of Jordan, Amman, Jordan. 2010.
- Mallory JL. The impact of a palliative care educational component on attitudes toward care of the dying in undergraduate nursing students. J Prof Nurs. 2003;19(5):305-12.
- Payne SA, Dean SJ, Kalus C. Comparative study of death anxiety in hospice and emergency nurses. J Adv Nurs. 1998;28(4):700-6.
- Irvin S. The experiences of the registered nurse caring for the person dying in a nursing home. Collegian 2000;7(4); 30-34.
- Stoller EP. Effect of experience on nurses’ responses to dying and death in the hospital setting. Nursing Research 1980;29(1): 35-38.
- Weigel C, Parker G, Fanning L, Reyna K, Gasbarra D. Apprehension among hospital nurses providing end-of-life care. Journal of Hospice and Palliative Nursing 2007;9(2):86-91.
- Barrere C, Durkin A, LaCoursier S. The influence of End-of-Life education on attitudes of nursing students. International Journal of Nursing Education 2008;5(1):1-18.
- Abdel-Khalek A, Al-Kandari Y. Death anxiety in Kuwaiti middle-aged personnel. Omega (Westport) Journal 2007;55(4):297-310.