Keywords
Diabetic neuropathy, diabetes mellitus, health related quality of life
Introduction
The prevalence of type 2 diabetes mellitus (T2DM) in Greece increased significantly, from 8.7% in 2002 to 10.3% in 2006. The age-adjusted prevalence of diabetes among adults was 8.2% (men, 8.5%; women, 7.8%) in 2002 and 9.5% (men, 9.7%; women, 9.3%) in 20061. These findings show that the prevalence of diabetes is rising rapidly in the Greek population and appears to be increasing in parallel with prevalence of obesity [1]. Worldwide the number of patients with T2DM is expected to increase dramatically from about 3.2 million last year (8.8% of the national population) to about 4.25 million (11.1%) over the next 19 years. [2] This enormous increase in the number of T2DM patients will certainly be accompanied by chronic diabetic microvascular or macrovascular complications. Diabetic peripheral neuropathy (DPN) is the most prevalent and troublesome complication in patients with diabetes mellitus (DM), causing morbidity with significant impact on the quality of life of the person with diabetes, and can result in early death [3].
he prevalence of type 2 diabetes mellitus (T2DM) in Greece increased significantly, from 8.7% in 2002 to 10.3% in 2006. The age-adjusted prevalence of diabetes among adults was 8.2% (men, 8.5%; women, 7.8%) in 2002 and 9.5% (men, 9.7%; women, 9.3%) in 20061. These findings show that the prevalence of diabetes is rising rapidly in the Greek population and appears to be increasing in parallel with prevalence of obesity [1]. Worldwide the number of patients with T2DM is expected to increase dramatically from about 3.2 million last year (8.8% of the national population) to about 4.25 million (11.1%) over the next 19 years.[2] This enormous increase in the number of T2DM patients will certainly be accompanied by chronic diabetic microvascular or macrovascular complications. Diabetic peripheral neuropathy (DPN) is the most prevalent and troublesome complication in patients with diabetes mellitus (DM), causing morbidity with significant impact on the quality of life of the person with diabetes, and can result in early death [3].
Diabetic neuropathy (DN), which may be focal or diffuse, is diagnosed when diabetic patients complain of symptoms and/ or show signs of peripheral nerve dysfunction after the exclusion of other etiologies [3]. Chronic sensorimotor DPN is the most common form of DN.3-5 A major symptom in DN patients is pain arising as a direct consequence of abnormalities in the peripheral somatosensory system in people with diabetes [4].
The symptoms can be present as severe numbness, paresthesia, or hyperesthesia, however, DPN may be asymptomatic in about 50% of patients [5] and as the DPN progresses, the painful symptoms usually disappear although they have a substantial impact in quality of life (QoL) [6,7].
In addition, DPN is also associated with substantial morbidity, which includes mostly susceptibility to foot or ankle fractures and ischemic ulceration leading to lower-limb amputations, [9,10] but also depression [8]. Considering the fact that painful symptoms in DPN have also a significant negative effect on QoL as the condition limits daily activities and interferes with sleep, there is a need for regular evaluation of health related quality of life (HRQoL) in patients with DN. [9,10] Since preventive strategies and patient education still remain key factors in reducing complication rates and mortality, measurement of HRQOL is crucial for the future treatment plan of these patients [3]. If we take into consideration that in a recent study [11] of patients with diabetes and chronic painful peripheral neuropathy (CPPN), 12.5% of study participants had never reported their symptoms to their treating physician and 39.3% had never received any treatment for their painful symptoms, it is quite evident why the health care providers should include evaluation of HRQoL as a regular procedure for every patient. Moreover, the guidelines for treatment of Type II DM emphasize that one of the primary objectives is to improve HRQoL. [11] The two major approaches to measuring HRQoL are generic and disease-specific instruments, and the two have been compared [12] in diabetes patients and shown to demonstrate complementarity and provide different kinds of information, with the generic ones perhaps providing more information than their disease-specific counterparts [13].
So the aim of the present study was to identify significant disease-specific and sociodemographic predictors of DN in patients with T2DM, with a small, validated, multidimensional instrument (SF-12) since up to day QoL in these patients has only been assessed through T2DM patients [14] facing DN as a complication only, and not as a very important situation with a major effect in QOL.
Methodology
Patients
The study design was prospective. A random sample of 64 patients with DN, attending two outpatients clinics (2nd Department of Internal Medicine, Research Institute & Diabetes Center, School of Medicine, University of Athens ''Attikon” University Hospital and in 3rd Department of Internal Medicine and Diabetes Center, General Hospital of Nikaia) were enrolled, from June 2011 to July 2012. The selection of the specific hospitals was based on the fact that they represent the current clinical practice, since they are two of the major hospitals in Greece, treating a large number of diabetic patients. Five of the study participants were excluded; two who could not read and write in Greek language, one was under treatment for breast cancer and two who were under treatment for psychosis. Additional excluded criteria were: living in a nursing home, cognitive or mental illness, cancer under treatment and hospitalization during the evaluation of fatigue. Finally, of the 59 patients enrolled, six did not return the questionnaires., therefore 53 patients completed the study.
The study protocol was approved by the Scientific and Ethical Committee of the Attikon University Hospital and the General Hospital of Nikaia and the procedures followed were in accordance with the Helsinki Declaration [15]. All patients who were willing to participate completed an informed consent form, and all responses were anonymous.
Procedures
Demographic and clinical data were collected by subject’s medical records. Diabetic neuropathy was diagnosed according to the American Diabetes Association criteria [16], using tests such as pinprick sensation, vibration perception (using a 128-Hz tuning fork), 10-g monofilament pressure sensation at the distal plantar aspect of both great toes and metatarsal joints, and assessment of ankle reflexes. Glycemic control was assessed by glycosylated hemoglobin (HbA1c), performed during the last three months from the evaluation of fatigue. Hematocrit (Ht) and white blood cells (WBCs) were also evaluated.
Psychometric Measurements
Health related quality of life was evaluated using the SF-12, a short form of the SF-36 questionnaire consisting of 12 questions (with score ranging between.0 to 100 and a cut off point of 50). The authors have consequently suggested that a 12-item sub-set of the original 36 items of the SF-36 can be used to construct a shorter health survey [17]. All 12 items were used to calculate the physical and mental component summary scores (PCS12 and MCS12), by applying a scoring algorithm empirically derived from the data of a US general population survey [18].
The Michigan Neuropathy Screening Instrument (MNSI) was used to record neuropathic symptoms [19], as a rapid, simple and reliable test for screening DPN in both diabetes clinics and epidemiological surveys (with score ranging between.0 to 6) [20]. The Greek questionnaire was validated on a sample of 173 people, 99 women and 74 men, aged 25-85 years (M = 65,2 ± 11,7), with diabetes type 1 and 2, and mean duration of diabetes 14.1 years, of whom 33 were diagnosed with peripheral neuropathy. The Greek questionnaire was created with forward and backward translation from the English version according to the instructions of the MAPI Research Institute. For the validation the characteristics of the score were compared with the generally accepted scale of diabetic neuropathy score (DNS). The scale had a good internal consistency (cronbach’s α =.832). The correlation between the 2 scales diagnosing neuropathy was very high (r = .830 p = .000). The questionnaire indicated a good discriminant validity since significant differences were found among people with diabetes (MO = 0.51 ± 0.6) and coexisting neuropathy (MO = 2.32 ± 1.3) (Mann Whitney U = 7.85 p =, 0001). The scale has a sensitivity of 0.63 and specificity of 0.97 for scores > 2 and 0.78 and 0.95 for scores> 1.5 respectively [21].
States of depression, anxiety and stress was assessed with the Depression Anxiety Stress Scale (DASS-42) [22], which is a quantitative measure of distress on the basis of three subscales of depression, anxiety (e.g, symptoms of psychological arousal), and stress (e.g., cognitive, subjective symptoms of anxiety). We used the Greek validated version of DASS-42 with scoring ranging from 0 to 126, with higher scores indicating negative emotions existence [23].
Comorbidity of depression was made by a psychiatrist and a psychologist according to the diagnostic statistical manual (DSM-IV) criteria [24].
Fatigue was assessed with the Multidimensional Fatigue Inventory (MFI) [24]. The MFI was developed as a tool to assess fatigue in a comprehensive way, with a special interest in fatigue as experienced by patients. The questionnaire has five subscales measuring general fatigue, physical fatigue, reduced activity, reduced motivation and mental fatigue. We used the Greek validated version of the questionnaire with scoring ranging from 20 to 100, with higher scores indicating more symptoms of fatigue [25].
Finally, pain was assessed using a ‘pain scale’ consisting of a blue-red plastic rule graduated in 11 points labeled 0–10, along with a red pointer slides revealing a red bar. Respondents were asked to move the slider to a point corresponding to ‘your pain at its worst in the last month’ and at the present moment. Respondents were told that a rating of ‘0’ denoted ‘no pain at all’ while a ‘10’ was ‘pain so severe as to prohibit all activity; the worst pain you can imagine’. Scores were then transferred by the interviewer to an 11-point (0–10), 10 cm visual analogue scale (VAS) labeled ‘0’ and ‘10’ at opposite ends. This was later coded to an integer from 1 to 10 for each question.
Covariates
Participants were requested to provide information on household income (0-1000 Euros, 1001-2000 Euros or more than 2000 Euros), education level (primary, secondary, tertiary), current job status (employed or not), marital status (married or single), smoking status (yes or no), frequency of alcohol consumption per week (more than or less than twice per week) and reduction in social activities (none, medium, severe). Participants also reported whether they had ever had co-morbidities including, hypertension, coronary artery disease (CAD), retinopathy, cerebrovascular disease, chronic kidney disease (CKD), musculoskeletal disorders, thyroid disease and comorbidity of depression.
Statistical analysis
Descriptive and inferential statistics were conducted by using SPSS version 17.0. Data analyses involved descriptive statistics in order to calculate frequencies, means and standard deviations for each variable. Analyses of the relationship between independent variables and HRQoL were performed to establish those variables associated with HRQoL.
Differences between subjects with DN in T2DM were examined by using independent samples t-test for continuous variables (e.g. physical fatigue, general fatigue, reduced activity, reduced motivation, mental fatigue, anxiety, depression, stress). R coefficients were used to determine the associations between the continuous variables. Bivariate analyses (t-tests, ANOVA and Pearson's and Spearman's correlation coefficients as appropriate) were then performed to evaluate the relationships between independent variables and the two main domains of the SF12, the PCS12 and MCS12. Those independent variables that were associated with a dependent variable in bivariate analyses with a p value <0.05 were subsequently included in linear multiple regression analyses to determine independent predictors.
Two separate linear regression analyses were conducted to examine the effects of fatigue, depression, anxiety, stress, optimism and sociodemographic characteristics on each of the two main domains of SF12. Variables were entered into the model when the significance level of their F value was less than 0.05 and variables were removed when their level was greater than 0.10. A total of 2 models of multivariate linear regression analysis have been created.
Results
Sample
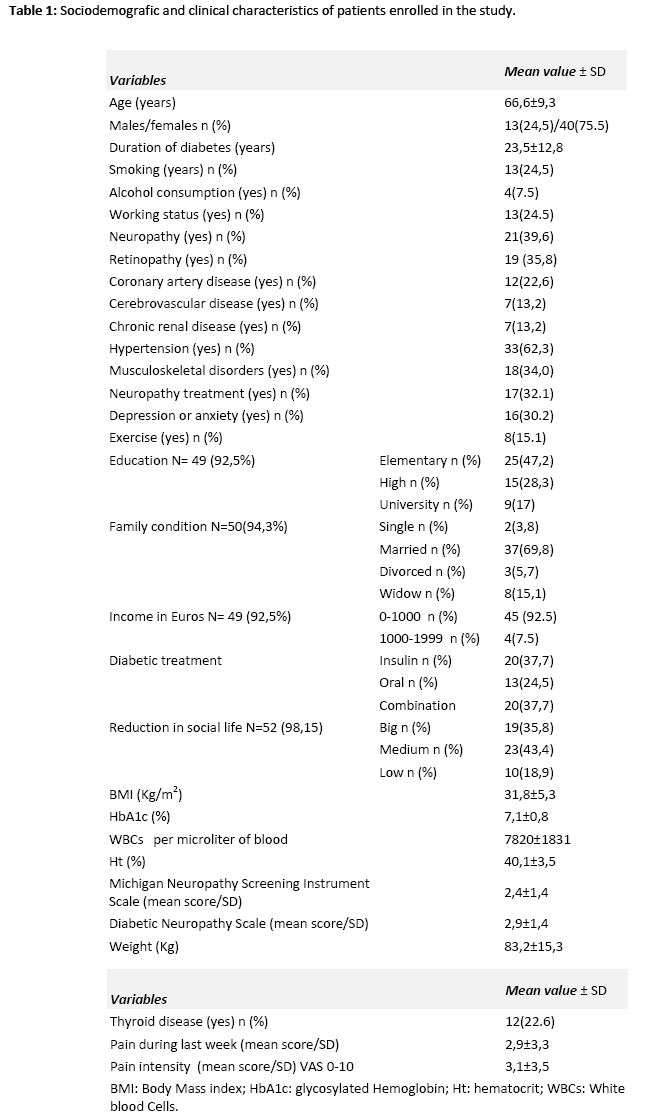
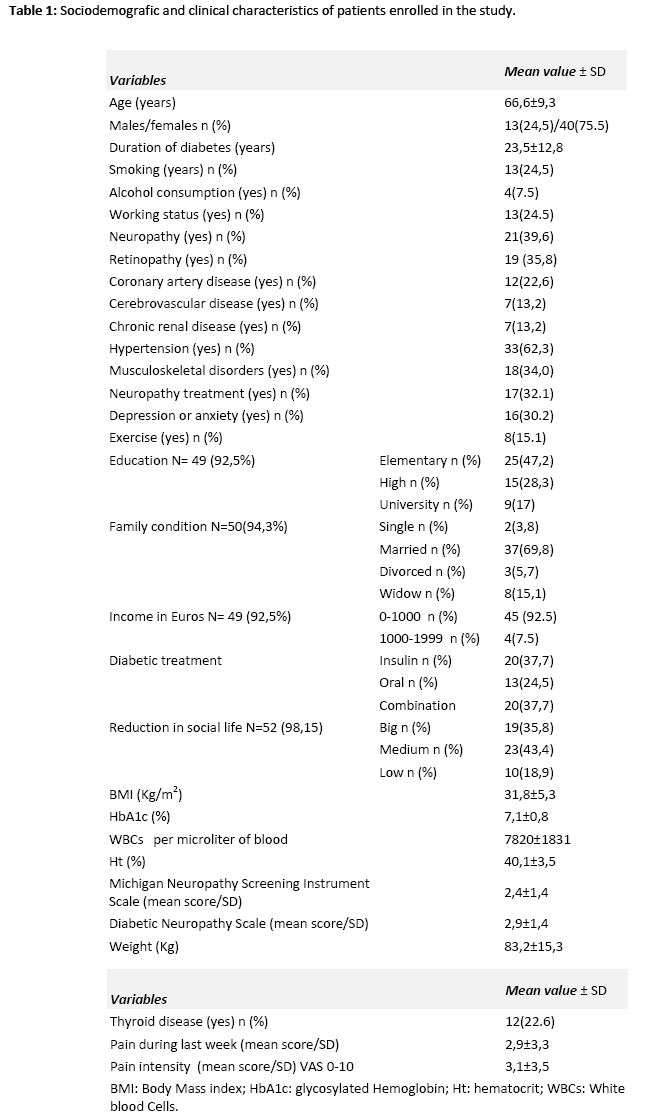
Out of the 64 patients who could participate, 53 (Ν=53) returned the complete battery to the researchers (82.81% response rate). The sample consisted of 13 males (24.5%) and 40 females (75.5%) with age (± SD) 66.6 ± 9.3 years, duration of DM 23.5±12.7 years and HbA1c 7.1 ±0.8%. Of the study participants, 93.4% were obese (BMI> 25kg/m2), 69.3% were married, 51.0% had low education, 24.5% were current smokers and 75.0% were not on permanent work at the time of inclusion. MNSI and the DNS were 2.4±1.4 and 1.9±1.4, respectively. Sociodemographic and clinical characteristics of study participants are presented in Table 1.
Descriptive analysis and correlations
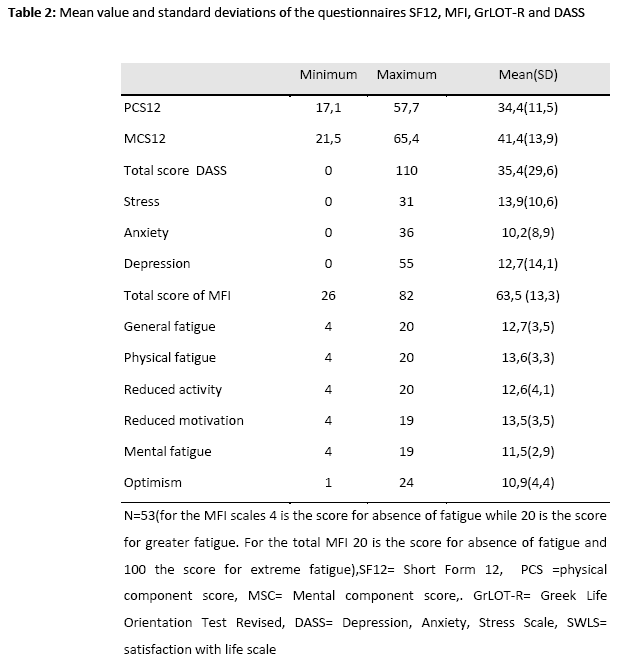
The mean value and SD of Sf-12, PCS (0-100) and MCS (0-100) as well as the MFI and the five subscales, depression, anxiety, stress, optimism, and life satisfaction are presented in Table 2. As outlined in Table 2, PCS12 (34.4 ± 11.5) and MCS12 (41.4 ± 13.9) were both lower from the normative data of the healthy Greek population (50 ± 10 for both scores) [25].
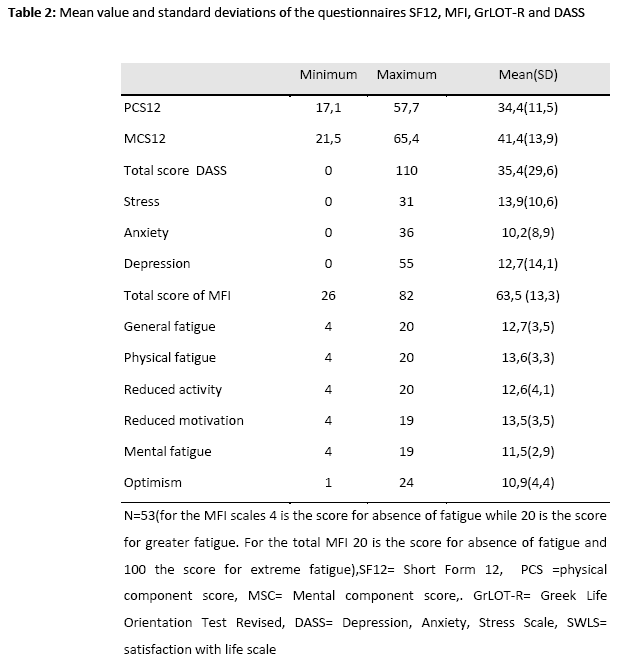
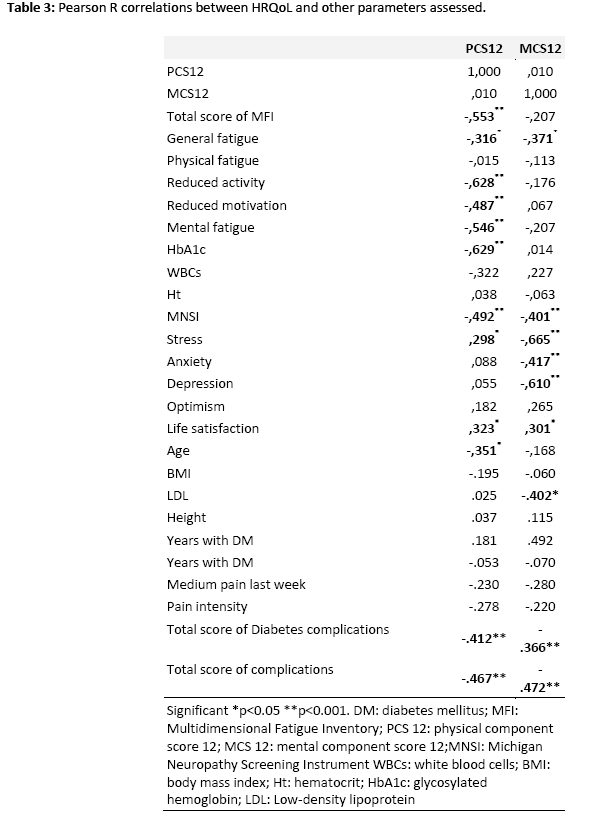
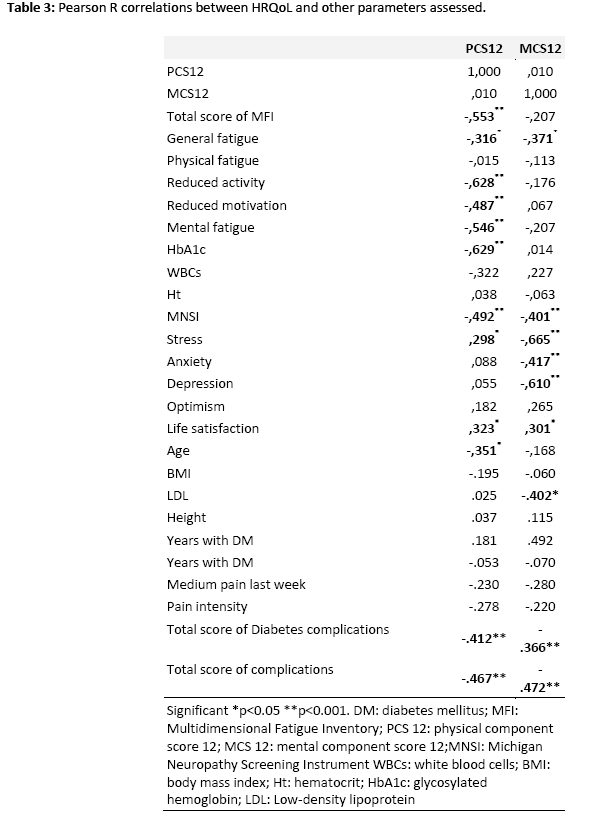
Table 3 presents correlations for age, fatigue, physical (PCS12) and mental (MCS12) composite scores of SF12, medium pain scores, complications summary scores, WBC, HbA1c, Ht and satisfaction with life. Both PCS12 and MCS12 were significantly (p<0.001) correlated with general fatigue (r=-.316 and -.371 respectively p<.05), MNSI (r=-.492 and -.401 respectively, p<.001), total score of diabetic complications (r=-.412 and -.366 respectively, p<.001), and summary score of all complications (r=-.467 and -.472 respectively, p<.001). There were seven significant negative correlations between the PCS12 and age, general fatigue, reduced activity and motivation, mental fatigue HbA1c (p<.05), and one positive correlation with stress (Τable 3). For the MCS12, there were only three other negative significant correlations with stress, anxiety and depression (p<.05) and a positive correlation with life satisfaction (p<.05) (Τable 3).
Testing for control variables
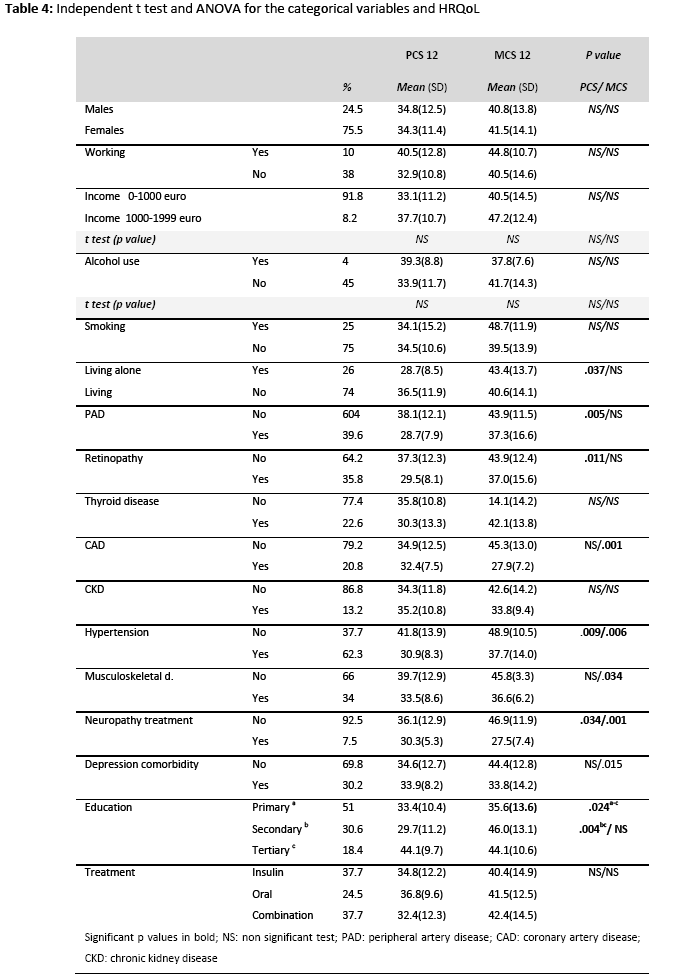
The extent to which demographic variables (age, education, marital status, employment status), and medical variables (such as PAD, retinopathy, thyroid disease, musculoskeletal disorders and other complications) were related to outcome variables was assessed, thus determining the need control for these variables in the main analyses. The significant associations with the study outcome variables that emerged from the t-test and ANOVA analyses are shown in Table 4. Living alone was negatively associated with PCS12 (t = -2.147, p < 0.05) PAD, retinopathy, hypertension and neuropathy treatment were positively associated with PCS12 (tPAD = 2.983, tretinopathy = 2.387, thypetension = 2.902, and ttreatment = 2.187 respectively p < 0.05). CAD, hypertension, musculoskeletal disorders, treatment and depression co-morbidity were positively associated with MCS12 (t= 5.715, t=2.857, t=2.364, t=6.913 and t=2.525 respectively, p<0.05). There were no other significant differences between composite scores of SF12 and demographical characteristics or smoking status and alcohol consumption.
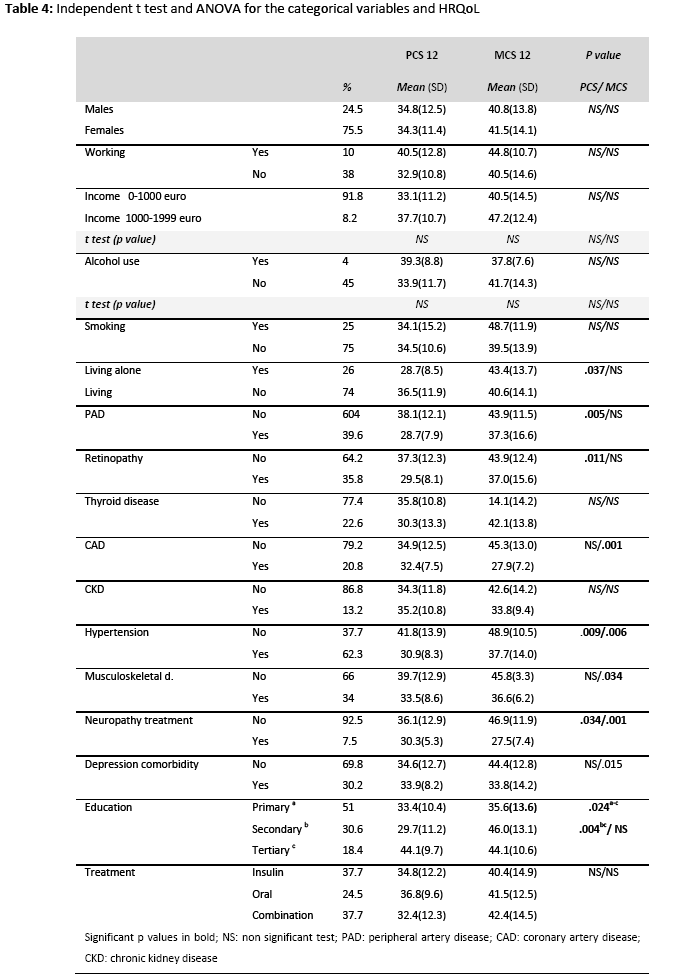
A one-way between groups analysis of variance (Table 4) was conducted to explore the impact of diabetes treatment and education in HRQOL, as measured by the PCS12 and MCS12. There was statistically significant difference at the p<0.001 level in PCS12 scores for the three groups [F4, 91= 7.338, p=0.0001]. Post-hoc comparisons using the Group comparison with Bonferroni correction (p<0.05) indicated that the mean score of PCS12 for subjects with primary education (mean=33.4, SD=10.4) was significantly different from the mean score of PCS12 for subjects with secondary education (mean=29.7, SD=11.2) (mean difference=10.75, p=0.024) and they with secondary education had a significantly lower score from the patients with tertiary education (mean=44.1, SD=9.7) (mean difference =-14.39, p=0.004). There was no significant difference between the three different treatment options (insulin, oral, combination).
Regression analysis for HRQOL model
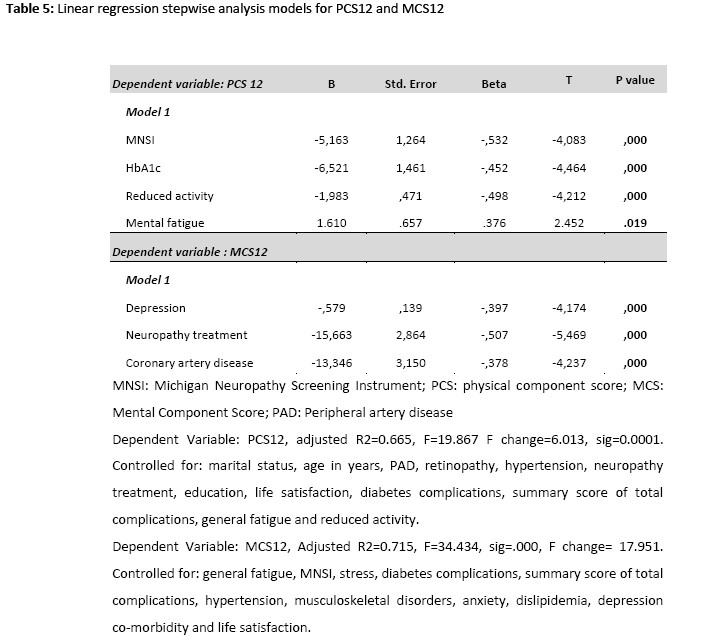
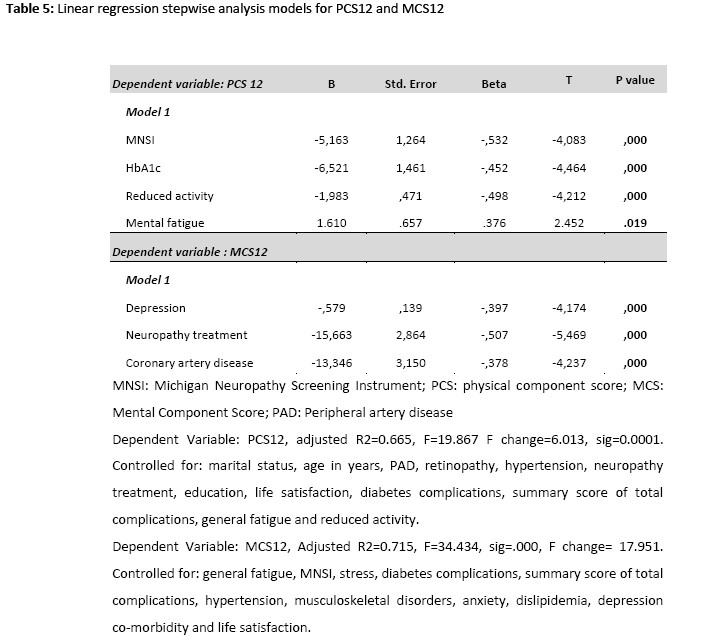
Multiple linear regression analysis was used to develop a model for predicting physical composite score (PCS12) and a model for predicting mental component score (MCS12). The results of the regression analyses with regression coefficients are presented in Tables 5. Each of the predictor variables had a significant (p < .01) zero-order correlation with PCS12 and MCS12 for each model, but only MNSI (beta=-.532, p=.001), HbA1 (beta=-.452, p=.001), reduced activity (beta=-.498, p=.001) and mental fatigue (beta=.376, p=.019) had significant (p < .05) partial effects in the full model for PCS12. As it was expected, neuropathy symptoms (MNSI), reduced activity, mental fatigue and worse glycemic control were consistently related to poorer physical functioning. Depressive symptoms (beta=-.397, p=.001), CAD (beta=-.507, p=.001), and treatment for neuropathy for the last 6 months (beta=-.378, p=.001) were predictors for MCS12. Higher depressive scores and existed complications were associated with significantly worse MCS12.
Discussion
The results demonstrated that patients with DN had significantly lower HRQoL compared to a previous research concerning the general population in Greece. [25]. Quality of life in patients with DN and T2DM could be affected by various factors. Numerous demographic and psychosocial factors such as age, marital status, education, depressive symptoms, fatigue and psychological stress have been found to influence quality of life (QoL) [26] and indeed bivariate analysis showed significant correlations with age, education and marital status, while there was no correlation in regards to income and working status maybe because the majority of subjects were elder and retired. In addition, diabetic complications which are among the most important disease-specific determinants of QoL [27], had significant correlations in bivariate analysis but only CAD managed to stay in the final regression model of MCS12.
The results also demonstrated that both subjective factors, such as depressive symptoms and domains of multidimensional fatigue, as well as objective factors related to DN, such as neuropathy symptoms, as they were measured with MNSI and HbA1c, affected HRQoL. In particular, HbA1c, an indicator of glycemic control, was associated with impaired physical condition and therefore quality of life, in contrast to previous studies in patients with DM where this parameter was not found to be correlated to impaired HRQoL [28,29]. Thus, good glycemic control itself seems to be a significant factor in patients with DN and may contribute to better QoL.
In addition, it was found that DN was clearly associated with impaired HRQoL. This association may be independent of other co-morbidities since only CAD had a significant effect in MCS12. In patients with DN, both subjective factors, such as depression and psychological stress, as well as objective factors such as glycemic control and fatigue, were related to impaired HRQoL, suggesting that there is a need for both objectively and subjectively well controlled DN in order to have a better QoL, something that is differentiated from patients with diabetes with no DN, where objectively well-controlled diabetes does not necessarily translate to a better QoL [28].
QoL is an important health outcome in its own right, representing the ultimate goal of all health interventions. It has been reported26 that duration and type of diabetes are not consistently associated with QoL. Intensive treatment does not seem to impair it, while having better glycemic control is associated with a better life quality. Complications of diabetes are the most important disease-specific determinants of QoL, as well as numerous other demographic and psychosocial factors, which should be controlled when comparing subgroups. Studies of clinical and educational interventions suggest that improving patient’s health status and perceived ability to control their disease, results in improved QoL. Methodologically, it is important to use multidimensional assessments of QoL, to include both generic and disease-specific measures, and use these measures to guide and evaluate treatment interventions [27].
Other studies [29,30,31] have found several factors independently associated with higher physical functioning like being married, having a higher formal education, fewer co-morbidities, better perceived health; being not at risk for depression, as we performed in the bivariate analysis. Others have also observed a significant effect of normal body weight, and not taking insulin, although no such correlation could be obtained from the results of the present study [26]. This could be explained by the fact that the sample of the present study had no significant differences in terms of weight, (possibly due to the fact that they were regular patients suffering from DN for many years).
Another interesting difference with existing literature, is the fact that although in T2DM patients female gender, lower education, unemployment, long duration of diabetes, and having nephropathy and lower extremity lesions were associated with higher probabilities of reporting "some or extreme problems" in most dimensions of Euroquol (EQ-5D), which is the other most used specific questionnaire measuring health related quality of life, and the same factors in addition to retinopathy were significantly associated with lower levels of HRQoL 30, whereas in the present study they didn’t. Even though in the present study such a difference between genders, was not found, associations with other complications like PAD, retinopathy, CAD, musculoskeletal problems were observed as well. The same applies to the significant correlation observed between both physical and mental functioning with the summary score of diabetic and total complications.
It is a very important issue, the fact that depressive symptoms had a strong correlation in regression analysis, indicating that mental health is affected in DN as well as in DM from the psychological state of the patient. Indeed, in other researches too, patients reported "some or extreme problems" most frequently in Pain/Discomfort and Anxiety/Depression dimensions of EQ-5D respectively [30]. In another study, self-reported depressive symptoms had a significant effect on lowering the Euro-QoL visual analogue scale (EQ-VAS) in the diabetes group, while stress level had a significant effect in lowering both the EQ-5D and the EQ-VAS. In the present study, stress had also a significant negative correlation with MCS12, but it also had a significant small positive correlation with PCS. In addition, although HbA1c, diabetes duration, and treatment modalities had no significant effect on lowering HRQoL in other studies [28], in our findings HbA1c was one of the predictors in the model of PCS12, something that was expected since poor glycemic control is one of the reasons leading to DN [31]. A correlation between CAD and MCS, was also observed in a recent study about economics in health, where it was revealed that the presence of CAD, resulted in utility decrements (P < 0.001) for all the instruments that measured HRQoL [32].
A major difference between the sample of the study and another research concerning DM patients in general was the final predictors of the two main components of the SF questionnaire. While in the present study with DN patients, MNSI, HbA1c, reduced activity, mental fatigue, depression, treatment and CAD were the most important predictors of impaired HRQoL, elsewhere female gender, diabetic complications, non-diabetic comorbidity and duration of diabetes were the significant predictors of the model with SF-36. Despite these differences which may be explained due to the fact that in that study fatigue was not included in the models and the sample were not only DN patients, both multivariate regression analyses produced models explaining significant portions of the variance in SF-36 and SF-12 subscales, especially physical functioning and also showed that diabetes-related indicators were more important disease predictors, compared to sociodemographic variables, as it had been done in the present study [14].
The present study is not without any limitations. Data were collected from two outpatient diabetic clinics. A possible selection bias could not be excluded since the more concerned diabetic patients might seek a specialized diabetes care. However, the findings could have significant implications for health promotion in medical practice in Greece. Also, we did not use a control group to our analysis because our aim was to estimate factors that are related with quality of life in a specific sub-population of diabetic patients, those with diabetic neuropathy. Adding a control group - healthy subjects or/and diabetic patients without neuropathy -would make the analysis hard to follow.
In conclusion results of the present study suggest that good quality of life is significantly related to good diabetes self-management and HbA1c control in T2DM patients with DN. Therefore, these patients should be encouraged to perform self-management for controlling their blood glucose levels and improving their QoL as it was reported in a previous research concerning T2DM patients with foot ulcers [32]. Therefore, in order to preserve a good HRQOL, it is obviously important to prevent diabetes complications and properly manage concomitant chronic diseases even when the patient has already DN.
Acknowledgements
We would like to thank Dr Georgia Kostopanagiotou, Professor of Anesthesiology, 2nd Department of Anesthesiology, School of Medicine, University of Athens, Pain Unit, “Attikon” University Hospital, Athens, Greece for her assistance with the protocol design, Dr Stavros Pappas, Director in 3rd Department of Internal Medicine and Diabetes Center, General Hospital of Nikaia, Piraeus, Greece, for giving his permission to run the present protocol, Dr Vasileios Spinaris, Director of Psychiatric Ward, General Hospital of Nikaia, Piraeus, Greece for the evaluation of depression co-morbidity, as well as Mrs. Vergidou P. (Staff Nurse at General Hospital of Nikaia) and Mrs Prassa D. (Nurse at Attikon University Hospital) for their enormous help accessing the patients files. We would also like to thank all the patients that took part in this study.
Conclusions
The present study examined the intrahospital transport procedure of non-ICU patients and found that in a very large proportion the administration of therapy was interrupted during transport. This finding is particularly important since the study found that the interruption of oxygen affects the health condition of patients, causing a decrease in SatO2 and an increase of breath frequency. Therefore, the results of this study support the international literature that intrahospital transports can put patients at risk.
The development and maintenance of a written protocol of intrahospital transport procedures in Greek hospitals and education of nurses in minimizing the risks could significantly reduce the incidence of adverse complications and ensure the quality of care provided to patients. Certainly, there is a great need for further study of the intrahospital transports in Greek hospitals, focusing on factors associated with complications and challenges, on the education of nurses and other health professionals, in order safe transports to be performed.
This study involves certain limitations that need to be addressed. Firstly, took place only in one clinic of a large hospital of Athens and patients from other clinics and other hospitals of Athens or the region were not included, which reduces the generalisability of the study results. Second, there was a limited period of data collection in the study and a small number of patients enrolled. However, this study involved non-ICU patients undergoing an intrahospital transport measuring the interruption of oxygen and intravenous therapy, which very few studies have assessed, although various guidelines have proposed the importance of the continuation of applied therapy during transport.
2928
References
- Gikas A, Sotiropoulos A, Panagiotakos D, Pastromas V, Paraskevopoulou E, Skliros E, et al. Rising prevalence of diabetes among Greek adults: findings from two consecutive surveys in the same target population. Diabetes research and clinical practice. 2008 Feb;79(2):325-9.
- Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes research and clinical practice.2011; 94(3):311-21.
- Vinik A, Ullal J, Parson HK, Casellini CM. Diabetic neuropathies: clinical manifestations and current treatment options. Nature clinical practice. Endocrinology & metabolism. 2006; 2(5):269-81.
- Treede R-D, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008; 70(18):1630-5.
- Poncelet AN. Diabetic polyneuropathy. Risk factors, patterns of presentation, diagnosis, and treatment. Geriatrics. 2003; 58(6):16-8, 24-5, 30.
- Galer BS, Gianas A, Jensen MP. Painful diabetic polyneuropathy: epidemiology, pain description, and quality of life. Diabetes research and clinical practice. 2000; 47(2):123-8.
- Young MJ, Breddy JL, Veves A, Boulton AJ. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds. A prospective study. Diabetes care. 1994; 17(6):557-60.
- Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabaei BP, et al. Valuing health-related quality of life in diabetes. Diabetes care. 2002; 25(12):2238-43.
- Smith SC, Lamping DL, Maclaine GDH. Measuring health-related quality of life in diabetic peripheral neuropathy: a systematic review. Diabetes research and clinical practice. 2012; 96(3):261-70.
- Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabetic medicine a journal of the British Diabetic Association. 2006;23(11):1165-73.
- Massi-Benedetti M. The cost of diabetes Type II in Europe: the CODE-2 Study. Diabetologia. 2002; 45(7):S1-4.
- Anderson RM, Fitzgerald JT, Wisdom K, Davis WK, Hiss RG. A comparison of global versus disease-specific quality-of-life measures in patients with NIDDM. Diabetes care. 1997; 20(3):299-305.
- Parkerson GR, Connis RT, Broadhead WE, Patrick DL, Taylor TR, Tse CK. Disease-specific versus generic measurement of health-related quality of life in insulin-dependent diabetic patients. Medical care. 1993; 31(7):629-39.
- Papadopoulos A a, Kontodimopoulos N, Frydas A, Ikonomakis E, Niakas D. Predictors of health-related quality of life in type II diabetic patients in Greece. BMC public health. 2007; 7:186.
- WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects. 2008 Oct 22; Available from: https://www.wma.net/en/30publications/10policies/b3/
- Care M, With P, Mellitus D. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2002;26Suppl 1(1):S32-S42.
- Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996; 34(3):220-33.
- Ware JE, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Medical care. 1995; 33(4 Suppl):AS264-79.
- Lunetta M, Le Moli R, Grasso G, Sangiorgio L. A simplified diagnostic test for ambulatory screening of peripheral diabetic neuropathy. Diabetes research and clinical practice. 1998; 39(3):165-72.
- Jia W, Shen Q, Bao Y, Lu J, Li M, Xiang K. [Evaluation of the four simple methods in the diagnosis of diabetic peripheral neuropathy]. Zhonghuayixuezazhi. 2006; 86(38):2707-10.
- Λυράκος Γ, Παπαζαφειροπούλου Α, Χατζηαγγελάκη Ε, Δαμίγος Δ, Μπούσμπουλας Σ, Παππάς Σ, et al. Στάθμιση της κλίμακας ελέγχου συμπτωμάτων Διαβητικής νευροπάθειας (Michigan Neuropathy screening Instrument MNSI) σε ασθενείς με σακχαρώδη διαβήτη. Ιατρικές Εξελίξεις. 2012;283(ΚΖ):12–8.
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy. 1995; 33(3):335-43.
- Lyrakos GN, Arvaniti C, Smyrnioti M, Kostopanagiotou G. P03-561 - Translation and validation study of the depression anxiety stress scale in the greek general population and in a psychiatric patient-s sample. European Psychiatry. 2011; 26(null):1731.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition - Text Revision (DSMIV-TR) . 4th editio. Amer Psychiatric Pub; 2000.
- Smets EM, Garssen B, Bonke B, De Haes JC. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. Journal of psychosomatic research. 1995; 39(3):315-25.
- Lyrakos G, Hatziagelaki E, Spinaris B, Damigos D, Spyropoulos I, Kostopanagiotou G. P-232 - The comparison of fatigue between patients with diabetes melittus, psychiatric outpatients and general population in Greece. European Psychiatry. 2012; 27(null):1.
- Kontodimopoulos N, Pappa E, Niakas D, Tountas Y. Validity of SF-12 summary scores in a Greek general population. Health and quality of life outcomes. 2007; 5:55.
- Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes/metabolism research and reviews. 2012; 15(3):205-18.
- Choi YJ, Lee MS, An SY, Kim TH, Han SJ, Kim HJ, et al. The Relationship between Diabetes Mellitus and Health-Related Quality of Life in Korean Adults: The Fourth Korea National Health and Nutrition Examination Survey (2007-2009). Diabetes & metabolism journal. 2011; 35(6):587-94.
- Ali S, Stone M, Skinner TC, Robertson N, Davies M, Khunti K. The association between depression and health-related quality of life in people with type 2 diabetes: a systematic literature review. Diabetes/metabolism research and reviews. 2010; 26(2):75-89.
- Weijman I. Diabetes at Work Fatigue in relation to job characteristics, diabetes symptoms and self-management. Universiteit Utrecht; 2005. Available from: https://igitur-archive.library.uu.nl/dissertations/2005-0311-094157/full.pdf
- Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes care. 2001; 24(6):1069-78.
- Bennett BK, Hickie IB, Vollmer-Conna US, Quigley B, Brennan CM, Wakefield D, et al. The relationship between fatigue, psychological and immunological variables in acute infectious illness. The Australian and New Zealand journal of psychiatry. 1998; 32(2):180-6.
- Krousel-Wood M, Radosevich DM, Erikson C, Blonde L, Sanderson-Austin J. Quality of care indicators, health behaviors, and physical functioning in adults with diabetes. The Ochsner journal. 2007; 7(4):158-66.
- Matziou V, Tsoumakas K, Vlahioti E, Chrysicopoulou L, Galanis P, Petsios K, et al. Factors influencing the quality of life of young patients with diabetes. Journal of diabetes. 2011; 3(1):82-90.
- Kontodimopoulos N, Pappa E, Chadjiapostolou Z, Arvanitaki E, Papadopoulos AA, Niakas D. Comparing the sensitivity of EQ-5D, SF-6D and 15D utilities to the specific effect of diabetic complications. The European journal of health economics : HEPAC : health economics in prevention and care. 2012; 13(1):111-20.
- Navicharern R. Diabetes self-management, fasting blood sugar and quality of life among type 2 diabetic patients with foot ulcers. Journal of the Medical Association of Thailand = Chotmaihetthangphaet. 2012; 95(2):156-62.