Keywords
Blood, body fluid exposure, health professionals, Emergency Department.
Introduction
Recent data have shown that health professionals in every clinical environment often face many occupational hazards such as exposures to human blood and body fluids, involving serious consequences to their health. However, during last 25 years there has been noticed a remarkable reduction in infections by hepatitis B approaching almost 96% in health care professionals as a result of infection control measures, vaccine-induced immunity, better prevention and the apply of a series of recommendations by the Centers for Disease Control and Prevention in daily clinical ptactise. [1-5]
The vast majority of research studies claim that the risk of accidental blood and body fluid exposure is a matter of vital importance for health care workers throughout the world and various strategies need to be introduced to reduce that risk. Assessment of the danger and development of effective preventive and control strategies are the key-elements for the reduction of exposure among health care workers. [1-5] Emergency Department in General Hospital is a demanding sector where the staff is often characterized as “of high risk” due to the lack of personnel and the heavy task of work. According to the literature health care workers in the emergency department or out-of-hospital setting are at especially high risk for exposure to blood or body fluids for the reason that nonemergency health care workers are frequently referred to hospital Committee for immediate treatment of occupation exposures. [1-5]
The present study represents an effort to write down data of the Greek clinical environment of Emergency Department.
The aim of the present study was to explore the reasons that may cause injuries as well as the level of nurses’ knowledge.
Method and material: The sample of the study sample consisted of 124 nurses of 6 General Hospital in Attica working at Emergency departments. Data were collected by the completion of a specially designed questionnaire which apart from the demographic variables, it also included variables concerning the causes, the circumstances of exposure and the level of knowledge of nurses about this danger.
The design of the present questionnaire was based on an elaborate review of the literature concerning factors that contribute to the exposure of health professionals to blood and body liquids.
Statistical analysis: The statistical method used was Pearson’s chi-square test for comparison of proportions. Differences were considered significant at the 0.05 level
Results
The sample studied was consisted of 124 nurses working in the Emergency Department of six General Hospitals in Attica. 79.8% of the participants were women and 20.2% men.
In regard to age, 14.5 % of the sample was within 18-25 years old ετ?ν, 26.6% within 26-35 years old, 43.5% within 36-45 years old and 15.3% >45 years old.
Regarding educational status 56.5% of the sample studied was graduate of Technological Institute, 32.3% of two years education level and 4.8% of university level.
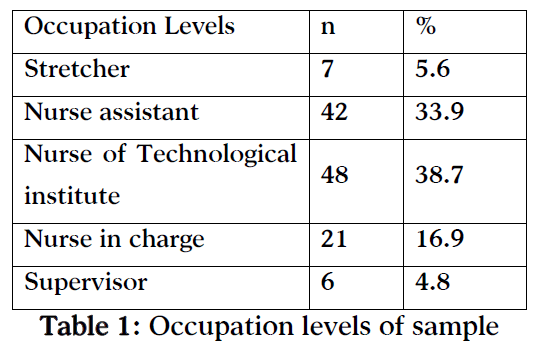
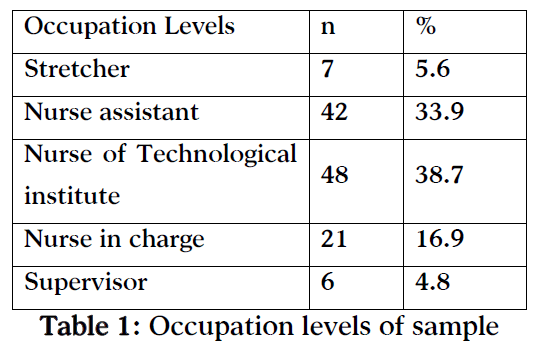
Occupation levels of the sample-studied are seen in table 1.
Regarding the years at work, 39.5% of the participants worked up to 3 years, 14.5% 4-5 years, 14.5% 6-10 years, 8.9% 11- 15 years, 12.9% 16-20 years and 9.7%>20 years.
87.1% of the sample-studied reported exposure to body liquids or blood some time in the past while 50.9% reported exposure within the last six months.
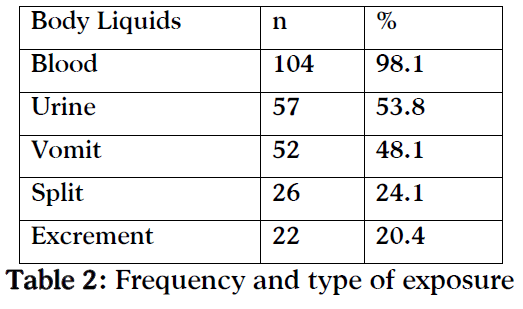
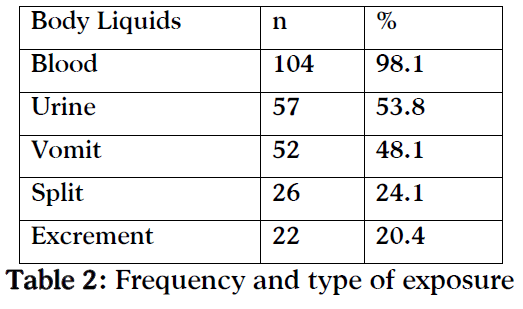
More in detail, the sort of body liquids and the individuals exposed are seen in table 2.
52.8% of participants reported exposure during evening shift while 30.6% and 16.7% in morning and night shift, respectively.
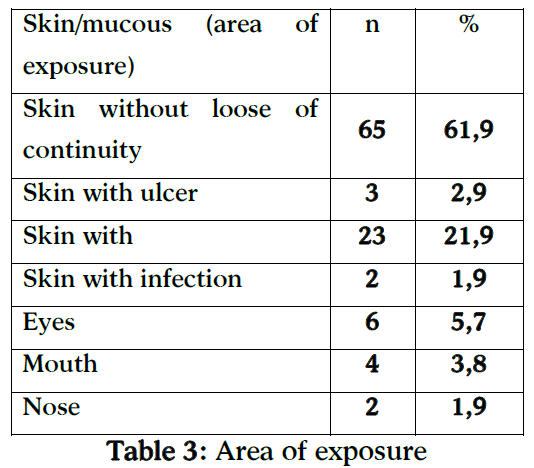
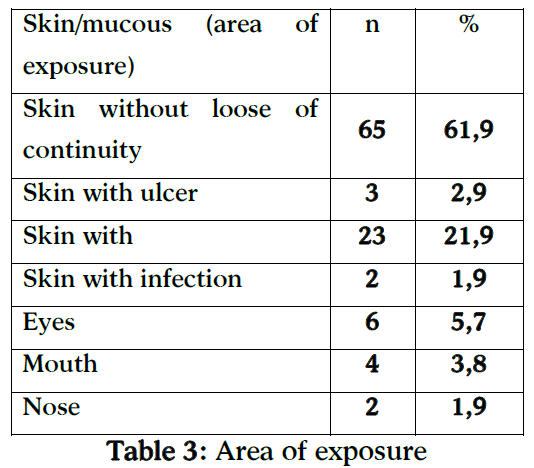
Regarding the level of exposure, 10.3% reported deep wound, 32.7% middle and 57.0% of surface wound, whereas in 25% of the cases the injury regarded skin and its’ continuity. 77.2% reported through the skin needle-stick injury, 42.3% needle-stick injury with visible blood and the 82.2% reported that the needle stick had been used to other patient.
The task performed while injury was in 35.9% recapping of a used needle and in 31.4% the removal of medical equipment.
92.4% of the participants reported less than 5 minutes exposure time. 15.3% and 15.3% took no precaution or did not give an answer.

Regarding the recording of the accident, 68.3% reported it to the supervisors and 34.1% reported to the Committee of Infection Disease. 2.9% of the participants reported disease related to the exposure.
In terms to awareness of risk factors, 67.9% reported that they already knew the risk factors of blood and body liquids exposure while 82% reported that they usually take all the appropriate measures and follow the instructions to protect themselves and their colleagues. 71.8% had been vaccinated for hepatitis Β and 34.7% for tetanus. 93.5% of the participants reported that they knew the correct way of disposal of sharp material to prevent injury. 55.4% reported that it was informed for the hygiene by Committee of Infection Disease.
100% of the sample studied reported that they needed more information.
Finally, men were more likely to report the injury to the Committee of Infection Disease with statistical significant difference, p=0,004 as the 86.4% of men reported the accident versus to 63.4% of women.
Discussion
The “profile” of nurses as it is reflected by the present study is mainly consisted of women, age 25 – 45 years old working for over 5 years. The majority of participants reported exposure to blood or body liquids while blood exposure and needle stick injury were the most frequent.
Exposure to blood and body liquids among all health professionals receives a great deal of attention, globally. [5-10] However, according to Hanrahan et al., [9] further research is needed to elucidate the organizational and behavioural factors leading to sharps injury both within the hospital and other health care settings.
Tarantola et al., [10] showed that 7.649 blood and body fluid exposures were reported by health care workers to occupational medicine departments in 61 hospitals. More in detail, nurses and nursing students accounted for 4.587 (60%) of exposures, followed by nurses' aides and clinicians while most (77.6%) of the reports were related to needle stick injury.
Similarly, Hsieh et al., [11] who explored blood and infectious body fluid exposures for health care workers showed that nurses had the highest percentage (60.6%) of exposure and other job categories including physicians, technicians, cleaning staff, and interns accounted for around 10% each. Furthermore, Adesunkanmi et al., [12] who explored the prevalence of accidental injuries and body contaminations among the operating personnel during general surgical operation, showed that operating personnel sustained 62 sharp injuries (10.5%), these were caused by suture needle in 57 cases (92.0%), towel clips in three (4.8%), knife cut in two (3.2%).
The most frequent activity at the time of the accident exposure was the recapping or disposal of the needle. At the same time, 93.5% of participants reported that knew the correct way of needles disposal.
It is widely accepted that the most common occupational hazard for all healthcare professionals involved in clinical care are the needlestick and sharps injuries mainly caused by inadequate disposal and recapping of needles. According to a previous study by Legge [13] many sharps injuries occur during disposal or because of over-filling of disposal systems. Also Blenkharn [14] supported that despite the great attention given to the safe use of sharps, dangerous needles still find their way into waste sacks instead of a sharps bin. Moreover, blood and body fluid exposures from carelessly packaged clinical waste are common.
Also the results of the present study showed that 30% of the participants took no precaution measures and only 34.1% reported the accident to the Committee of Infectious Disease. Similarly, Gurubacharya et al., [15] who explored the knowledge of health care workers including nurses and paramedical staffs from different departments of a Hospital showed that the knowledge of health care workers about the use of preventive measures was inadequate as only 23% of the participants were in the habit of using gloves for phlebotomy procedures all the time. Furthermore, the results of their study showed that 52 subjects (74%) had a history of needle-stick injuries and only 21% reported the injuries to the hospital authority.
The results of the present study also showed that 71.8% had been vaccinated against hepatitis B and 34.7% against tetanus. Gurubacharya et al., [15] showed that 60% had been vaccinated against hepatitis B, while 40% were not vaccinated against hepatitis B and only 14% had been tested for Anti-HBs antibody after hepatitis B vaccination. Kesieme et al., [16] who determined the knowledge of operating room personnel showed that the majority (86.8%) had the awareness of the existence of Hepatitis B vaccine while 83.8% of respondents believed that the vaccine should be given as part of work place safety measures. Also, Sukriti Pati et al., [17] showed that 55.4% of the health care workers participating their study had been vaccinated and 44.6% were not vaccination-status conscious; of these 27.7% had never been vaccinated and 16.4% were unaware of their vaccination status. Patel et al., [18] claim that the greatest infection hazard is presented by HIV, hepatitis C virus (HCV), and hepatitis B virus (HBV) and the average risk of infection following a percutaneous exposure to these viruses is estimated as 0.3%,3 1.8%,4 and in excess of 30%,5 respectively.
82% of the participants reported that they applied the instructions to protect themselves and their colleagues of blood transmitted diseases while the 67.9% reported awareness of the risk factors for exposure to blood and body liquids. Puro et al.,19 claim that provision of information to healthcare workers thus resulting in prevention to exposure is the primary strategy to reduce the risk of occupational bloodborne pathogen infections. Health care workers need to have access to expert consultants to receive appropriate counseling, treatment and follow-up.
Finally, the vast majority of the participants in the present study reported the need of further information about these occupational hazards. The same results showed Zhang et al., [20] who demonstrated a lack of knowledge regarding transmission of bloodborne diseases and universal precautions. Cooley et al., [21] claimed that there is low awareness of the risks that these injuries pose and highlighted the need of new products with enhanced safety features that should be accompanied by education and training to improve practice in relation to sharps and their disposal. Health care workers should be made aware of hazards, preventive measures and post-exposure prophylaxis to needle-stick injuries. A hospital-wide hepatitis immunization programme should also be started. [22,23]
Finally, the results showed that men were more likely to report the accident compared to women. A possible explanation is that women underestimate the fact, paying no attention to the consequences. The results of the present study are in congruent with those by Dement et al., [24] who showed that more often were exposed males, persons employed less than 4 years, Hispanic employees, and persons less than 45 years of age. Moreover, the same researchers also supported that it is mainly the needle stick injuries and splashes that place health care workers at risk for numerous blood-borne infections including human immunodeficiency virus (HIV), hepatitis B (HBV), and hepatitis C (HCV).
Conclusions
High percentage of the participants reported exposure to blood and body liquids. Blood and urine are seemed to be the most frequent danger for exposure. The most striking is that the vast majority of participants reported need for further information.
Significant measures to reduce the risk of exposure are strict infection control, universal precautions, immunization against HBV, management of exposures as well as procedures for managing staff who have been exposed.
3323
References
- Moran GJ. Emergency department management of blood and body fluid exposures. Ann Emerg Med. 2000;35(1):47-62.
- Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48(6):482-90.
- Shiao J, Guo L, McLaws ML. Estimation of the risk of bloodborne pathogens to health care workers after a needlestick injury in Taiwan. Am J Infect Control. 2002;30(1):15-20.
- Lanphear BP. Transmission and control of bloodborne viral hepatitis in health care workers. Occup Med. 1997;12(4):717-30.
- Petruk J. Sharps injuries. Time to change our equipment and attitudes. Can Nurse. 2003;99(9):18-22.
- Gabriel J. Reducing needle-stick and sharps injuries among healthcare workers. Nurs Stand. 2009;23(22):41-4.
- Twitchell KT.Bloodborne pathogens. What you need to know--Part I. AAOHN J. 2003 Jan;51(1):38-45; quiz 46-7.
- Wilburn SQ . Needle-stick and sharps injury prevention. Online J Issues Nurs. 2004;9(3):5.
- Hanrahan A, Reutter L. A critical review of the literature on sharps injuries: epidemiology, management of exposures and prevention. J Adv Nurs. 1997;25(1):144-54.
- Tarantola A, Golliot F, Astagneau P, Fleury L, Brücker G, Bouvet E; CCLIN Paris-Nord Blood and Body Fluids (BBF) Exposure Surveillance Taskforce Occupational blood and body fluids exposures in health care workers: four-year surveillance from the Northern France network. Am J Infect Control. 2003;31(6):357-63.
- Hsieh WB, Chiu NC, Lee CM, Huang FY. Occupational blood and infectious body fluid exposures in a teaching hospital: a three-year review. J Microbiol Immunol Infect. 2006;39(4):321-7.
- Adesunkanmi AK, Badmus TA, Ogunlusi JO. Accidental injuries and cutaneous contaminations during general surgical operations in a Nigerian teaching hospital. East Afr Med J. 2003;80(5):227-34.
- Blenkharn JI. Sharps management and the disposal of clinical waste. Br J Nurs. 2009;18(14):860,862-4.
- Gurubacharya DL, Mathura KC, Karki DB. Knowledge, attitude and practices among health care workers on needle-stick injuries. Kathmandu Univ Med J (KUMJ). 2003;1(2):91-4.
- Kesieme EB, Uwakwe K, Irekpita E, Dongo A, Bwala KJ, Alegbeleye BJ. Knowledge of Hepatitis B Vaccine among Operating Room Personnel in Nigeria and Their Vaccination Status. Hepat Res Treat. 2011;2011:157089.
- Sukriti Pati NT, Sethi A, Agrawal K, Agrawal K, Kumar GT, et al. Low levels of awareness, vaccine coverage, and the need for boosters among health care workers in tertiary care hospitals in India. J Gastroenterol Hepatol. 2008;23(11):1710-5.
- Patel D, Gawthrop M, Snashall D, Madan I. Out of hours management of occupational exposures to blood and body fluids in healthcare staff. Occup Environ Med. 2002;59(6):415-8.
- Puro V, De Carli G, Cicalini S, Soldani F, Balslev U, Begovac J, et al. European Occupational Post-Exposure Prophylaxis Study Group. European recommendations for the management of healthcare workers occupationally exposed to hepatitis B virus and hepatitis C virus. Euro Surveill. 2005;10(10):260-4.
- Zhang M, Wang H, Miao J, Du X, Li T, Wu Z. Occupational exposure to blood and body fluids among health care workers in a general hospital, China. Am J Ind Med. 2009;52(2):89-98.
- Cooley C, Gabriel J. Reducing the risks of sharps injuries in health professionals. Nurs Times. 2004;100(26):28-9.
- Grande Gimenez Marino C, El-Far F, Barsanti Wey S, Servolo Medeiros EA. Hospital Epidemiology Committee, Federal University at Sao Paulo, SP, Brazil. Cut and puncture accidents involving health care workers exposed to biological materials. Braz J Infect Dis. 2001;5(5):235-42.
- Munro R. Sharps safety. Solving the needlestick nightmare. Nurs Times. 2001;97(24):12
- Dement JM, Epling C, Ostbye T, Pompeii LA, Hunt DL. Blood and body fluid exposure risks among health care workers: results from the Duke Health and Safety urveillance System. Am J Ind Med. 2004;46(6):637-48.