Keywords
Criteria air pollutants; Lung disorders; Heart diseases; Auto-immune diseases; Blood disorders
Abbreviations: APOE: Apolipo Protein E; CB1 & CB2 Receptors: Cannabinoid Receptors; COAD: Chronic Obstructive Airway Disease Coex: Exhaled Carbonmonooxide; CoHb: Carboxy Hemoglobin; ERV1: Expiratory Reserve Volume 1; FBG Levels: Fasting Blood Glucose Levels; FEV: Forced Expiratory Volume; FVC: Forced Vital Capacity; HbA1C: Glycosylated Haemoglobin A1C; HBO2: Hyperbaric Oxygen; IHD: Ischemic Heart Disease; LIDAR: Light Detecting and Ranging Systems; PEF: Peak Expiratory Flow; SRAW: Specific Airway Resistance; TNF-alpha: Tumour Necrosis Factor Alpha; t-PA: Tissue Plasminogen Activator
Introduction
Environmental contamination is a serious concern that arises due to natural and anthropogenic activities and adversely affects human health. One of the major types of environmental pollution attributed to air pollutants is considered in terms of exposure and the consequences due to exposure on human health. Based upon the air pollutant mixture, these can be divided into primary pollutants and secondary pollutants. Primary air pollutants directly emit from the source and enter the atmosphere. Primary air pollutants such as the burning of fossil fuels, gas emissions from vehicles, thermal power plants emit nitrogen oxides while volatile organic compounds (VOCs) are released by human activities such as gasoline and solvents. Nitrogen oxides and VOCs react and form highly reactive secondary pollutants in the presence of sunlight. These emissions combine with primary emissions to form smog. The reactions create tiny airborne particles, surface ozone (O3), sulfur dioxide (SO2) nitrogen dioxide (NO2), carbon monoxide (CO) and affect children, senior citizens, and vulnerable populations with severe health problems. Rapid industrialization, urbanization, and the use of vehicles release harmful gases resulting in outdoor air pollution. The properties of gases such as solubility, concentration, and size determine penetration into the respiratory tract. The burning of fossil fuels such as crops, wood, waste, and dung leads to indoor air pollution producing allergies. Metal and radioactive particles may result in severe noncommunicable health problems. Indoor air pollutants are more concentrated than outdoor air pollutants because the small area covered by the pollutant exerts effects very rapidly; therefore, the pollutants are scattered more efficiently in a limited area and easily penetrate the human body from their origin. Hence, indoor air pollution is more dangerous than outdoor air contamination. Weather and geography affect the location and severity of the magnitude of the pollution. The temperature regulates the length of time taken by smog formation and may occur more rapidly and severely during sunny days. When temperature inversions occur and the wind is calm, smog may remain trapped over the area for a few days. As traffic and other sources add more pollutants to the air, the smog gets worse [1].
The London smog consisted of SO2 resulted in approximately 1200 deaths within a year while 6000 deaths were reported due to the Bhopal gas leak of 40 tons methyl isocyanate. Recently similar pollution accidents were noted in Delhi when emergency measures need to be maintained by temporarily shutting down all types of smog releases to control the emissions. SOx concentration was found more in urban areas, but later this gas reached rural areas as the study revealed that the daily mean concentrations of SOx had fallen 1000 to 500 μg/m3 [2].
Largely developed chimneys help to transport pollutants’ dispersal widely, and the concentration fell to 25 μg/m3. The correlations among criteria pollutants (NO2 vs. CO; NO2 vs. PM2.5; NO2 vs. PM10) from 2004 to 2009 vary annually and spatially from site to site, indicating the heterogeneous nature of the air mix in Delhi. Significant PM10 concentrations were initiated by roadside dust, industrial emissions, and long-distance transport from the Thar Desert during summertime. Recent studies revealed that North Indian cities like Delhi and Lucknow are polluted predominantly by particulate matter. NO2 and SO2 concentrations have decreased mostly due to fuel switching and more industrial controls. However, aerosol concentrations emitted from sources such as vehicular, industrial emissions, road dust, and crop burning, domestic, or construction activities are on the rise with ever-increasing population and urbanization. The highest level of PM10 (200 μg/m3) was measured in residential areas of Lucknow which is above the limit (60 μg/m3) prescribed by the central pollution control board, indicates distinct seasonality during winter months. However, the concentration levels of SO2 (8 μg/m3) and NO2 (30 μg/m3) are at permissible limits. The pollutants enter the deep alveoli of the lungs and may also damage the brain barrier [3]. These data show that currently, air pollution has become a severe problem, especially in developing countries, which results in non-communicable diseases such as ischemic heart disease, stroke, COPD, lung cancer, etc. and increases the risk for disease in 75% of the human population. The association of neuropathologic damage with CO was evidenced through globes pallidus lesions, white matter changes, and diffused low-density lesions in the brain. Even at the room temperature level, CO emission is highly toxic, which affects the sense organs such as the brain and heart leading to several disorders. Very low levels of COHb (<5- 10%) were detected in smoking people. CO enters the organism and combines with haemoglobin which occupies the oxygen-carrying capacity, thus decreasing organ functions. The severe CO toxicity may induce tachycardia and tachypnea by cellular hypoxia. CO exposure produces morphological changes in the myocardium and lowers skeletal muscle function due to cytochrome oxidase inhibition. Tissue injury and Electrocardiography (ECG) results verified the mortality in hospitals [4].
Nitrogen dioxide plays a major role in the atmospheric reactions that produce ground-level O3 or smog. The health risk factors are directly or indirectly dependent upon cooking practices in the most crowded places in a small area. Short term exposure of NO2 leads to a greater risk for hospitalization rate and diagnoses for cardiovascular disease (CVD related mortality (69%), pulmonary disease (28%) while its combination with 10 μg/m3 PM2.5 increased cardiovascular mortality rate. The combined short-term effects of PM, O3, and temperature were observed in 70 subjects suffering from diabetes mellitus by examining systolic and diastolic blood pressure [5]. The blood pressure was elevated due to the PM-induced rise in myocardial oxygen demand.
Early population-based cross-sectional studies indicated that the mortality rates with long-term effects depend upon the concentration of pollutants [6]. Physical activity reduced the mortality frequency with CVD deaths [7]. A monitoring program was held in 11 fitness centers in Libson and the parameters such as temperature and humidity, PM, CO2, CO, and VOCs were monitored [8]. The results indicated enhanced toxicity attributed to infections in the respiratory tract and inner parts of the nose. Acute lower respiratory infections diseases occur above the epiglottis such as pharyngitis, laryngitis, or rhinitis [9]. The daily counts of health-related incidence and population of the monitors situated in the study area observed individual data of pollutants with approximately 1% increase in daily deaths with the level of particulates [10]. Ambient air contains various highly reactive pollutants such as oxides of nitrogen and oxygen which are inhaled with the particles and produce a severe effect on the tissue cells of the lung [11]. Long-term exposure to outdoor air pollution increases the risk of chronic respiratory disease leading to CVD [12]. Alwahaibi and Zeka [9] found allergic and acute respiratory health effects in young populations due to air pollution exposure. They defined allergic diseases as conjunctiva, dermatitis, and eczema while acute respiratory diseases included upper and lower respiratory infections, pneumonia, and asthma. This review is primarily concerned with the examination of studies on some important criteria air pollutants including PM10, PM2.5, CO, NO2, and SO2 in terms of methodology and human health risk assessment. Pollutants and their adverse health effects with corresponding concentrations are presented in Table 1.
| Pollutant |
Concentration |
Health Effects |
| Particulate Matter (PM) |
| PM10 |
100-299 µg/m3 |
Exposure to air-borne particles shows an increase in mortality and morbidity. The particles can easily penetrate deep into the tissue like alveoli in the respiratory system and cause severe cardiovascular problems. Particulate matter has stronger effluence over the age of 65 cause respiratory deaths and also a decrease in pulmonary function. |
| PM10 |
150 µg/m3 |
The typical range of about 102-105 cm2 and 1-100 µg/m3 increased 1.7% of mortality with 3.3% increase in COPD and 4% pneumonia deaths. |
| PM10 |
150 µg/m3 |
The short-term exposure indicated the effects of daily levels of PM10 for CVD hospitalization in daily life during 1995-2004. |
| PM2.5 |
57 µg/m3 |
The impact of PM2.5 concentration on people leads to premature births. |
| PM2.5 |
11-33 µg/m3 |
Mortality in 65-year aged persons was recorded more (0.64%) than the younger ones (0.34%) and diagnosed with the probability of respiratory diseases. |
| PM2.5 |
10-27% µg/m3 |
Clinical conditions, especially in older people and acute health illnesses, were affected more with pre-existing diseases like diabetes and CVD. |
| PM10& PM2.5 |
10 µg/m3 PM2.5
& 0.74% per 14.4 µg/m3 PM10 |
A 5- lag day’s increase 1.05% per 10 ug/m3 in PM2.5 and 0.74% per 14.4 µg/m3 in PM10. It is associated that PM2.5 had a deep association with mortality than PM10 because it’s lesser size. |
| PM10& PM2.5 |
54.4 µg/m3 |
The epidemiological studies differentiated the complete attributable mortality and morbidity in the case of PM2.5 and PM10 in the 5-year of period of time. |
| PM10& PM2.5 |
115 µg/m3 |
By increasing PM concentrations, premature births had reached 0.59 million cases. |
| PM10 & PM2.5 |
120 µg/m3 PM10,
100.2 µg/m3 PM2.5 |
The concentrations of endotoxins with pollutants including environmental factors highly affected the houses where biomass fuel was used than LPG-using houses. It was observed that the deposition of particulate pollutants was found more in infants and children than in adults, which caused 75% of endotoxins deposition in the alveolar region. |
| PM10 & PM2.5 |
65.5 µg/m3
153 µg/m3 |
The endotoxins of PM (PM2.5, PM10 & PM1) are the major indoor air pollutants that can cause respiratory problems. |
| CO2, PM |
900-1500 µg/m3 |
Mainly children, women, and elderly persons were observed with frequent illness, cough, and other respiratory problems due to improper ventilation system which spread endotoxins rapidly. |
PM10, PM2.5
& NO2 |
56.3 µg/m3,
29 µg/m3,
41.8 µg/m3 |
Short-term air pollution had increased the respiratory hospital admissions of all ages (0-65 yrs). |
| Gaseous Pollutants |
| Carbon monoxide (CO) |
3.69% |
Higher COHb levels were found in the traffic police at junctions than the normal office staff; correlated with high mobility and mortality rate, i.e., 400-500 deaths in 5 years (1999 to 2004) in the US. |
| CO |
70% |
In India, the traffic regions have dangerous effects because these are ground-level sources, so it may spread easily. |
| CO |
2.55-4.98 µg/m3 |
Severe headache, cardiovascular disabilities, dizziness, etc. CO exposure may lead to premature births in pregnant women and low birth weight in newborn babies. |
| CO |
0.46-11.3 µg/m3 |
Attack in cellular functions, tissue injury, and transmission in the central nervous system. |
| CO |
33.1 µg/m3 |
Acute CO poisoning in blood samples leads to myocardial perfusion. |
| CO |
≥ 500 µg/m3 |
Chronic exposure causes CO toxicity like general illness, flu-based fevers, and psychosomatic symptoms. The chronic toxicity is more because the CO levels lead to tissue damage and reduce oxygen-carrying capacity. So it is very dangerous to sensitive parts like the brain, heart, and lungs. |
| CO |
8.7-87 µg/m3,
100 µg/m3 |
COHb is dependent on its CO level and the way of exposure as well. The ambient air pollution with CO at 100 ppm is more harmful to health. |
| CO |
2.5-4.98 µg/m3
(0.008 µg/m3-exposure as CoHb levels) |
Toxicity in cellular level bonding refers oxygen-carrying capacity of Hb as the major acute mechanism. Non-smokers with high COHb levels were observed. |
| CO |
100-400 µg/m3 (0.01%-0.04%) |
Not only coronary but also causes neurological problems. Disurbance in brain developing and functioning caused by CO toxicity. It induces tissue hypoxia which affects the cerebellum. |
| CO |
13.6 µg/m3, 48% of CO exposure |
About 84% of people suffered from headaches at 21.3% COHb level. |
| CO |
11-25 µg/m3
(1-8 hrs) |
The headache is caused by chronic CO poisoning. COHb levels >30-40% cause dizziness, general weakness, fatigue, and sleeping sickness. These symptoms can cause from days to months rather than 6 months. So mainly the CO effect can cause by a long-term more efficiency. |
| CO |
0.5 µg/m3 |
Formations of COHb mechanism in bloodstreams may lead to coronary artery diseases. The CO diffuses from the alveolar capillaries through a membrane into the bloodstream by diffusion method. The affinity absorption of CO to Hb is 210 times more than the O2. This mechanism affects mortality by arrhythmia and heart attacks. |
| Nitrogen dioxide (NO2) |
30-90 µg/m3 |
Serious lung damage with a delayed effect, shortness of breath, and chest pains. |
| NO2 |
0.62 µg/m3 |
Increased NO2 concentration increases lower respiratory infections and also increases asthma in children. |
| NO2 |
0.053-10 µg/m3 |
Patients with asthma and COPD cause rapidly responsiveness to NO2. Traffic and indoor air pollution cause respiratory illness, bronchitis, etc. |
| NO2 |
>200 µg/m3 |
Higher-level exposure causes cough, chest pain, vomiting, and headache. It affects tachycardia, radiographic bilateral pulmonary functions, etc. |
| NO2 |
50-100 µg/m3 |
Asthmatics are susceptible to long-term NO2 pollution. |
| NO2 |
>100 µg/m3 |
Acute and chronic exposure of NO2 was observed experimentally and showed greater mortality by inducing bacterial and viral infections. |
| NO2 |
≥ 40 µg/m3 |
NO2 causes an increase in asthma by 3.1%. |
| Sulphur-Di-Oxide (SO2) |
1-2 µg/ m3;
Response concenteration-8 µg/m3 |
SO2 is one of the pollutants that can be more harmful due to outdoor than indoor pollution, influenced by pollutant responsiveness. |
| SO2 |
1.5-13 µg/m3 |
SO2 concentration goes to peak while doing physical activity like jogging, exercise, etc., and observed high SO2 concentration in oral breathing. |
| SO2 |
1-50 µg/m3 |
SO2 response gradually increases from nose to oral while doing mild to heavy exercise, showing the sensitivity of the pollutant. |
| SO2 |
3-4 µg/m3 |
The relationship was observed for mortality based on physical factors and different seasons. |
| SO2 |
19.2 µg/m3
830 µg/m3 |
At low temperatures and the low levels of air pollution, the hospital admissions for asthma and CVD were observed in daily mortality. |
| SO2 |
65.7 µg/m3,
≥ 0.005 µg/m3 |
FEV and FVC observed for the associations on mortality. |
| SO2 |
10 µg/m3 |
Lower FEV1 by 54 ml. caused bronchitis, emphysema, or asthma and respiratory illnesses in newborns and elderly people, but now young people (>16-35-65>) are also affected. |
| SO2 |
19.2-23.3 µg/m3 |
SO2 with the association of PM shows higher sulfate levels in urban areas which caused lower FEV1 levels of about 151 ml. |
| SO2 |
4.2-27.8 µg/m3 |
The associations of TSP, TSO4, and SO2 affect preadolescent children causing cough, respiratory illness, etc. |
| SO2 |
2.29 µg/m3 |
The concentrations can induce hypothesis by inflammatory pathway to cause cardiovascular problems. |
| SO2 |
3.9-4.13 µg/m3 |
The bond between the pollutants like sulfate with biological mechanisms leads to CVD. Two major traffic air pollutants (SO2 & O3) have marked inflammation, oxidative stress, and blood coagulation in healthy humans. |
Table 1 Pollutants and their health effects along with pollutants’ corresponding concentrations.
Methodology
The measurement of the degree of pollution using data for modeling and measuring the quantity and quality of any pollutant in a systemic way is known as a pollution monitoring method. Since the main objective of this review is to assure the health impacts of pollutants due to indoor and outdoor exposure, different techniques for different samples are required to measure the concentrations of the pollutants. Earlier the studies were simply depending on the changes in clinical implications as per the pollution effects. However, the studies after the 1960s were developed by population-based cross-sectional methods followed by mortality rates with long-term and short-term effects. The research methods are based on the evaluation of the daily counts in relation to hours to minutes by monitoring health-related incidence equipment. Pollutant-wise methods for their measurements according to health impacts have been given in this section.
Particulate matter (PM)
The particulate matter may deposit easily in different parts of the body and can spread to upper parts like the nose and also penetrate deep into the alveolar region of the respiratory system. Measurements for particulate matter began in 1964 with simple statistical calculations. Later on, the methodology was developed and induced better PM estimations. The regression analysis for PM concentrations with reference to the hospital admissions indicated the increased admissions due to respiratory illness caused by PM10 emissions. From the 1970s to the mid-1990, the PM effects have been calculated by studying the population-based observations. After that, during 1970- 1980, elemental concentration became a major source for mass balance. The Chemical Mass Balance (CMB) receptor was used for measuring the particulate matter to determine PM2.5 and PM10 concentrations by different sources such as diesel, fossil fuel, and vehicle exhaust. The sources like coal combustion (42%), vehicular emission (47%) were determined through the CMB model and observed seasonal variations in Kolkata from 2003 to 2004. They monitored ambient PM10 mass concentration by atomic emission spectrophotometer and found higher concentrations in winter seasons. The 24-hour PM10 concentrations were analyzed by poison regression analysis model, and gravimetric filter-based method with meteorological aspects. The scientists estimated the concentrations of PM10, PM2.5, and PM1 in indoor areas by using Lung Dose Evaluation Programme (LUPED) model. This model is based on the endotoxins concentration deposits in the cellular regions of the respiratory tract and its breathing rates at regular intervals of time. Particulate matter was also determined by low pressure three cascade impactor or Dektai impactor. Therefore, the analytical methods transformed from simple population calculations to fully scientific and economically skilled equipment, which gives better results to determine the effective concentrations [13].
Carbon monoxide (CO)
The effects of CO have been recognized in neuropathy logical studies in white matter in the brain through CT and MRI in the 1970s. Later on, it was observed with the help of simple graphical experiments followed by identifying COHb levels. The COHb levels were estimated in about 40 myocardial ischemic male subjects through electrocardiography and results showed reduced COHb levels in the range from 0.6% to 0.3% and a decrease in subendocardial thickness and angina pre and post-exercise tests. The symptoms hypothesized as CO effect were examined through a simple questionnaire based on the tool named CH2OPD2 (community, home, hobbies, occupation, personal habits, diets, and drugs) mnemonic and sequential questionnaire to obtain an environmental exposure history. The cross-sectional studies on the blood samples of 708 subjects experienced the analysis of headspace capillary gas chromatography, mass spectroscopy with an HP mole sieve plot column. The correlation between CO exposure and carboxyhaemoglobin was analyzed through regression models which indicated that COHb concentration increased by 1.29% to 10% increase of CO exposure. The blood samples of a group of 30-to 40-year-old traffic police were compared with the same age people of a hospital for about 2 years through spectrophotometer and Mann-Whitney U test to determine the difference in CO toxicity. The scientists had developed the scientific techniques according to increasing concentration and varieties of sources and found that time series analysis is the most suitable model to predict the CO concentrations. On the other hand, the removal analysis of CO toxicity is becoming an advanced technique nowadays; Norma Baric Oxygen therapy is the method to eliminate CO toxicity from the patient. Empirical mode description (EMD) was used to calculate the suicide population in association with air pollution and weather variables as one of the factors. Therefore, these studies prove that CO affects not only the blood serums but other systems of the body are also affected [14].
Nitrogen dioxide (NO2)
The effects of long-term NO2 exposure were identified by using different lung models and cultured cells, regression models, and diagnosed with a tissue injury. NO2 responsiveness to asthmatic patients was observed for 30 min. exposure in four days and found SRAW at 0.05 p.m. of the pollutant level with 40% decreases in PVP by inducing methacholine. The analysis of lung parameters Fev1, Fec, and specific airway resistance of NO2 exposure revealed acute responsiveness. The asthmatic subjects were exposed to 0.30 ppm NO2 concentration after exercise on a treadmill with a resting time of 10 minutes and revealed increased SRAW but decreased Fev1 and Fec. As an indoor air pollutant, NO2 can affect sometimes in the short term and long term as well. Long-term exposure (4 years) to high levels of NO2 concentration (>40 μg/m3) affected 5758 children diagnosed with lung functioning parameters and skin prick tests resulted in decreased lung function [15].
Sulfur dioxide (SO2)
The breathing patterns of the responsiveness of SO2 were examined through a simple questionnaire survey of selected areas such as Nashville and its suburban fringe. The Oesophageal cathedral method was applied on 8 male subjects to examine pulmonary flow resistance and lung volume through the gas compression method. The studies on the effect of SO2 on broncho-constriction through SRaw revealed that the induced SO2 stimulates bronchi construction in persons affected with mild asthma while hyperventilation induces the increasing bronchi construction. The association of compound mucous cilia with SO2 exposure was observed through the biological marker and revealed that SO2 caused the epithelial tissue injury. The data of suspended particles like sulfates, nitrates, and mortality of the Santa Clara County, city were correlated with relative temperature, humidity, and seasonality by a regression model to determine the effectiveness of the pollutant. The poison regression, autocorrelation analysis of 15 European cities with a population count, concentrations of black smoke, nitrogen dioxide, and ozone revealed that meteorological variables affect the air quality and observed the SO2 concentrations ranged approx. 30-300 μg/m3 could lead to a positive association with daily mortality in highly polluted years of Athens (1984-1988) through an autoregression model with a 1-day log. Comparative studies on associations of pollutants had been conducted by many scientists recently. The cross-sectional studies of >16 yrs (1995 to 2001) revealed SO2 concentration of approximately 10 μg/m3 correlated with 54 ml of Fev1 in individuals caused a lower rate of lung function. Fev1 and Fvc were measured by Spirometer and statistically analyzed by chi-square test and variance of the post and present estimations. The association of SO2 and PM affected around 1414 persons who lived in higher sulfate and STR (Sulphur transformation ratio) area with lower Fev1 levels by 151 ml. The effect of SO2 concentration (151-350 μg/m3) on lung function growth in about 1001 preadolescent children of 10 to 12 yrs age was observed in Cracow and Poland by measuring Fvc and Fev1 for 2 years through spirometric and multivariate model analysis. The study of biological mechanisms through the Mann- Whitney method revealed the effects of SO2 and inflammatory markers, oxidative stress, fibrinogen, coagulation factors were measured by the Elisa-based method. Blood samples of diabetic patients were analyzed for different parameters such as CRP, Glucosamine, HbAc, haemoglobin over 3 weeks. The data were analyzed with the association of pollutants and meteorological factors statistically by Spearman and Pearson correlation coefficient [16].
Results and Discussion
The increasing population along with industrialization and urbanization are the major causes to modify the efficiency of the pollutant concentration as the effects of pollutants can also be seen in a short period of time. However, all the diseases which affect people are caused by several microorganisms, but their productiveness can depend on the increasing pollutant concentration. Depending upon the efficiency of the diseases, it is classified into Physiological and Psychological diseases in this study. The effects of the diseases related to individual pollutants are discussed here within these two categories.
Physiological diseases
Health problems related to the respiratory system due to major pollutants prevent the oxygen-binding capacity with the blood, PM causes inflammation in the lungs; NO2 causes respiratory infections, especially in children, and increases chronic respiratory diseases including shortness of breath, etc. On the basis of reviewing peer-reviewed papers of each pollutant, it was found that physiological diseases that occur due to pollutants are CVD, COPD, asthma, diabetes, and cancer. Therefore, it is necessary to identify potential pollutants’ correlation with the diseases.
PM10 and associated physiological diseases: Previous studies reveal that the mortality due to PM concentration may be evidenced mainly through the criteria of observing hospitalization. Hospital admissions due to PM caused pulmonary inflammation triggering systemic hypercoagulability. Increased heart rate leads to myocardial infarction followed by heart attack and a high risk of CVD mortality. Postmenopausal women have been seen suffering from obesity due to the 10 μg/m3 PM exposure and found 76% increased risk of mortality due to CVDs. The associations of various pollutant effects on hospital admissions due to CVDs have been increased by 2.79% per 23 μg/m3 PM10 and 1.66 μg/m3 CO concentrations. Some studies revealed that PM affects middle-aged people and causes CVDs and observed a tremendous increase in C - reactive protein, a protein produced by the liver that shows the presence of inflammation and breast cancer. PM10 caused CVD, COPD, and pneumonia diseases observed through hospital admissions due to vehicular pollution; long-term exposure to PM10, O3, NO2, and SO2 can cause hyper coagulability and thrombosis due to adverse effects on ATPP, PT, CRP, and tissue-type plasminogen activator (t-PA), etc. which leads to CVD. PM exposure above acceptable levels in people working in photocopy shops felt very high nasal blockage and other lung infections and resulted in CVD issues. Urban air pollution exposure caused hypermia due to high levels of PM10 and PM2.5 concentrations and exaggerates the response of small arteries to cardiac ischemia. Association of PM10 and NO2 long-term exposure was reported the decrease in lung volume and airway resistance in children examined by spirometry. The comparative study of low pollution district (LPD) and high pollution district (HPD) was revealed high-risk asthma, changes in the FEV1, FEF (Forced Expiratory Flow), and other respiratory problems in children [17].
The emergency visits for asthma were strongly increased due to PM10 and PM2.5 exposure.
Particulate matter plays a vital role in the morphological change that increases the risk of non-malignant respiratory diseases and IHD. PM10 was recognized as a specific pollutant among other pollutants, which indicated a significant role in increasing COPD admissions in the winter season and asthma on warm days. Elevated levels of PM10 concentration have reported the cases of CHF. It was found that 10 μg/m3 increased by 0.72% (0.35%-1.10% at 95% confidence interval) increase the rate of admission of CHF. An association of particulate and gaseous pollutants caused blood coagulation factors like prothrombin time, activated partial thromboplastin, fibrinogen, etc. risk in women. The InterLeukin-6 expression is around 430 children were found higher with more exposure to PM2.5 (45.38 μg/m3) and PM10 (80.07 μg/m3) while TNF-alpha was reported due to PM emission through vehicles followed by pulmonary illness. The strongest association of PM10 and FVC was reported in a European study of Cohorts of Air pollution effects based on long-term air pollution levels in a standard manner. Hospital admissions of the cases of COPD in above 65-year aged patients indicated positive associations with PM10 [18].
According to emergency visits to the hospital with acute respiratory diseases in a 65-year-old female, had a higher risk of acute COPD due to association of PM10 and SO2 exposure with meteorological properties, showed prominent IQR range, i.e. 28.3 μg/m3 and 7.8 μg/m3 respectively. The concentrations of PM2.5 and PM10 in the form of Asian dust (AD) were detected by LIDAR in 231 adult asthmatic patients found with reduced lung function by PEF. The study on short-term exposure of traffic-related pollutants reported an increase in CVD and respiratory hospital admissions while long-term exposure of PM10 to middle-aged women caused a 13% increase in COPD. Even a low level of air pollutants’ association below the Environmental Protection Agency standards (PM10 & NO2) showed the association with chronic respiratory diseases in adults and a 15% increase in children’s hospitalizations. The association of air pollutants PM10, NO2, and CO caused an increase in the visits of allergic rhinitis (AR) in winters while the association of short-term exposure of PM10 and SO2 showed increased FVC and FEV1 levels. Weather variables were also found as a predictor of increasing COPD admissions.
There is no direct evidence on the effect of particulate matter on diabetes. However, the nurses living in residential places near the roadways were examined with little association and effectiveness. Around 54-55 years old women were diagnosed with subclinical inflammation added to PM related to type-2 diabetes and were observed stronger in women than men. Low socioeconomic status had a higher risk of diabetes with PM10 association. Long-term air pollution with the two-pollutant model is experimental evidence found with limited epidemiological evidence for diabetes mellitus.
PM2.5 and associated physiological diseases: The fine particulate pollutant (PM2.5) enters the deep alveoli in respiratory symptoms while the ultra-fine particles (PM1) reach into deep cellular regions and lymph nodes mix with the blood. Short-term PM2.5 (10 μg/m3) exposure led to a 13% increase in CHF admissions, the risk of ischemic stroke and cerebrovascular diseases. The association of PM2.5 and NO2 caused supraventricular tachycardia, which increases the risk of heart arrhythmia. PM2.5 emission was observed as the reason for the increased levels in urinary 8-hydroxy oxygenation concentrations in 110 inspectors at a diesel vehicle inspection station. PM2.5 effect was observed as oxidative stress in asthmatic patients with the exchange in neutrophils indicated high oxidation of plasmatic lipids causes a decrease in the defence mechanism in human blood. Traffic exposure was found to elevate endotoxin in a 1-year-old child and caused the development of allergic wheeze conditions. An increment of 10 μg/m3 in PM2.5 concentration was found associated with an increase in ERV1 based on URTI, LRT, and AECOPD. People who work on Oxford Street for 2-4 hours showed a decrease in FEV1, FVC in asthmatic individuals due to the association of diesel traffic exposure. Long-term traffic exposure of PM2.5 to a population-based study showed increased levels in CIMT (Carotid Intima Media Thickness-a marker of subclinical atherosclerosis). TNF-alpha, fibrinogen, PA-1, t-PA, Soluble platelet selctin, t-Hcy (Fasting total Homocysteine-blood markers of inflammation and blood coagulation) leads to cardiovascular and respiratory issues. The pollutant exposure to children (0-17- year) caused asthma showed stronger association in the winter season. The cases of hospital admissions due to PM2.5 associated with organic carbon were found more associated with URI and pneumonia while traffic-related PM2.5 had lagged association with asthma in children and COPD in adults. The throat diagnosis of coronary angiography indicated PM2.5 as a risk factor for stroke in residents. PM2.5 along with particle-bound Polycyclic Aromatic Hydrocarbons and 8-hydroxy-2’deoxyguanosine level caused PM-induced DNA damage and inflammatory responses in the lungs. The impact of particulate matter exposure revealed the low level of TNF- alpha, IL-10 with the association of suppression of Th1-Thr caused by allergic and autoimmune diseases in the adolescents of starazagora. Fifty-seven adult asthmatics with a source of PEF were found with the association of 5-day average PM2.5 concentration (1.3 μg/m3) and average 1.14 Lmin-1 decreased level of PEF in the evening. PM2.5 and chemical constituents like EC, OC, silicon, and sulfur, etc., were found strongly associated with increased atherosclerosis. The effect of long-term air pollution on the resident population lived nearby 50-200 m from high traffic areas has reported the decrease in the ankle-brachial index and peripheral arterial disease, especially in women. The longitudinal cohort study of survival models associated with PM2.5, an attributable factor indicated the risk of diabetes mellitus due to long-term exposure of PM2.5 while another study of 44-year aged patients reported hypertension and diabetes. PM2.5 with NO2 may increase the risk of hypertension in diabetes women obesity, CVD may be suspected to increase diabetes in non-smokers also. Long-term air pollution with the incidence of acute coronary syndrome patients had increased the risk of ST-Elevation Myocardial Infarction (STEMI) due to particulate air pollution; later on, people were at high risk of CVD. PM2.5 exposure can play a prominent role in increasing type-2 diabetes as it has adverse effects on glucose tolerance, insulin activity, and blood lipid concentration which increases diabetic activity. High levels of blood pressure and body mass index resulting from the high concentration of NO2 and PM2.5 exposure ensured a high risk of type-2 diabetes significant risk of lung cancer and respiratory diseases. The association of PM2.5 and NO2 caused high HbA1C levels, which could be a risk factor for the imbalanced glucose metabolism in diabetic patients [19].
CO and associated physiological diseases: Carbon monoxide is a poisonous gas mainly emitted from vehicles, which causes primarily severe headaches, cardiovascular problems, premature births, low birth weight in newborn babies, dizziness, etc. Increasing levels of CO concentration was correlated with decreasing BP and other health effects like headache, dizziness and slight fever, etc. The binding mechanism of CO with Haemoglobin (Hb) forms cell affinity of an oxygen molecule called hypoxemia which inhibits the oxygen-binding capacity caused gasometrical and respiratory issues. Increasing Serum Ischemia modified albumin is a diagnostic biomarker in blood COHb that showed a positive association with CO poisoning. The CO with low blood plasma concentration affects the bilirubin may cause high-risk factor for ischemic heart diseases, CAD-related diseases and arteriosclerosis, etc. which leads to high morbidity and mortality rate. CO pollution affects the Coex levels, is a simple surrogate biomarker related to wealth consequences. Coex levels were found higher in smokers than non-smokers in rural and urban areas and may associate with an increased risk of myocardial infarction, respiratory infections, and other diseases. Recent studies on the direct effect of CO on lungs are very less, however, the association of CO with other pollutants has been reported. For instance, the association of CO with NO2 and PM effects as an inflammatory with COPD, exhaled CO with MRI measures lead to increase the risk of stroke and different cardiovascular problems, metal concentration with CO causes severe diseases such as hypertension and anaemia, etc.; oxygen and CO poisoning caused cardiovascular squeals in 37% of patients. The association of outdoor pollutants mainly PM10, NO2, CO, and O3 with CVD was observed as CO (0.9 ppm for 8 hrs; 6.0%) and NO2 (5.1 ppb for 24 hrs; 6.9%) increased the risk of cardiac failure (CVD). This result indicates that a low concentration of CO shows the least effect, but with high intensity and prominent effect of COPD admissions in hospitals. The people working in various toll plazas and signals and roadside shopkeepers who were exposed to CO higher than the WHO’s permissible level were diagnosed with depression, tidiness, fatigue, forgetfulness, respiratory problems with a high pulse rate, and low oxygen levels. CO showed a significant association of North Atlantic Ocean with meteorological properties and reported with heat stress and coronary diseases which indicated a prominent risk for CVDs. The number of emergency visits under CO and NO2 exposure was associated with a 2-3% increase in COPD while other combinations of CO with O3 also reported increased COPD admissions and asthma [20].
Outdoor air pollution, mainly traffic-related pollution, increased haemorrhage stroke while another study reported acute myocardial infarction. A weak association was recorded between pollutants and cerebrovascular diseases by the two-pollutant model (CO & NO2). CO (0.1 ppm) was correlated with a 3.6% increase of IHD admissions in association with CHF and arrythrimia. Increasing distance with traffic-related air pollution reduced the mortality rate with acute HF and increased CVD mortality. Longterm and short-term air pollution showed increased inflammation by increasing ferritin and WBC counts. On warm days, CO toxicity is responsible for increasing hospitalization due to allergic rhinitis.
NO2 and associated physiological diseases: Average and peak concentrations of NO2 penetrates deep peripheral bronchi lead to mild and moderate types of asthma. High annual mean temperatures altered the interaction of NO2 exposure to ambient air increased the risk of allergic rhinitis and asthma in traffic police and roadside shopkeepers, airway resistance and induced allergic sensitization were also reported in 2 months to 4-yearold children. Asthma-related factors were also associated with hand eczema. Around 114 asthmatic children of 7-12 years, age examined due to an increase in upper respiratory infections even at relatively low levels of pollutant exposure. Increased ED asthma visits were reported due to high NO2 concentration and the effect of meteorological properties, particularly in the cold season. Diesel exhaust was seen as a source of the reduction in lung function, airway resistance, airway acidification, and neutrophilic inflammation effects in asthma patients. Exhaled nitric oxide (eNO) affected airway inflammation and other biomarkers were also observed with enhanced allergic conditions in 6-15-yearold children. Association of traffic-related PM and NO2 caused COPD mortality and lung cancer. A positive association of NO2 and pollen was observed with an increase in asthma emergency admissions. On analyzing the pollutant exposure with the two-pollutant model, the CVD effects were observed through the measurement of hsCRP (High sensitivity c-reactive protein), bow-like biomarkers which were associated with the inflammation. Lower pulmonary function was diagnosed due to increasing emissions from a local coal-fired station even in the limit of pollution standards in Hadera, Isreal [21].
The study designed by the generalized additive model used in the association of traffic-related air pollutants with hospitalization on an AMI, an 11 % increase in COPD was observed in the cold season due to NO2 exposure correlated with meteorological factors and reduced expiratory flow. Outdoor air pollution and asthma fluctuations associated with lung function with high levels of motor vehicle emissions (NO2, SO2, CO, etc.) lead to lower pulmonary function. In the morning, Fev1 measurements were found with the strong effects of pollutants like NOx and O3, which indicates lower lung function. Short-term traffic-related NO2 along with other pollutant concentrations promote cardiovascular and respiratory mortality, COPD, and lung cancer mortality. The study of short-term exposure of NO2 in association with PM10 caused acute lower respiratory infections in young children. Long-term air pollution affects living beings near major roads which are at high risk of COPD mortality. Among the lag of 0-5 days, about 3.95% increase in respiratory mortality with NO2 exposure. Traffic-related NO2 was observed as a cause of diabetes mellitus, especially in women. However, however, healthy non-smokers were also found with a high level of glucose. Around 30.6 ml lower FEV1 measurement had been identified in a large cohort study due to NO2 exposure. The number of emergency visits with NO2 and CO exposure was associated with a 2-3% increase in COPD cases. Short-term exposure of NO2 (2.67%) showed an association for increasing CVD also correlated with diabetes (3.5%). Ten Italian residents had diabetes and other chronic diseases with an increase of 10 μg/m3 NO2 exposure and type-2 diabetes diagnosis due to the traffic-related buffer (250 m) with NO2 exposure while 100 m traffic buffer caused a high risk of increasing Atherosclerosis. High levels of HbA1C and FBG were observed with 5 μg/m3 of NO2 exposure in Taiwan. Traffic-related air pollution with the PM and NO2 exposure in the association of incidence of C3c marker used in the inflammation process caused a risk of increasing diabetes. Long-term exposure to NO2 with PM is a higher risk of chronic diseases like CVD with diabetic mortality.
SO2 and associated physiological diseases: The concentration of SO2 in ambient air depends upon meteorological conditions. The risk level of SO2 is 0.3 μg/m3, which may affect human health by causing asthma, bronchitis, airway inflammation, breathing difficulties, psychiatric alterations, heart failure, circulatory collapse, etc. A spirometric air pollution monitoring program reported cough, lower respiratory illness, and bronchitis due to the exposure of TSO4, TSP, and SO2 with CO. There was 200 ppb of SO2 and 400 ppb of NO2 exposure for 4 to 6 hours, showing mild optic asthma and increased plasma viscosity in men and women with meteorological properties while Fev1, FVC and CBU (Cumulative breath units) levels decreased after exposure to combined pollutants. The heavy traffic enhances the airway response to inhaled allergies possibly as a result of airway inflammation by the combination of SO2 and NO2. The association of air pollution, especially SO2 and suspended PM caused an increase in blood pressure (1.79 mm Hg per 80 μg/m3 SO2), lipid peroxidation, which may alter antioxidant enzyme activities to sensory evoked potentials. In the coal-burning areas, the effect of PM and SO2 concentration responded on vitro and vivo relations to neuron degeneration and positively correlated with the risk of neuronal dysfunction and increased morbidity from COPD. SO2 pollution causes brain inflammation and related microvasculature dysfunction. The action of endogenous 2-AG suppresses the inflammatory-related microvasculature dysfunction. The receptors CB1 and CB2 can be used in the medication for brain injuries due to SO2 inhalation [22].
The effect of SO2 on mortality depends on temperatures except with humidity. At a minimum temperature (<20°C), the SO2 concentration may increase the COPD admissions, PC20 Methocholine may not be controlled, but reduced effectiveness of lung function increased the asthmatic conditions. Asthma ED transport visits were reported more in the cold season from 73 ppb SO2 exposure. Around 5416 Ohio Medical cases were diagnosed with about a 35% increase of asthmatic conditions correlated with 50 μg/m3 SO2 concentrations. The daily ER visits were recorded as a 6% increase in asthma and 5% of COPD correlated with ambient SO2 exposure. Early pregnancy and preconception with ambient NOx and SO2 exposure lead to an increase in the risk of Gestational Diabetes mellitus. The association of pollutants such as PM10, NO2, and SO2 with fasting blood glucose led to an increase in the FBG levels. The 10 μg/m3 SO2 exposure showed an increase in lipid levels such as total cholesterol, Triglycerides, and Low-density lipoprotein cholesterol, etc. especially in women and elderly people, which is a sign of risk of diabetes. The annual mean concentration of SO2 revealed lung cancer and respiratory mortality in Japan and cancer in Stockholm, Sweden.
Psychological diseases
Psychologically, the effectiveness of behavior is known as stress or depression. Psychological stress influences humans in two ways-the amount of sadness, self-pain, bad incidents, sad thoughts, and other emotions cause depression. Hypotension and low lipid level have been associated with depression symptoms, especially in adults. The research of air pollution on human behavior started in the 1970s; its conceptual framework for future research based on the relationship between air pollution with human behavior may vary. The high level of concentration of pollutants affects the physiological process, may cause stress. Psychological stress may act as an environmental disruptive pollutant that affects human health. However, very little research has been done on pollutants’ effect on stress and depression, but on the basis of discussion on the interactions, physiological diseases such as dementia, depression, and stress are being discussed in this section [23].
PM10 and associated psychological diseases: The increment in suicide risk showed positive correlation with the exposure of PM10 is one of the evidences of the pollutants affect caused depression. Exposure to pollutants like SO2, NO2, PM10 and CO increases the ED visits for depression with CVD, asthma and diabetes etc. Korean version of the SGDS-K (Geriatric Depression Scale) was used to measure the symptoms of depression to know the pollutant concentrations with various diseases. Some pollutants (e.g. PM10 associated with O3) have indirect effect and caused dementia. Long term pollution increases the dementia with Alzheimer’s symptoms like memory impairment and communication impairment, etc. Traffic related particulate pollution in elderly people shows the symptoms to become transition state between aging with dementia and Mild Cognitive Impairment. Air pollution causes acute epidemiologists stress by increasing psychological disorders. Urban pollutants affect the plasma levels and Adrenocarticotropic hormone (ACTH) which promotes psychosocial stress in non-smoking police officers. Effect of ambient pollutants influences suicide risk in low educated, white collar and married people. Association of traffic exposure with APOE decreases in cognitive impairment.
PM2.5 and associated psychological diseases: The depression was noticed in large population-based nurses, due to the impact of PM2.5 at 0-45 depression scales. A positive correlation was observed between long-term exposure to PM2.5 and socioeconomic stress, which signified the symptoms of psychological diseases like moderate to severe anxiety and depression. Another study proved the positive association of PM2.5 exposure with stress, even by controlling age, gender, demographic, and socioeconomic health status. Stress toxicants can influence disease risk in immune function, lung structure, and its function, etc. Asthmatic children were identified with stress by measuring blood markers (IgE, interleukin-5, interaction beta, etc.) which indicated higher chronic stress. Social environmental status (SES) reflects poor asthmatic conditions. The highest level of stress was associated with chronic stress and statistically evidenced with the pathways between SES and immune response in children having asthma. The national life, Health, and Aging project observed the association of air pollutant exposure with erectile dysfunction (a sign of psychological stress) in old age people. Air pollution enhanced the psychosocial, environmental stresses with an increased risk of CVD. Around 6.7% of dementia was diagnosed in 67 older aged people with PM2.5 exposure. Individuals with CVD disease due to PM2.5 exposure associated with a 10.1% increase in stressful suicide risk. Air pollution with a positive association of poor cognitive function may intend to a high risk for dementia.
CO and associated psychological diseases: CO exposure also increases the risk of dementia, substantiate with the study of vehicular exposure of NO2 and CO with an increase of dementia cases in Taiwanese. High levels of diesel exhaust exposure to pollutants reported the symptoms of acute psychological stress. An association of HBO2 (Hyperbaric Oxygen) with CO exposure resulted in the declination in cognitive behavior. ED visits were associated with a correlation between CO concentrations and meteorological factors. Indoor CO exposure increased depressive symptoms in rural women because the emission from kerosene stoves was found to be associated with higher cognitive impairment even at a low level of acute CO poisoning. A 43-year-old woman was diagnosed with cognitive impairment due to CO exposure.
NO2 and associated psychological diseases: From a neurological point of view, parasympathetic activity can cause inflammation. High concentrations of pollutants may cause psychological stress due to imbalance in different lifestyles. The pollutants’ concentrations (PM2.5, PM10, and NO2) were correlated with the depressed mood of the people through validated questionnaires that showed the effect of pollution on psychological diseases. Females were found with higher levels of depression than males due to NO2 and SO2 exposure. Each 10 μg/m3 level of NO2 increased the odds ratio of depression of 2:00 (95% CI; 1.37, 2.93) ranking with the use of antidepressants. In a chemical analysis of the population-based survey, dementia was diagnosed with the effect of NO2 and CO exposure. Parental stress is an outcome of NO2 exposure without smoking habit, which may lead to a decrease in lung function. Increased temperatures along with increasing ambient NOx concentrations caused the risk of suicide in Guangzhou, China. Even low-level pollutant concentrations would have increased the psychiatric admissions along with the increased risk of suicide distress due to exposure to gaseous pollutants. The lower cognitive decline was associated with O3, NO2, and PM2.5 concentrations in which NO2 exposure is inversely proportional to logical memory abilities. The mental development (prenatal/postnatal periods) in infants was affected with NO2 with Benzene exposure.
SO2 and associated psychological diseases: The long-term and short-term effects of low levels of SO2 exposure correlated with chronic stress. The history revealed the mood distortions and stress followed by its impact on physiological systems. Short-term exposure to air pollution affected the person suffering from physiological diseases, and they had a high risk of depressive mood. The exposure to high levels of SO2, NO2, and PM10 to the pregnant women found with high levels of depression scores (i.e., P.-75-100) showed severe depression in cold weather. The linking mechanism of the air pollutant levels on suicide mortality increases the chances of depression. PM2.5, BC, and SO42- concentrations were reported as higher Perceived stress scale (PSS) which is a marker of increasing depression and stress in people. The effect of air pollution between prenatal and postnatal was associated with parental stress, which increases childhood asthma. High levels of pollutant exposure to >30 years of age were found with increased stress and suicide mortality. Recently, a case of cognitive disorder was observed after the surgery, which is a sign of increasing dementia [24].
Characteristics of Study Objects
There was a total of 369 papers were accessed for conducting this review study. After exclusion of papers that were either repeated/ old information (n=60) or the study period was unknown (n=02), research papers remained 307. Out of which, 60 papers were excluded for missing data on age, sex, mortality regarding physiological diseases (CVD, COPD, Asthma, Diabetes, and Cancer) and 07 for psychological diseases (Dementia, Depression, and Stress). In this way, only 240 papers were found eligible to consider for this review. Records of (1997-2019) years across the globe with an insufficient number of included individuals were also excluded (n=22). The remaining 7781054 patients were included in the study. A cohort for the primary outcome, 2754056 patients had a valid record of physiological diseases and psychological diseases (with pollutants concentration and age), whereas methodology and results for physiological diseases (2088092) and psychological diseases (665975) included in the study of functional outcome. A detailed flow diagram is presented in Figure 1.
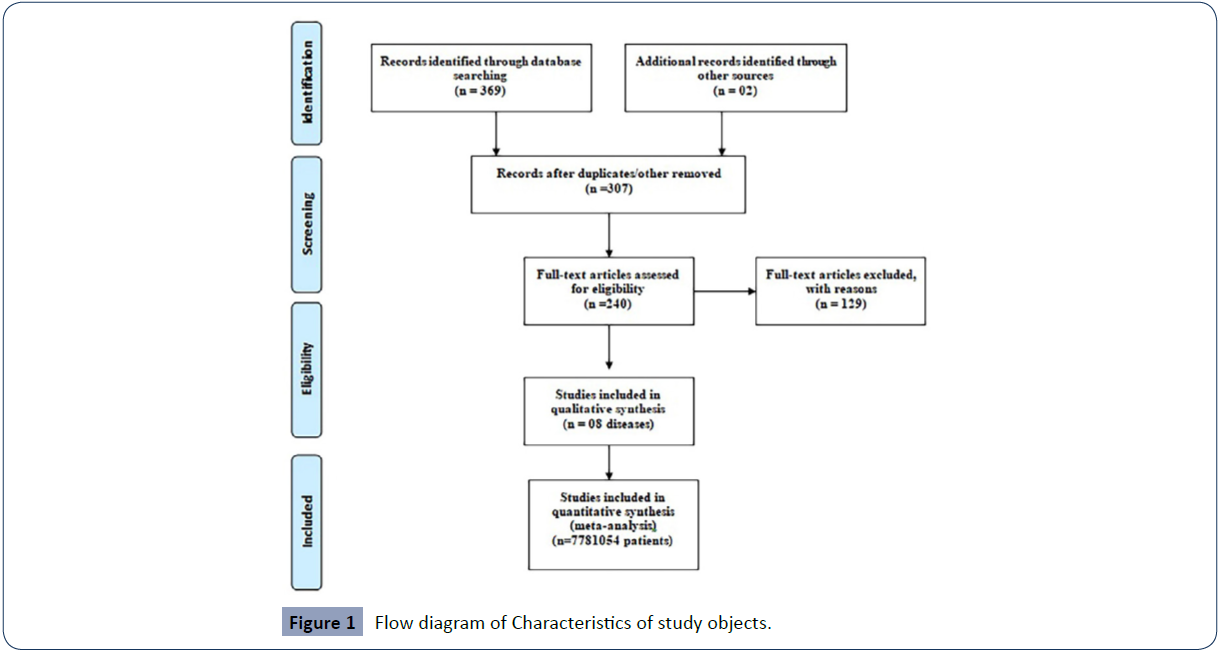
Figure 1 Flow diagram of Characteristics of study objects.
Interpretation of systematic evidences by the authors
The present study is based on the interpretations of>360 peer-reviewed research papers from international journals (all references are not mentioned in this paper). Out of which 40-50 research papers belong to each pollutant (PM2.5,PM10,CO,NO2&SO2) and associated physiological diseases (CVD,COPD, asthma, diabetes & Cancer) along with psychological diseases (dementia, stress & depression). A general review of air pollution and its health effects indicated two main groups of diseases, physiological diseases, and psychological diseases. Physiological diseases may occur either from direct or association of pollutants exposure. On the other hand, psychological diseases are caused by direct and combined with the pollutants exposure or as a consequence of physiological diseases. The pollutant may affect directly or indirectly endocrine glands, which spoils the hormonal system and leads to neuropsychological diseases. The short-term and long-term effects of pollutants on mortality and morbidity have also been discussed. Trends were analyzed for pollutants’ concentration levels over the years, associating pollutants with different diseases and age-wise effect of diseases.
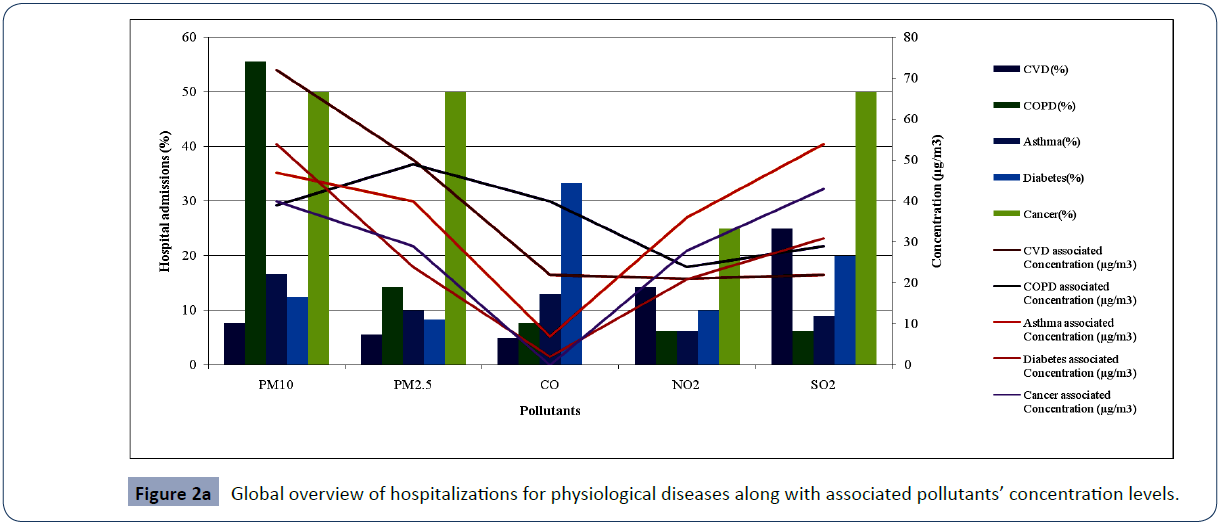
Figure 2a gives a global overview of the diseases caused due to direct and indirect exposure to the pollutants. The Largest hospitalizations of COPD (>50%) are caused by PM10 followed by >15% cases due to PM2.5 exposure. Both types of particulate matter (PM10 & PM2.5) and SO2 are responsible for almost 50% of cases of cancer. The fourth highest disease is diabetes as >30% cases are observed due to CO exposure. For the cases of asthma, almost all five pollutants are accountable, but PM10 is the main contributor (15% cases) and SO2 is the main contributor for CVD hospitalizations (>20%).
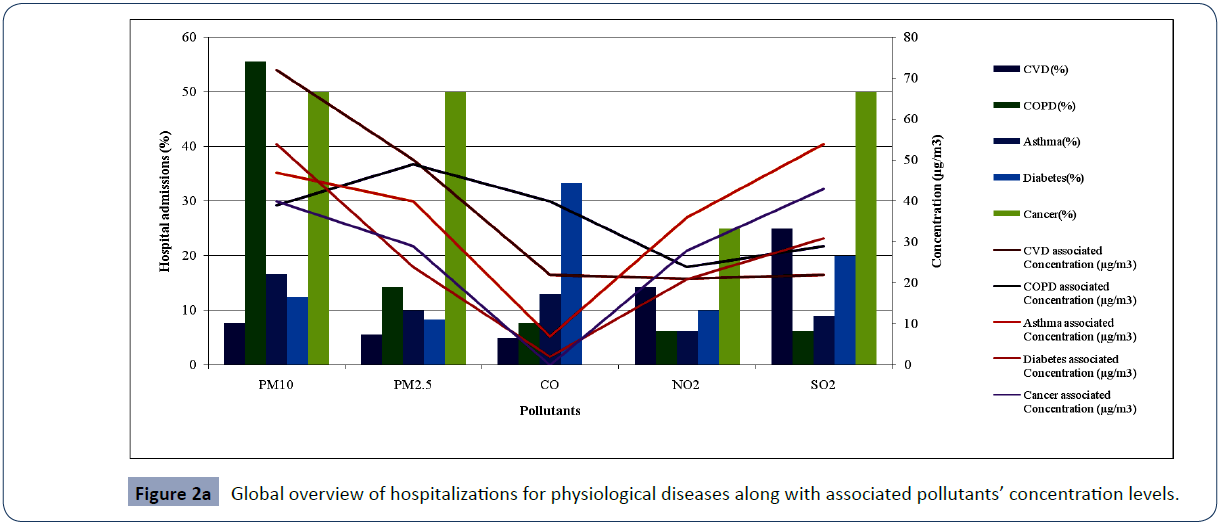
Figure 2a Global overview of hospitalizations for physiological diseases along with associated pollutants’ concentration levels.
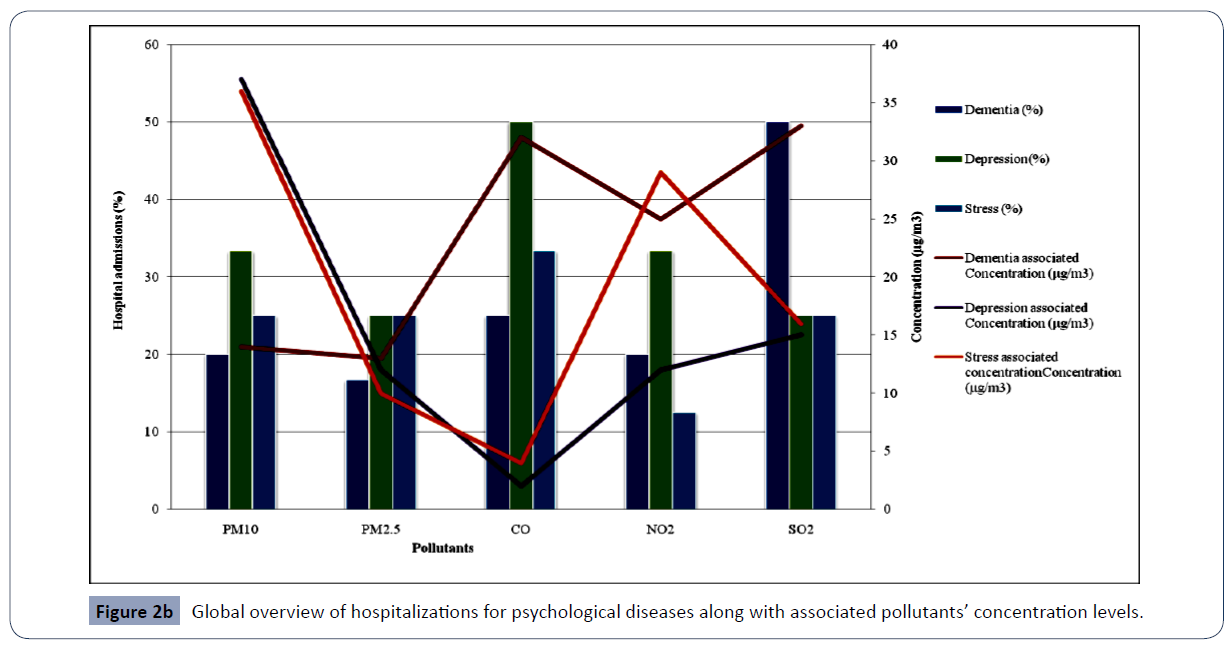
Figure 2b illustrates the pollutants’ effects on hospital admissions of psychological diseases with the direct and indirect association of other diseases. The CO and SO2 are the main contributors to the increasing admissions of dementia (≤50%). CO is the prime pollutant that causes the maximum number of psychological diseases’ admissions of depression. PM2.5 and SO2 are the second-largest contributors to depression (25%). PM10 is the main pollutant concentration that causes nearly 40-50% of psychological diseases. PM2.5 (15%) is the least contributor to increasing psychological diseases. Stress was increased by PM10 (40%), NO2 (30%) and SO2 (≤20%) concentrations. CO and SO2 are the main pollutants that cause a maximum percentage of dementia. NO2 is the second largest contributor to depression.
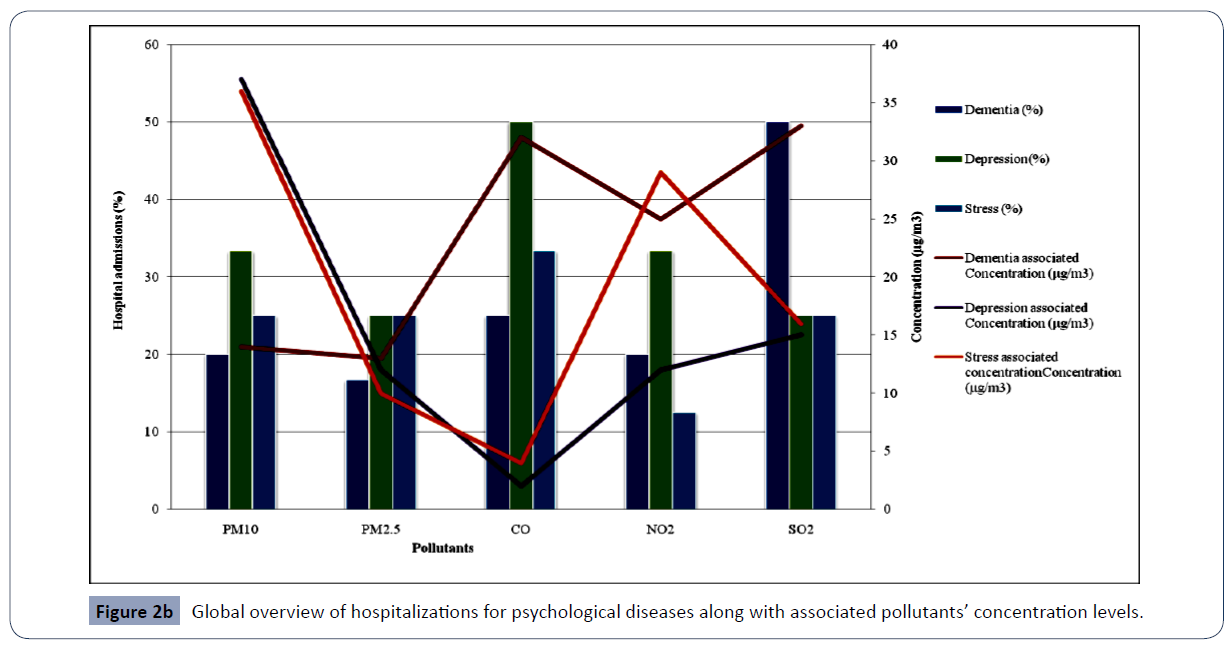
Figure 2b Global overview of hospitalizations for psychological diseases along with associated pollutants’ concentration levels.
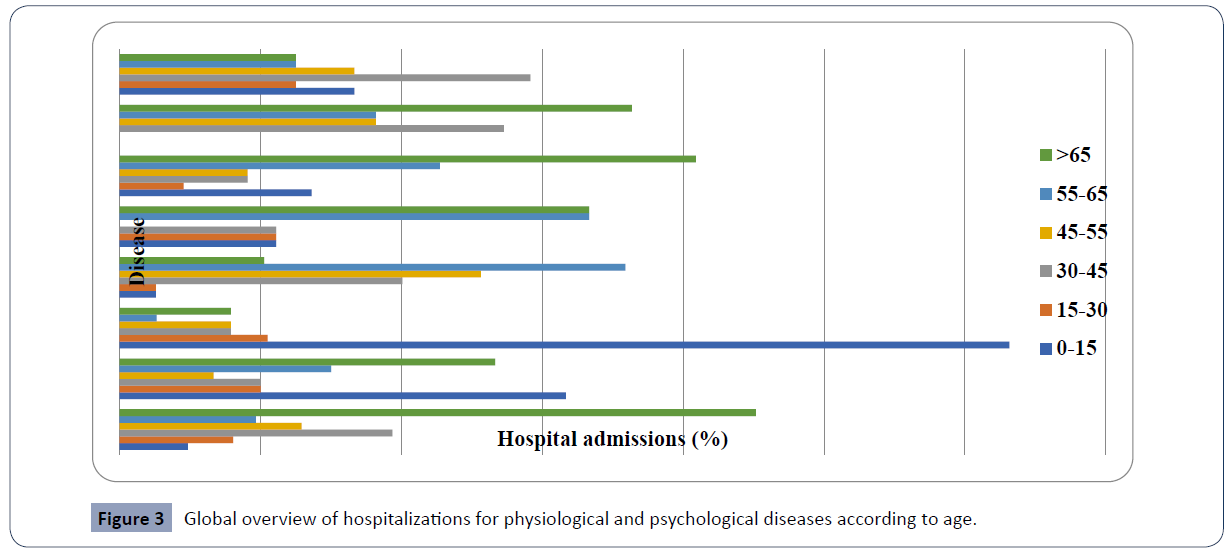
Age is one of the important factors of increasing its effectiveness. Figure 3 reflects the causing capacity of different age groups. The age group of ≤ 15 years is very sensitive mainly for asthma (60%) followed by the cases of COPD (30%) and cancer (10%). Except for diabetes, all diseases are prominent in the adult group, i.e., the 15-30-year age group; however, diabetes (35% in 55-65 age groups) and CVD (45% in above 65 years) are the most abundant diseases after 30 years. The cases of cancer (35%) have been observed at the age of ≥ 65 years.
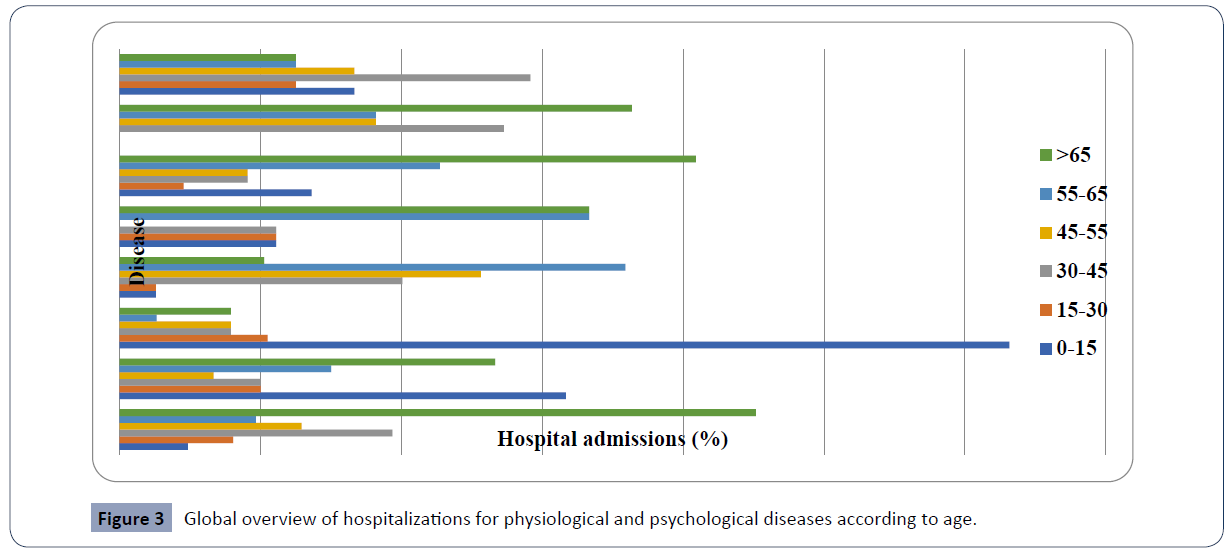
Figure 3 Global overview of hospitalizations for physiological and psychological diseases according to age.
Psychological diseases affect the age above 65 years. Dementia is the main disease that occurs (≤50%) above 65 years of age [25]. The age group of 30-45-year is the first highest age group for increasing stress while depression occupies the highest percentage above 65 years of age group, continuously reducing the effects above 45-year. Stress affects around 30-45-year and it was observed that stress level is decreasing as increasing the age (45<55<65<65 above).
Conclusion
The hypothesized analysis of different pollutant concentrations upon different causing diseases is a clue for further studies on different aspects. The analysis of different age groups with pollutant-associated diseases gave an overview to identify the intensity of diseases on susceptible groups. Among all pollutants, CO shows less effectiveness on cancer and CVD while NO2 is represented as a prominent factor for COPD hospitalizations for physiological diseases. Based on the concentrations, there is enough study done on the effect of PM10 and PM2.5 pollutants. However, the effects of pollutants on psychological diseases need more rigorous studies on decisive health effects.
38698
References
- Abe T, Tokuda Y, Ohde S, Ishimastsu S, Nakamura T, et al. (2009) The relationship of short-term air pollution and weather to ED visits for asthma in Japan. Am J Emerg Med 27: 153-159.
- Abelsohn A, Margaret D, Barry S, Jessiman J, Weir E (2002) Identifying and managing adverse environmental health effects: 6. Carbon monoxide poisoning. CMAJ 166: 1685-1690.
- Adams WC, Brookes KA, Schelegle ES (1987) Effects of NO2 alone and in combination with O3 on young men and women. J Appl Physiol 62: 1698-1704.
- Ailshire JA, Crimmins EM (2014) Fine particulate matter air pollution and cognitive function among older US adults. Am J Epidemiol 180: 359-366.
- Alderete TL, Habre R, Toledo-Corral CM, Berhane K, Chen Z, et al. (2017) Longitudinal associations between ambient air pollution with insulin sensitivity, β-cell function, and adiposity in Los Angeles Latino children. J Diabetes 66: 1789-1796.
- Alessandrini ER, Stafoggia M, Faustini A, Berti G, Canova C, et al. (2016) Association between short-term exposure to PM2.5 and PM10 and mortality in susceptible subgroups: a multisite case-crossover analysis of individual effect modifiers. Am J Emerg Med: 1-11.
- Allard G, Nelson CJ, Pallardy SG (1991) Shade effects on growth of tall fescue: II. Leaf gas exchange characteristics. Crop Sci 31: 167-172.
- Almendra R, Santana P, Vasconcelos J, Silva G, Gonçalves F, et al. (2017) The influence of the winter North Atlantic Oscillation index on hospital admissions through diseases of the circulatory system in Lisbon, Portugal. Int J Biometeorol 61: 325-333.
- Alwahaibi A, Zeka A (2016) Respiratory and allergic health effects in a young population in proximity of a major industrial park in Oman. J Epidemiol Community Health 70: 174-180.
- Anand JS, Schetz D, Waldman W, Wiśniewski M (2017) Hyperventilation with Maintenance of Isocapnia. An Old New Method in Carbon Monoxide Intoxication. PloS One 12: e0170621.
- Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, et al. (2012) Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes care 35: 92-98.
- Annesi-Maesano I, Baiz N, Banerjee S, Rudnai P, Rive S, SINPHONIE Group (2013) Indoor air quality and sources in schools and related health effects. J Toxicol Environ Health B Crit Rev 16: 491-550.
- Arbex MA, de Souza GM, Cendon SP, Arbex FF, Lopes AC, et al. (2009) Urban air pollution and chronic obstructive pulmonary disease-related emergency department visits. J Epidemiol Community Health 63: 777-783.
- Arena VC, Mazumdar S, Zborowski JV, Talbott EO, He S, et al. (2006) A retrospective investigation of PM10 in ambient air and cardiopulmonary hospital admissions in Allegheny County, Pennsylvania: 1995–2000. J Occup Environ Med 48: 38-47.
- Al-Awadi L (2018) Assessment of indoor levels of volatile organic compounds and carbon dioxide in schools in Kuwait. J Air Waste Manag Assoc 68: 54-72.
- Bauer M, Moebus S, Möhlenkamp S, Dragano N, Nonnemacher M, et al. (2010) Urban particulate matter air pollution is associated with subclinical atherosclerosis: results from the HNR (Heinz-Nixdorf-Recall) study. J Am Coll Cardiol 56: 1803-1808.
- Bell ML, Davis DL (2001) Reassessment of the lethal London fog of 1952: novel indicators of acute and chronic consequences of acute exposure to air pollution. Environ Health Perspect 109: 389-394.
- Berger A, Zareba W, Schneider A, Rückerl R, Ibald-Mulli A, et al. (2006) Runs of ventricular and supraventricular tachycardia triggered by air pollution in patients with coronary heart disease. J Occup Environ Med 48: 1149-1158.
- Biswas J, Upadhyay E, Nayak M, Yadav AK (2011) An Analysis of Ambient Air Quality Conditions over Delhi, India from 2004 to 2009. Atmospheric and Climate Sciences 1: 214-224.
- Bono R, Piccioni P, Traversi D, Degan R, Grosa M, et al. (2007) Urban air quality and carboxyhemoglobin levels in a group of traffic policemen. Sci Total Environ 376: 109-115.
- Bowe B, Xie Y, Li T, Yan Y, Xia H, et al. (2018) The 2016 global and national burden of diabetes mellitus attributable to PM2.5 air pollution. Lancet Planet Heal 2: e301–e312.
- Briet M, Collin C, Laurent S, Tan A, Azizi M, et al. (2007) Endothelial function and chronic exposure to air pollution in normal male subjects. Hypertension 50: 970-976.
- Çapraz Ö, Deniz A, Doğan N (2017) Effects of air pollution on respiratory hospital admissions in İstanbul, Turkey, 2013 to 2015. Chemosphere 181: 544-550.
- Carson JL, Collier AM, Hu SC, Smith CA, Stewart P (1986) The appearance of compound cilia in the nasal mucosa of normal human subjects following acute, in vivo exposure to sulfur dioxide. Environ Res 42: 155-165.
- Chang KH, Chang MY, Muo CH, Wu TN, Chen CY, et al. (2014) Increased risk of dementia in patients exposed to nitrogen dioxide and carbon monoxide: a population-based retrospective cohort study. PloS One 9: e103078.