Konstantinos Giakoumidakis1*, Rokeia Eltheni2, Hero Brokalaki3, Petros Galanis4, Ioannis Nenekidis5and George Fildissis6
1RN, MSc, PhD, Cardiac-Surgery Intensive Care Unit, “Evangelismos” General Hospital of Athens, Greece
2RN, MSc candidate, Cardiac-Surgery Intensive Care Unit, “Evangelismos” General Hospital of Athens, Greece
3RN, PhD, Associate Professor, Faculty of Nursing, National & Kapodistrian University of Athens, Greece
4RN, MSc, PhD, Center for Health Services Management and Evaluation, Faculty of Nursing, National & Kapodistrian University of Athens, Greece
5MD, PhD candidate, 1st Cardiothoracic surgery department, “Evangelismos” General Hospital of Athens, Greece
6MD, PhD, Associate Professor, Faculty of Nursing, National & Kapodistrian University of Athens, Greece
- *Corresponding Author:
- Giakoumidakis Konstantinos
45-47 Ipsilantou street 10676
Athens - Greece
Tel: +306973793489
E-mail: kongiakoumidakis@gmail.com
Key words
Cardiac surgery, risk factors, ventilation
Introduction
The number of patients undergoing cardiac surgery has increased substantially the last 20 years. It has been estimated that more than 30.000 and 10.000 operations are carried out each year in the United Kingdom [1] and Greece [2] respectively. In addition, the National Center for Health Statistics estimates that in 2007, in the United States of America, a total of 514.000 open heart operations (Coronary Artery Bypass Grafting - CABG and valve surgery) were performed [3].
The duration of the mechanical ventilation of cardiac surgery patients is among factors that affect the patient outcome, in terms of morbidity and mortality, as well as the cost of the procedure and the healthcare resource utilization in general. Several investigators has correlated the delayed patient extubation with higher mortality rates [4-6], more complications [6-8], increased length of stay in the intensive care unit (ICU-LOS) or the hospital (hospital LOS) [5,6] and higher healthcare cost [9]. Nevertheless, Hawkes et al. [10] conducted a systematic review aiming to assess the effect of the early extubation on patient outcomes and concluded that there was no evidence of lower mortality and morbidity rates on the early extubated patients compared with the conventially extubated patients. However, early extubation seems to reduce the ICU and Hospital – LOS.
The aim of our study was to identify the risk preoperative and intraoperative factors for increased mechanical ventilation among cardiac surgery patients. The early identification of high risk patients could contribute to more effective allocation of the limited healthcare resources and better planning of the operative list, a fact of great importance for centers with decreased ICU beds availability. In addition, might be helpful for the development of preemptive strategies.
Methodology
Study design and setting
An observational cohort study was carried out during a three-month period (form October 2010 to December 2010) among cardiac operated patients in a general, tertiary hospital of Athens, Greece. The inclusion criteria of our study were a priori defined as below: 1. patient age ≥ 18 years old, 2. the application of a cardiopulmonary bypass (CPB) during the surgery 3. the application of the same anesthetic procedures in all patients, 4. the same postoperative management of all patients. The exclusion criteria of this study were the following: 1. emergency procedure and 2. history of stroke, neurological or psychiatric disorder.
In total 114 patients were admitted to the 8-bed cardiac surgery ICU of the hospital, 48 of whom (42.1%) met the inclusion criteria and constituted our study sample.
Data Collection
A short questionnaire on basic socio-demographic characteristics (age, gender, weight, height) and clinical patient data (history of COPD, extracardiac arteriopathy, neurological dysfunction, previous cardiac surgery, active endocarditis, unstable angina, pulmonary hypertension, preoperative serum creatinine levels, preoperative EFLV, critical preoperative state, active endocarditis, recent [≤ 90 days] myocardial infarction, type of surgery, duration of surgery, duration of CPB, ischemic time, emergency operation, number of intraoperative RBC transfusions, duration of intubation) was attended. This questionnaire was formed by the researchers of this study.
For the evaluation of EuroSCORE we used data that had been included in the questionnaire of our study. EuroSCORE is a risk stratification model for predicting perioperative risk and mortality of patients undergoing cardiac surgery. It includes three wide categories of risk factors: the patient, the cardiac and the operation associated factors. The sum of the various risk factors results to a total score which represent the predicted probability of mortality and renged between 0 and 100% (logistic EuroSCORE) [11,12]. It is the most valid and reliable tool that has been used for predicting the perioperative risk in Europe, North America and Japan [13].
One of the researchers, the same each time, obtained the data based on both medical and nursing patient records.
Anesthetic procedures
All patients were given midazolam (0.05-0.06 mg/kg) and fentanyl (5-10 μg/kg) intravenously. In addition we gave an oxygen 100% mask until the induction of anesthesia. Anesthetic induction was achieved with a combination of thiopental (5mg/kg), propofol (1.5 mg/kg), etomidate (0.1-0.2 mg/kg) and atracurium (0.15 mg/kg) intravenously. During mechanical ventilation and anesthesia maintenance all patients were given oxygen, nitrous oxide, sevoflurane and propofol (2 mg/kg/h). Nitrous oxide was stopped before heparin was administered. In addition, we administrate additional dosing of narcotics (fentanyl 50-100 μg/kg/min) and muscle relaxants (atracurium). Apart from the loading dose of muscle relaxation, frequent preserving doses of myorelaxants (1/3 of the initial dose) were administered during the operation. Additionally sevoflurane was administered by the perfusionist along the whole cardiopulmonary bypass procedure. Eventually after extracorporeal withdrawal the anesthesiologist regain the management of sevoflurane from the perfusionist and perfuse it to the lungs.
Postoperative management
After the end of the operation, all patients were transferred to the cardiac surgery ICU and placed on a volume-cycled respirator for total ventilator support, under the administration of intravenous propofol sedation (25μg/kg/min). The patients were warmed with forced air until the surface temperature reach 36 °C. The patients were weaned off the respirator using a standard protocol, based on the following criteria 14: 1. patient awake with stimulation, 2. chest tube drainage < 50ml/hour, 3. hemodynamic stability (cardiac index >2.2 L/min/m2 on minimal inotropic support, systolic blood pressure at 100-140 mmHg, no arrhythmias), 3. core temperature > 35.5°C, 4. evidence of reversal of neuromuscular blockage and 5. satisfactory oxygenation (PaO2 >75mmHg with an FiO2 ≤ 0.5) and ventilation (PaCO2 < 45mmHg). Then, patients were extubated when the following criteria met [14]: 1. patient awake without stimulation, 2. acceptable respiratory mechanics (negative inspiratory force > 25 cmH2O, tidal volume > 5 ml/kg, vital capacity > 10-15 ml/kg, spontaneous respiratory rate < 24/min) and 3. acceptable arterial blood gases on T-piece (PaO2 > 70 mmHg on FiO2 ≤ 0.5, PaCO2 < 48 mmHg and pH = 7.32 – 7.45)
Statistical Analysis
The normality assumption for continuous variables was evaluated by both using the Kolmogorov – Smirnov criterion (p>0.05 for all variables) and normal probability plots. Quantitative variables are presented as means (±standard deviations - SD) whereas categorical variables are presented as absolute and relative frequencies. Quantitative variables were followed the normal distribution. Aiming to investigate the correlation between the duration of intubation and the demographic and clinical sample characteristic we used the t-test for independent samples, the Pearson’s correlation coefficient (r) and the analysis of variance (ANOVA). Variables that were statistically different at p-value less than 0.25 (p≤0.25 was used only in that case) in bivariate analysis were entered into the backward stepwise multivariate linear regression analysis. All tests of statistical significance were two-tailed and p-values of less than 0.05 were considered as significant. Statistical analysis was performed using the Statistical Package for Social Sciences software (SPSS 16.0 for Windows, SPSS Inc., Chicago, IL, USA).
Ethical approval
Permission to conduct this study was obtained by the ethical committee of the hospital. The study has been conducted in full accordance with ethical principles, including the World Medical Association Declaration of Helsinki and the International Committee of Medical Journal Editors. The methods of the study were restricted to observing and recording patient data and no part of the standard care was omitted. The investigators assured the anonymity and confidentiality of the collected data
Results
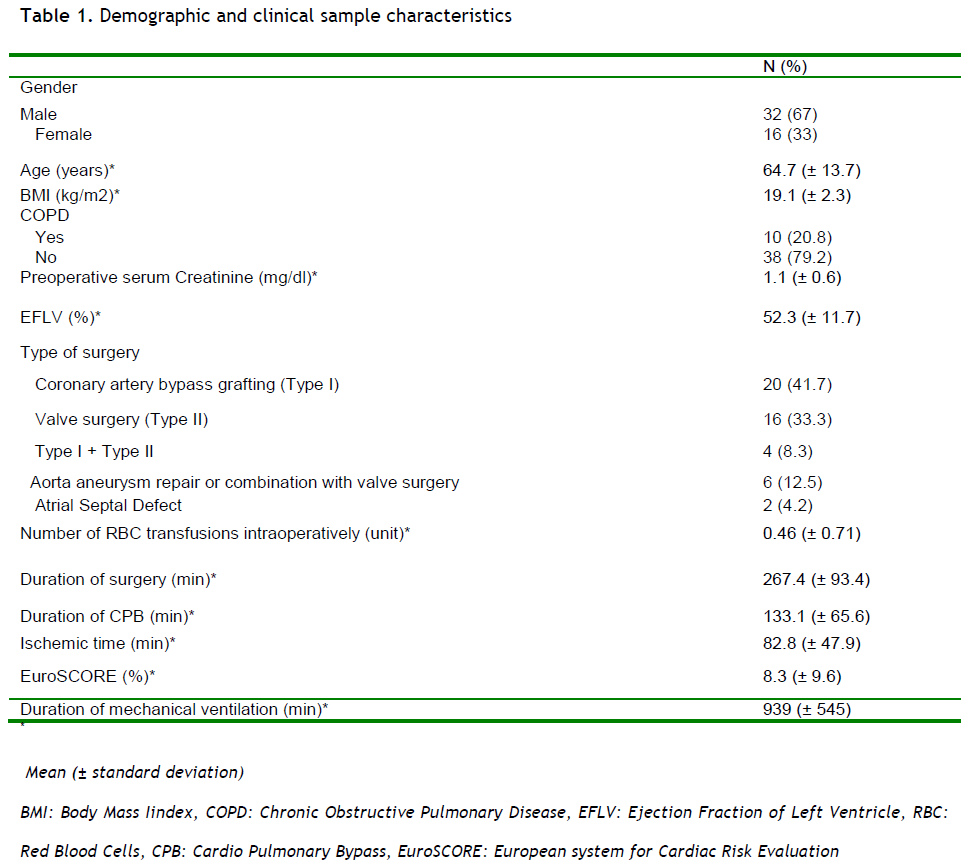
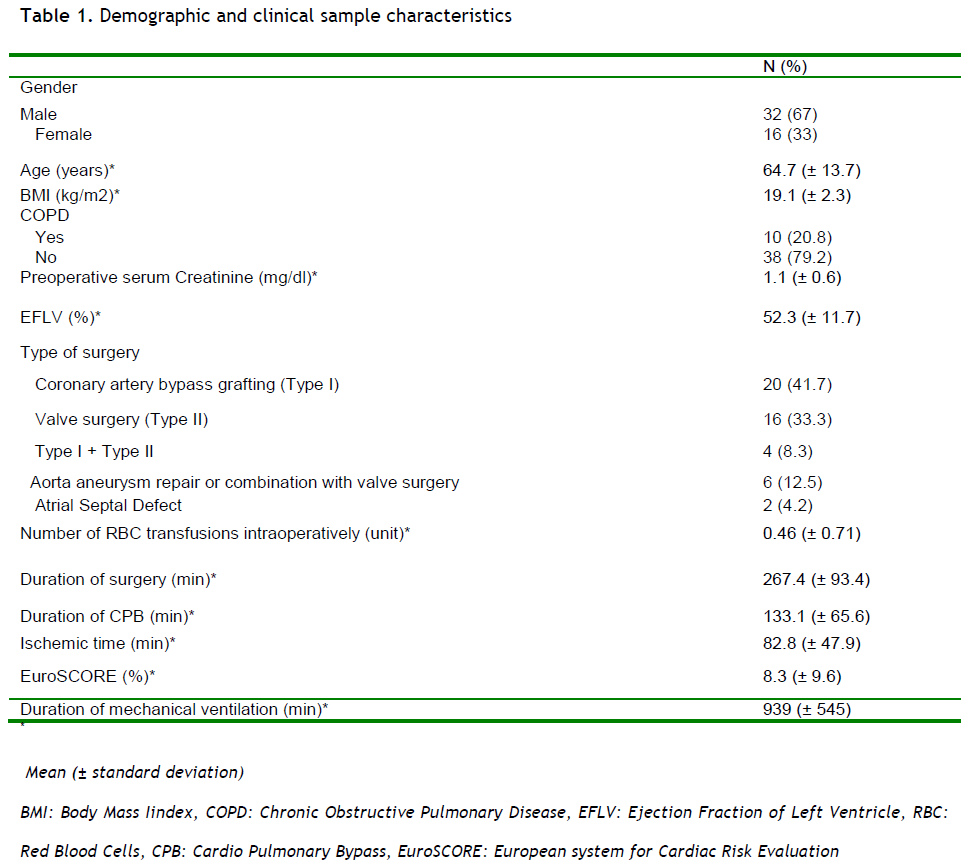
Sixty seven percent of the sample was male. The mean patient age was 64.7 (±13.7) years old, while the mean duration of intubation was 939 (±545) minutes. Most patients had either received a coronary bypass grafting (41.7%) or valve disease surgical repair (33.3%). Table 1 provides the demographic and clinical sample characteristics.
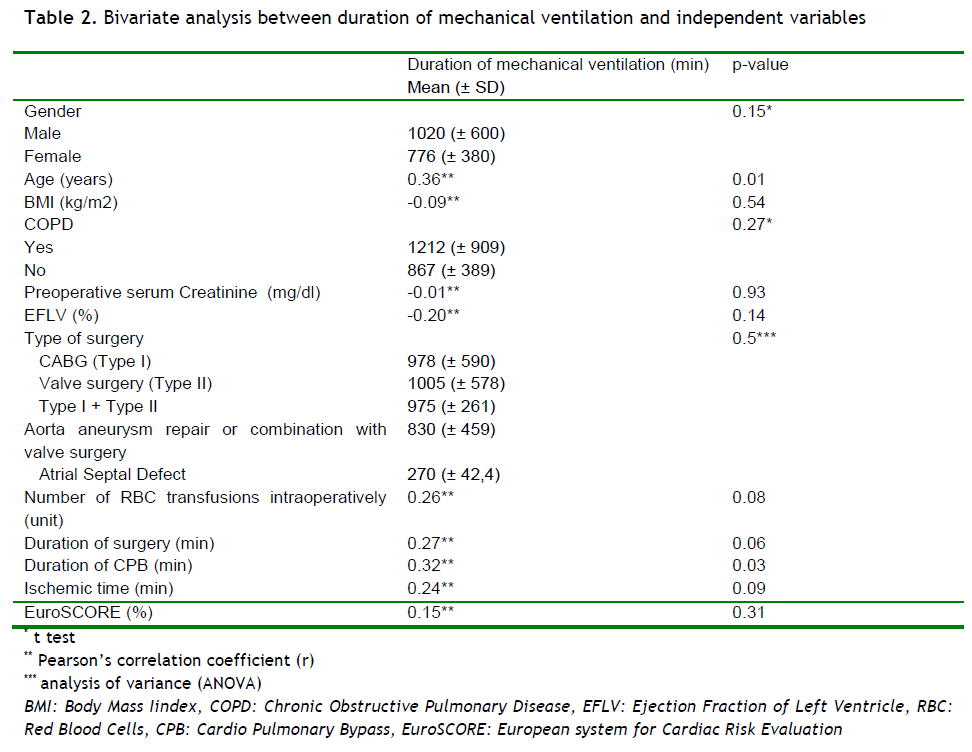
The correlation between the duration of tracheal intubation and the main risk factors, including preoperative and intraoperative variables is depicted in Table 2. Age (r=0.36, p=0.001), gender (p=0.15), EFLV (r= - 0.20, p=14), duration of surgery (r=0.27, p=0.06) and CPB (r=0.32, p=0.03), ischemic time (r=0.24, p=0.09), number of intraoperative RBC tranfussions (r=0.26, p=0.08) were associated with the duration of patient intubation at the level of 25% (a=0.25) in bivariate analysis. In particular, the older age, the male subjects, the decreased EFLV and the increased duration of surgery, CPB, ischemia and number of intraoperative transfusions with RBC units were correlated with prolonged duration of tracheal intubation among cardiac surgery patients. We did not observe any significant correlation between the duration of intubation and variables such as BMI, history of COPD, preoperative serum creatinine levels, type of surgery and EuroSCORE.
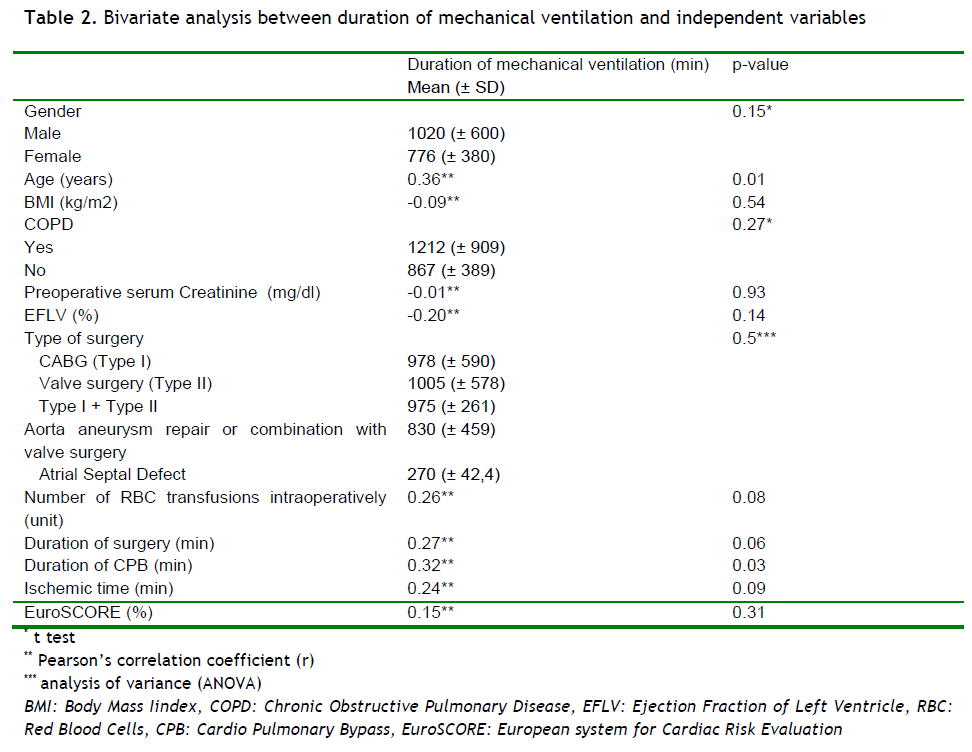
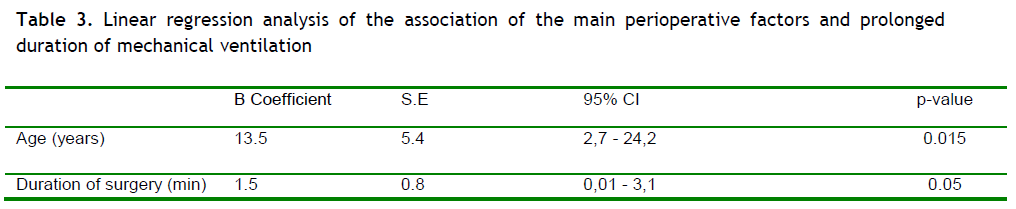
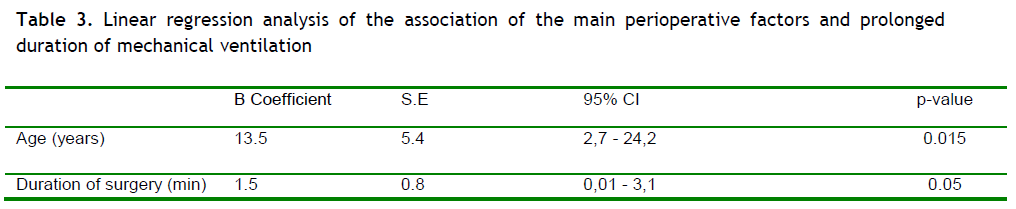
Table 3 summarizes the main findings of the multivariate analysis. We found a positive correlation between the increased age and the prolonged duration of tracheal intubation (β coefficient 13.5, 95%CI 2.7-24.2, p=0.015). In particular, the increased patient age by 1 year is correlated with increased duration of patient intubation by 1.5 minutes. In addition with the above patients with increased duration of surgery had greater probability of delayed tracheal extubation in the cardiac surgery ICU (β coefficient 1.5, 95%CI 0.01-3.1, p=0.05). In particular, the increased duration of the cardiac operation by 1 minute has as a consequence delayed patient extubation by 1.5 minutes.
Discussion
The main findings of our study were the statistically significant association of one preoperative (age) and one intraoperative (duration of the surgery) factor with the prolonged mechanical ventilation of the cardiac surgery patients. In particular the older age and the increased duration of the surgery were the independent predictors of the delayed tracheal extubation.
As aforementioned, the increased patient age was significantly correlated with prolonged intubation. In line with our results, Rajakura et al., [9] Cislaghi et al., [5] and Legare et al [15], investigating large series of cardiac surgery patients (7553, 5123 and 1829 patients respectively) concluded that the older age old is among the independent preoperative predictors of prolonged patient ventilation. In addition, Prapas et al., [16] conducted a study in a cardiac surgery center in Greece among 1359 of pump CABG patients and found that prolonged mechanical ventilation was strongly associated with advanced age. Finally, the correlation between the increased age and the delayed patient extubation was revealed by several other studies [6,17-19]. We could easily find o logical interpretation of this correlation based on the fact that elder patients are characterized as high risk surgical patients with prolong ICU and Hospital LOS [20-23] and increased mortality and morbidity rates [6,24]. Indeed the including of age as a risk factor in various risk stratification models, such as EuroSCORE and Parsonett Score, could, also, confirm our previous assertion.
At this point, we should mention that the significant correlation between older age and delayed patient extubation is a point of great interest, based on a steady increase in the age of either the cardiac surgical population over time [20,25] or of the general Greek population (23% of more than 60 years old) in conjunction with the restricted beds availability in Greece [26]. This combination reveals the necessity for rational healthcare resource allocation and utilization and also highlights the significance of the early prediction of high risk patients for prolonged mechanical ventilation, a clinical outcome which has been correlated with higher morbidity, mortality, increased length of hospital stay and therefore greater use of the restricted resources of the healthcare system.
Another important finding of this study was the association of the increased duration of surgery with the delayed patient extubation. In line with our results, Sato et al. [27] in a study of 484 CABG patients found that patients with a successful early extubation (within 6 hours of their ICU admission) had statistically significant shorter mean operation time (275±62 min) than those with delayed extubation time (325±83 min). In addition, Suemutsu et al.,[19] concluded that the increased duration of the surgery was among the predictive risk factors for delayed extubation among 167 CABG patients. The long operation time often denote technical difficulties in executing the planned operation due to unfavorable anatomy or intraoperative complications [20], a parameter which could interpret the association between the increased duration of surgery and the delayed patient extubation.
Although the duration of the operation constituted a risk factor for prolonged ventilation in our study, we did not correlate the duration of CPB with this outcome. Contrary to the findings of our study, several studies have correlated the duration of the CPB with the prolonged mechanical ventilation [4-6,28]. This result could be justified by the pulmonary complications and the increased morbidity rates that associated with the application of the extracorporeal circulation which inhibits the function of the lungs [29,30]. In addition, it is known that the use of CPB has been associated with a systematic inflammatory response that produces an increase in endothelial permeability and accumulation of extravascular lung water, decreases lung surfactant contributing to atelectasis and therefore has been incriminated as the major cause of postoperative pulmonary dysfunction [31,32].
Limitations
Our study allows us to reach significant conclusions regarding the preoperative and intraoperative factors that might affect the duration of the mechanical ventilation of cardiac surgery patients. In addition, is, among the few Greek studies, aiming to examine and indicate the risk factors for prolonged ventilation in this particular population. However, this study has some limitations. Firstly, the small sample size in conjunction with the fact that the study was conducted in one cardiac surgery ICU of one hospital limit the generalization of the findings to cardiac surgery patients treated in a wide range of ICUs and affect the external validity of our study. Secondly, our study did not identify postoperative variables that could be risk factors for prolonged patient ventilation aiming to examine only postoperative and intraoperative variables that could contribute to the prediction of high risk patients and the more effective allocation of healthcare resources. Nevertheless, the requirement for prolonged ventilation is greatly influenced by postoperative variables, such as the use of multiple blood products [19], the excessive mediastinal bleeding and the reoperation for bleeding [9,15,28]. Finally, another important limitation is the different cut off points for the definition of the prolonged mechanical ventilation, which limits the ability to compare the literature findings. Further research is needed to identify factors that might affect the duration of the mechanical ventilation among cardiac surgery patients.
Conclusions
The duration of the mechanical patient ventilation after cardiac surgery is a significant parameter, which influence the healthcare outcome, in terms of morbidity, mortality, resources’ utilization and healthcare cost. The increased age and the prolonged duration of the surgery seem to be strongly associated with delayed tracheal extubation contributing to the early prediction of high risk patients for prolonged ventilation. Early identification could encourage the relevant authorities to efficiently allocate the limited resources available and plan the operative list, a fact of great significance for centers with restricted beds capacity. Finally, it would assist clinicians in planning measures to limit the influence of parameters associated with prolonged ventilation.
3443
References
- Riley J. Nursing management of the cardiac surgical patient. In: Hatchett R, Thompson DR, editors. Cardiac Nursing: a comprehensive guide. London: Churchill Livingstone Elsevier; 2007. p. 517-50
- Giakoumidakis K, Brokalaki-Pananoudaki H. Patient education for Coronary Artery By-pass Grafting. Nosileftiki 2009; 48(2): 164-72
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart Disease and Stroke Statistics--2011 Update: A Report From the American Heart Association. Circulation 2011; 123(4): e18-e209
- Cislaghi F, Condemi AM, Corona A. Predictors of prolonged mechanical ventilation in a cohort of 3,269 CABG patients. Minerva Anestesiol 2007; 73(12): 615-21
- Cislaghi F, Condemi AM, Corona A. Predictors of prolonged mechanical ventilation in a cohort of 5123 cardiac surgical patients. Eur J Anaesthesiol 2009; 26(5): 396-403
- Lei Q, Chen L, Zhang Y, Fang N, Cheng W, Li L. Predictors of prolonged mechanical ventilation after aortic arch surgery with deep hypothermic circulatory arrest plus antegrade selective cerebral perfusion. J CardiothoracVascAnesth 2009; 23(4): 495-500
- Naughton C, Reilly N, Powroznyk A, Aps C, Hunt T, Hunter D, et al. Factors determining the duration of tracheal intubation in cardiac surgery: a single-centre sequential patient audit. Eur J Anaesthesiol 2003; 20(3): 225-33
- Akdur H, Yigit Z, Arabaci UO, Kocazeybek BS, G?rses HN. Investigation of the relationship between the duration of postoperative mechanical ventilation and complication incidence following coronary artery bypass graft. Med SciMonit 2007; 13(2): CR105-10
- Rajakaruna C, Rogers CA, Angelini GD, Ascione R. Risk factors for and economic implications of prolonged ventilation after cardiac surgery. J ThoracCardiovascSurg 2005; 130(5): 1270-7
- Hawkes CA, Dhileepan S, Foxcroft D. Early extubation for adult cardiac surgical patients. Cochrane Database Syst Rev 2003; (4): CD003587
- Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J 2003; 24(9): 881-2
- Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J CardiothoracSurg 1999; 16(1): 9-13.
- Toumpoulis IK, Anagnostopoulos CE, Swistel DG, DeRose JJ Jr. Does EuroSCORE predict length of stay and specific postoperative complications after cardiac surgery? Eur J CardiothoracSurg 2005; 27(1): 128-33.
- Bojar RM. Respiratory management. In: Bojar RM, editor. Manual of perioperative care in adult cardiac surgery. Malden, Massachusetts: Blackwell Publishing; 2005. p. 292-338
- L?gar? JF, Hirsch GM, Buth KJ, MacDougall C, Sullivan JA. Preoperative prediction of prolonged mechanical ventilation following coronary artery bypass grafting. Eur J CardiothoracSurg 2001; 20(5): 930-6
- Prapas SN, Panagiotopoulos IA, HamedAbdelsalam A, Kotsis VN, Protogeros DA, Linardakis IN, et al. Predictors of prolonged mechanical ventilation following aorta no-touch off-pump coronary artery bypass surgery. Eur J CardiothoracSurg 2007; 32(3): 488-92
- London MJ, Shroyer AL, Coll JR, MaWhinney S, Fullerton DA, Hammermeister KE, et al. Early extubation following cardiac surgery in a veterans population. Anesthesiology 1998; 88(6): 1447-58
- Rashid A, Sattar KA, Dar MI, Khan AB. Analyzing the outcome of early versus prolonged extubation following cardiac surgery. Ann ThoracCardiovascSurg 2008; 14(4): 218-23
- Suematsu Y, Sato H, Ohtsuka T, Kotsuka Y, Araki S, Takamoto S. Predictive risk factors for delayed extubation in patients undergoing coronary artery bypass grafting. Heart Vessels 2000; 15(5): 214-20
- Bucerius J, Gummert JF, Walther T, Doll N, Falk V, Schmitt DV, et al. Predictors of prolonged ICU stay after on-pump versus off-pump coronary artery bypass grafting. Intensive Care Med 2004; 30(1): 88-95
- Ghotkar SV, Grayson AD, Fabri BM, Dihmis WC, Pullan DM. Preoperative calculation of risk for prolonged intensive care unit stay following coronary artery bypass grafting. J CardiothoracSurg 2006 May; 1:14
- Abrahamyan L, Demirchyan A, Thompson ME, Hovaguimian H. Determinants of morbidity and intensive care unit stay after coronary surgery. Asian CardiovascThorac Ann 2006; 14(2): 114-8
- Ranucci M, Bellucci C, Conti D, Cazzaniga A, Maugeri B. Determinants of early discharge from the intensive care unit after cardiac operations. Ann ThoracSurg 2007; 83(3): 1089-95
- Mozes B, Olmer L, Galai N, Simchen E. A national study of postoperative mortality associated with coronary artery bypass grafting in Israel. ISCAB Consortium. Israel Coronary Artery Bypass Study. Ann ThoracSurg 1998; 66(4): 1254-62
- Fruitman DS, MacDougall CE, Ross DB. Cardiac surgery in octogenarians: can elderly patients benefit? Quality of life after cardiac surgery. Ann ThoracSurg 1999; 68(6): 2129-35
- World Health Organization. World Health Statistics 2008. [Internet]. Available from: https://www.who.int/whosis/whostat/en/index.html. Assessed January 10th, 2011
- Sato M, Suenaga E, Koga S, Matsuyama S, Kawasaki H, Maki F. Early tracheal extubation after on-pump coronary artery bypass grafting. Ann ThoracCardiovascSurg 2009; 15(4): 239-42
- Natarajan K, Patil S, Lesley N, Ninan B. Predictors of prolonged mechanical ventilation after on-pump coronary artery bypass grafting. Ann Card Anaesth 2006; 9(1): 31-6
- Puskas JD, Thourani VH, Kilgo P, Cooper W, Vassiliades T, Vega JD, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann ThoracSurg 2009; 88(4): 1142-7
- Reston JT, Tregear SJ, Turkelson CM. Meta-analysis of short-term and mid-term outcomes following off-pump coronary artery bypass grafting. Ann ThoracSurg 2003; 76(5): 1510-5
- Ng CS, Wan S, Yim AP, Arifi AA. Pulmonary dysfunction after cardiac surgery. Chest 2002; 121(4): 1269-77
- Asimakopoulos G, Smith PL, Ratnatunga CP, Taylor KM. Lung injury and acute respiratory distress syndrome after cardiopulmonary bypass. Ann ThoracSurg 1999; 68(3): 1107-15