Introduction
The term ‘Lisfranc dislocation,’ attributed to the French-Napoleonic era field surgeon Jacques Lisfranc de St. Martin, characterises fracture-dislocation of the tarso-metatarsal joint complex [1-3]. The Lisfranc complex consists of bony and ligamentous elements, which contribute to providing structural support to the transverse arch [2]. The complex represents the dividing line between the midfoot and forefoot. The oblique interosseous ligament is the strongest structure supporting the tarso-metatarsal joint [4]. Lisfranc injuries can be osseous, ligamentous or a combination, which often result from direct (bending or twisting movements applied to the midfoot) or indirect (crush injuries with soft tissue trauma) and high (motor vehicle accidents) or low velocity (falls) impacts [5]. In non-diabetic patients, high velocity (58%) indirect mechanisms (42%) cause axial loading or rotation on a plantarflexed foot are most common mechanisms for trauma [6].
The original classification system described by Quenu and Kuss described the injuries as homolateral, isolated or divergent based on the direction of the displaced metatarsal [7]. Hardcastle et al. further categorized the injuries into Type A, B or C based on the displacement and incongruity with a system that determines appropriate treatment [8]. Type A indicates complete displacement of all of the metatarsals or completes incongruity of the tarsometatarsal joint complex. Type B reflects partial incongruity, and Type C is a divergent pattern. Myerson [5] modified the system based on the direction of the dislocation. Type B injuries were divided into medial (B1) and lateral (B2) dislocations.
Historically, tarso-metatarsal complex injuries are considered to be extremely rare, with a reported incidence of one per 55,000 cases annually, and contribute approximately 0.2% of all fractures [9]. At least 20% of Lisfranc fracture-dislocations are misdiagnosed or missed during the initial evaluation [9]. Moreover, these injuries commonly affect males during the third decade of life, because of a fall from a height or a motor vehicle accident [10]. These ultimately lead to painful mal-union and impaired functions of the injured region. A delayed diagnosis can compromise the vascular supply. A missed diagnosis can lead to persistent instability, deformity, or arthritis, which necessitates a post-traumatic re-evaluation ten days later [11]. It is imperative, therefore, to have a high-index suspicion when evaluating any patient with mid foot pain, or a history of multiple traumas. Pathognomic features may include plantar ecchymosis at the mid foot level and painful palpations or manipulations of the tarsometatarsal joint [6]. For patients with subtle signs, the provocative maneuver with passive abduction and pronation of the forefoot with a fixed hind-foot can be useful [12]. Clinical symptoms also include soft tissue swelling, increased warmth, weightbearing instability, and significant pain. In addition, imaging with radiographs demonstrate diastasis of the base of the first and second metatarsal and a “fleck” sign in approximately 90% of cases that represents an avulsion off the base of the Lisfranc ligament [5]. CT or MRI reveals occult fractures and dislocations. Treatment depends on the severity and exact underlying cause of the injury. These range from conservative immobilization, open reduction and internal fixation with K-wires, trans-articular screws or plate.
Case Presentation
A 20-year-old African American woman, non-smoker, presented to the emergency department with left foot pain after going on a waterslide at an amusement park. According to the patient, she accelerated in a forward motion, but the first digit of the left foot was caught and pulled in the opposite direction. She stated that the pain was very severe, accompanied by swelling and throbbing pain, hours later. According to her mother, the patient tried placing an ice pack at home, and her symptoms got worse. Her past medical history is significant for controlled asthma and treated sinusitis. She also has a sulfur and penicillin allergy. The patient appeared to be alert and oriented, but had decreased range of motion of the left foot. There was a weakly palpable left dorsalis pedis pulse, when compared to the right. Her pain was severe when the left foot was everted. Swelling was noted at the first metatarsal of the first digit, with tenderness to palpation of the entire foot. No additional signs such as erythema, drainage or acute infections were observed. Initial assessment of anatomic classification, described the dislocation as a Grade II due to tearing of lateral ligaments, and Grade III for functional classification based on decreased ambulation.
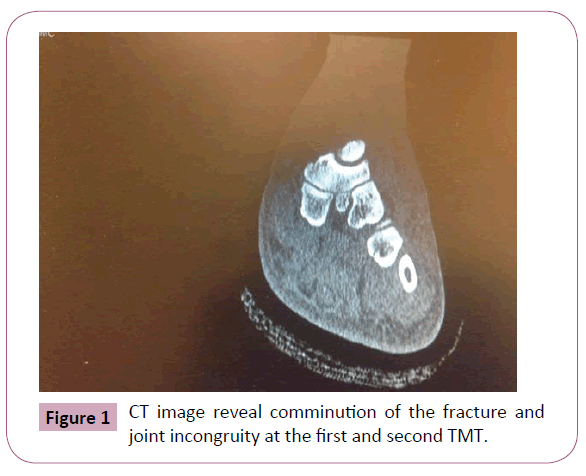
Lateral, frontal, oblique radiographs of the left foot were performed (Figure 1). Findings were significant for an oblique fracture at the lateral aspect of the base of the first metatarsal bone. There was a comminuted fracture at the base of the second metatarsal bone with an intra-articular extension (Figure 1). Mild spatial widening was significant between the first and second metatarsal bone, which was suspected as a Lisfranc Injury. Lastly, moderate generalized soft tissue swelling was also observed. After thorough review, the next step was to apply a Jones compression with a posterior split to stabilize the joint and prevent further exacerbation. Surgical intervention was scheduled ten days later. Upon discharge from the emergency department, the patient was prescribed oral analgesics for pain.
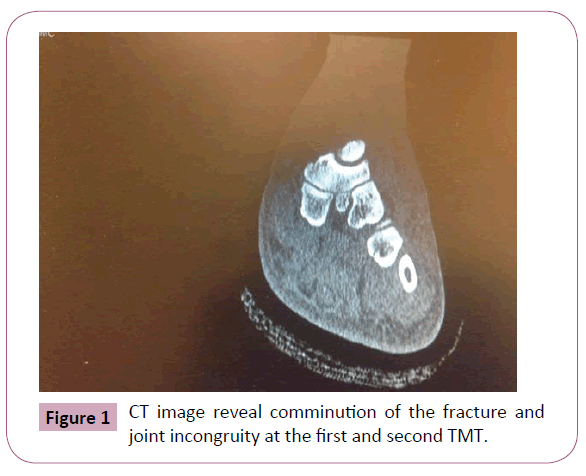
Figure 1: CT image reveal comminution of the fracture and joint incongruity at the first and second TMT.
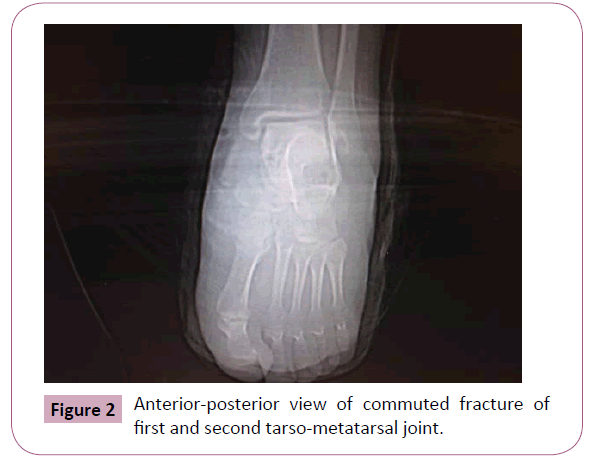
Two days after the initial emergency room visit, the patient followed up in the outpatient clinic. A left foot CT scan was performed in the axial plane, which demonstrated an avulsion fracture at the lateral base of the first, second and third metatarsal bones (Figure 2). A nondisplaced fracture at the medial base of the fourth metatarsal bone was also noted. The midfoot alignment appeared intact.
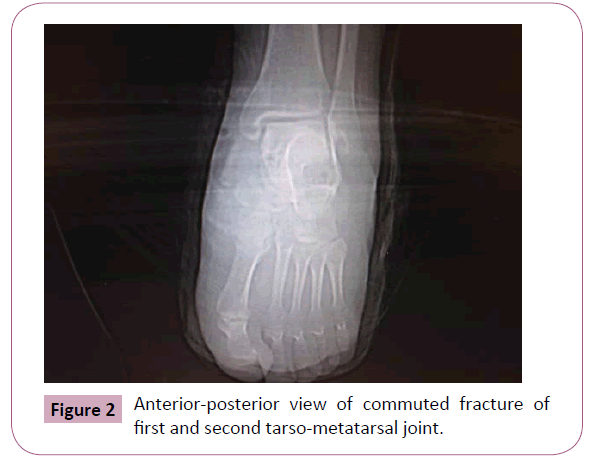
Figure 2: Anterior-posterior view of commuted fracture of first and second tarso-metatarsal joint.
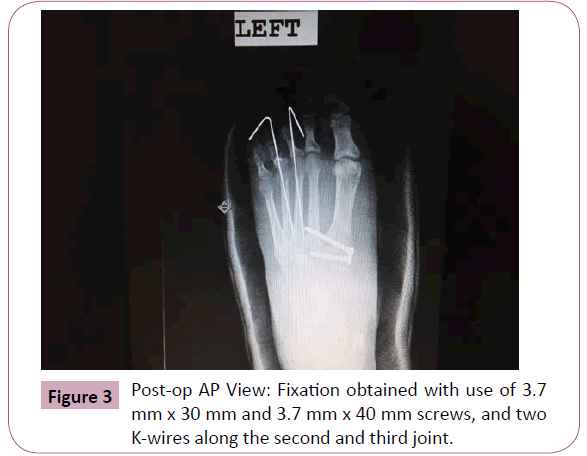
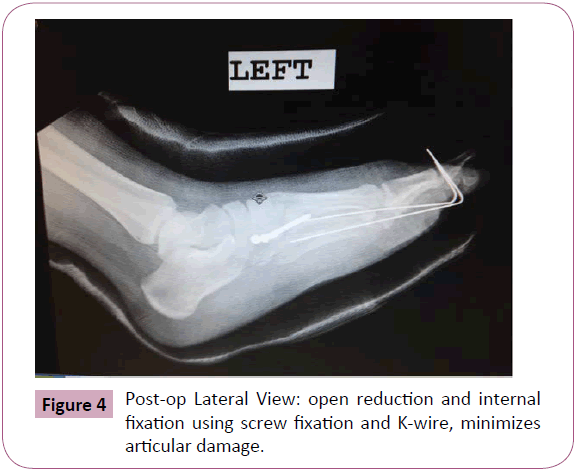
Eight days later, open reduction and internal fixation (ORIF) to surgically repair the Lisfranc complex along with implanted hardware (plates, screws, pins) was scheduled as planned. The patient was sedated under general anesthesia. A stab incision with the left lisfranc repair, using the Wright Medical Charlotte Lisfranc Injury set, was applied. Two screws, which measured 3.7 mm x 30 mm and 3.7 mm x 40 mm, and two K-wires were utilized (Figures 3 and 4). Anatomic closure using a bi-valve plaster cast covered the operated foot.
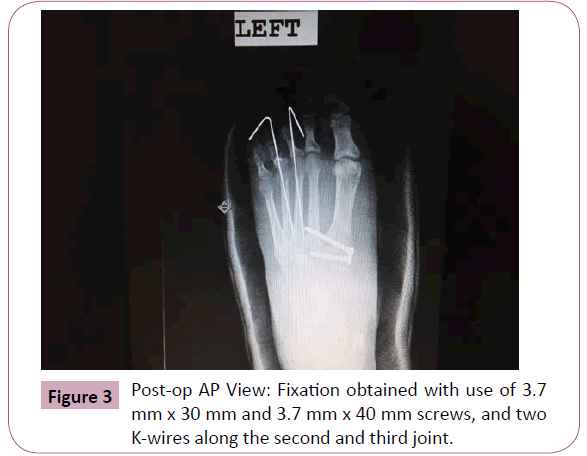
Figure 3: Post-op AP View: Fixation obtained with use of 3.7 mm x 30 mm and 3.7 mm x 40 mm screws, and two K-wires along the second and third joint.
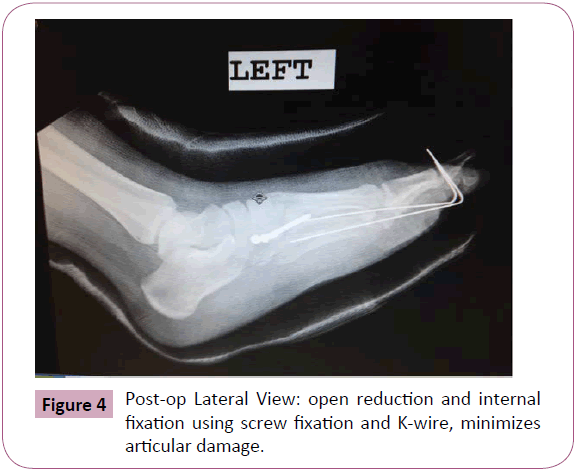
Figure 4: Post-op Lateral View: open reduction and internal fixation using screw fixation and K-wire, minimizes articular damage.
Post-operatively, the patient remained stable without complications. Upon discharge from the surgical suite, she was advised to ambulate with crutches, elevate her foot when resting, and intermittently place an ice bag behind the knee of the operated limb. The patient was informed to contact the emergency room if complications arose after discharge from the hospital.
Post-operative day 9, the patient was re-evaluated in the outpatient clinic. She denied symptoms of fever, nausea, vomiting, and/or dyspnea. She also denied left foot pain. She ambulated with crutches and the cast over the left foot appeared cleaned and intact. Upon examination of the foot, no signs of infection were observed. The two K wires were intact within metatarsals 3 and 4 (Figures 3 and 4). Upon discharge from the clinic, the patient was advised to have physical therapy to regain normal function, which included progressive exercise, neuromuscular training and tolerated functional activity training. She had to follow up to clinic in the following two weeks to remove the K-wires.
Discussion
Historically, injuries of the tarso-metatarsal complex are relatively rare, which require high-index suspicion evaluating any patient with mid-foot pain or with multiple traumas. Lisfranc injuries can be overlooked in patients with multiple traumas and in cases in which diastasis spontaneously reduces. Physical examination typically reveals edema, tender forefoot, and plantar ecchymosis [1]. Based on the initial assessment, grading of anatomic and functional of ankle sprains are also used to determine the timelines for recovery for patients. This patient was placed on Grade II scale for partial tearing of ligaments in the lateral complex, and Grade III scale for inability to walk. The grading system here predicted that this patient’s post-operative recovery and regaining full stability, ranged between 3-8 weeks [13].
A thorough neurovascular examination rules out compartment syndrome secondary to direct and crush injury [6]. Radiographic imaging for Lisfranc injuries are frequently subtle, easily missed, and may not represent the underlying degree of diastasis. Standard radiographs including three views of the foot should be obtained. However, subtle injuries may require bilateral weight bearing films. X-rays may show broken and/or shifted bones in the middle of the foot. An MRI may be helpful for ligamentous damage. CT can help to determine the extent of injury.
The value of CT examination allowed optimal evaluation of malalignment of the midfoot with oblique axial plane to visualize the length of the ligament [5]. In a study described by Gueramy and Karges [9] described that open reduction and internal fixation can be successful after 6 weeks in a patient with a delayed diagnosis. A consensus remains for the protection of the reduction and fixation for a minimum of six weeks with conflicting advice for the necessity for the removal of screws [8].
Open reduction using parallel incisions in the dorsum of the foot and small fragment screws was the preferred method of choice for first and second metatarsal joint injury [5]. K-wires were used to stabilize the lateral column [14].
According to Myerson [5], Kirschner wires, when used alone, have a limited role in the treatment of midfoot injuries. However, they are easy to insert and easy to pull out. For this particular patient, K-wires with two screws were utilized to support the stability of the lateral column of the foot (Figures 3 and 4). The advantage of screw fixation is a rigid reduction with gentle compression across the joint.
Complications, such as pin migration, pin-tract infections, and loss of reduction [15], were discussed with the patient and regular follow-up was advised. There was no residual subluxation or dislocations during postoperative follow-up with radiographs. As described by Arntz et al. [16], there is a 95% excellent achievement in patients with anatomic reduction for tarso-metatarsal injury.
K wires are often buried subcutaneously to decrease the risk of infection [5]. Screw fixation also provides more stability to the medial and middle columns. During the post-operative period, several issues were addressed, including limitations on weight bearing, resuming activities, and the removal of internal fixation. Partial protected weight bearing in a walking boot is permitted after the incisions heal. Progressive weight bearing begins at six weeks and is discontinued eight to ten weeks, depending on the symptoms [5]. Internal fixation is maintained for a minimum of four months for ligament healing. Dislocations, as compared to fractures, take longer to heal and necessitate more time for joint stability [1].
In a randomized prospective study, Ly and Coetzee [17] compared ORIF with primary arthrodesis in patients with ligamentous injury. Patients undergoing primary arthrodesis had a quicker recovery, and superior return to function than those who underwent ORIF. In contrast, Henny et al. [18] evaluated that no difference was observed in the functional results in groups treated with ORIF versus arthrodesis. Therefore, more studies are needed to clarify a definitive recommended treatment.
Conclusion
There is a lack of consensus in the literature regarding surgical treatment, complications, and functional outcomes of Lisfranc injuries [1]. Despite this, one should take into consideration of the initial articular cartilage damage that occurs at the time of injury. A development of degenerative changes markedly increases if the presence or extent of injury is misdiagnosed or unrecognized, and the anatomy is not restored [5]. Unrecognized and untreated injuries can cause an increase in pressure within the muscles that can damage the nerves and blood vessel. If the standard treatment for a sprain does not reduce the pain and swelling, or there is extensive bruising of the bottom of the foot, surgical intervention is required [1]. Surgical treatment allows for the realignment of the joints and returns the bone fragments to a normal position [14].
Author Contribution
JDM provided a thorough history of the patient and performed the necessary surgical procedures to treat the injury. NS was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
7913
References
- Stavlas P, Roberts CS, Xypnitos FN, Giannoudis PV (2010) The role of reduction and internal fixation of Lisfranc fracture-dislocations: a systematic review of the literature. International Orthopaedics (SICOT) 34: 1083-1091.
- Watson TS, Shurnas PS, Denker J (2010) Treatment of Lisfranc joint injury: current concepts. J Am Acad Orthop Surg 18: 718-728.
- Sands AK, Grose A (2004) Lisfranc injuries. Injury 35 Suppl 2: SB71-76.
- de Palma L, Santucci A, Sabetta SP, Rapali S (1997) Anatomy of the Lisfranc joint complex. Foot Ankle Int 18: 356-364.
- Myerson MS, Cerrato RA (2008) Current management of tarsometatarsal injuries in the athlete. J Bone Joint Surg Am 90: 2522-2533.
- Thompson MC, Mormino MA (2003) Injury to the tarsometatarsal joint complex. J Am Acad Orthop Surg 11: 260-267.
- Quenu E, Kuss GE (1909) Etude sur les luxations du metatarse (Luxationsmetatarso-tarsiennes). Due diastasis entre le 1er et le 2e metatarsien. Rev Chir 39: 1-72.
- Hardcastle PH, Reschauer R, Kutscha-Lissberg E, Schoffmann W (1982) Injuries to the tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg Br 64: 349-356.
- Philbin T, Rosenberg G, Sferra JJ (2003) Complications of missed or untreated Lisfranc injuries. Foot Ankle Clin 8: 61-71.
- Desmond EA, Chou LB (2006) Current concepts review: Lisfranc injuries. Foot Ankle Int 27: 653-660.
- Wiley JJ (1971) The mechanism of tarso-metatarsal joint injuries. J Bone Joint Surg Br 53: 474-482.
- Ross G, Cronin R, Hauzenblas J, Juliano P (1996) Plantar ecchymosis sign: a clinical aid to diagnosis of occult Lisfranctarsometatarsal injuries. J Orthop Trauma 10: 119-122.
- DiGiovanni CW, Brodsky A (2006) Current concepts: lateral ankle instability. Foot Ankle Int 27: 854-866.
- Myerson MS, Fisher RT, Burgess AR, Kenzora JE (1986) Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot Ankle 6: 225-242.
- Thordarson DB, Hurvitz G (2002) PLA screw fixation of Lisfranc injuries. Foot Ankle Int 23: 1003-1007.
- Arntz CT, Veith RG, Hansen ST Jr (1988) Fractures and fracture-dislocations of the tarsometatarsal joint. J Bone Joint Surg Am 70: 173-181.
- Ly TV, Coetzee JC (2006) treatment of primarily ligamentous Lisfranc joint Injuries: Primary arthrodesis compared with open reduction and internal fixation. A prospective, randomized study. J Bone Joint Surg Am 88: 514-520.
- Henning JA, Jones CB, Sietsema DL, Bohay DR, Anderson JG (2009) Open reduction internal fixation versus primary arthrodesis for lisfranc injuries: a prospective randomized study. Foot Ankle Int 30: 913-922.