Mohammad Alkot1, Walaa A Almaghrabi2*, Noura Al-Najdi2, Mohammad Al-Otaibi2, Mokhtar Shatla1 and Hossam Abdelbaki3
1Department of Family Medicine, Menoufia University, Menoufia, Egypt
2Umm Al-Qura University, Makkah, Kingdom of Saudi Arabia
3Department of Pediatric, Menoufia University, Menoufia, Egypt
Corresponding Author:
Dr. Walaa A. Almaghrabi
Umm Al-Qura University, Makkah, Kingdom of Saudi Arabia
Tel: +966543892243
E-mail: Walaa.mg@hotmail.com
Received: March 14, 2018; Accepted: March 27, 2018; Published: March 31, 2018
Citation: Alkot M, Almaghrabi WA, Al-Najdi N, Al-Otaibi M, Shatla M, et al. (2018) Prevalence of Complications of Sickle Cell Disease at Makkah Al-Mukaramah, Saudi Arabia, 2017. Ann Clin Lab Res Vol.6: No.1: 226. doi:10.21767/2386-5180.1000226
Background: The studies in the Middle East Arabs have found that there are specific risk factors making Sickle cell disease (SCD) more prevalent in that part of the world, which has the fast growing in the population and the increase in consanguinity marriage. Despite of that, there are no studies conducted in Makkah Al-Mukarramah or even in all Saudi Arabia (KSA) regions that, focusing on the complications of SCD and its related risk factors.
Objectives: To determine the pattern of admission and estimate the prevalence of different complications of SCD among children in Makkah Al-Mukaramah, KSA, 2017.
Patients and methods: A retrospective, analytic, noninterventional cohort study was carried out in Makkah Al- Mukaramah, KSA over a 6 months period (from first of June 2017 to end of December 2017). The study reviewed the medical files of all sickler patients who have been admitted to the pediatric departments of the involved hospitals in the given time. Records of patients having combined thalassemia disease and/or Glucose 6 Phosphate Dehydrogenase Deficiency (G6PD) were excluded from the study. The required data were collected by using hard copies of a well-designed, semi-structured, valid and reliable checklist.
Results: The study included 145 medical files of pediatric patients with SCD. Their age ranged between one day to 14 years with a Mean ± SD of 7 ± 3.6 years. Males represent 54.5% of them. Almost two-thirds of patients (67.6%) were Saudis. All cases live outside Makkah (n=5) were diagnosed as Sickle cell anemia with Vaso-occlusive crisis (VOC) whereas 47.1% of those live in Makkah were diagnosed by VOC at admission. The most frequent complication was VOC (55.9%), followed by infection (9%). Overall, 41.4% of SCA pediatric patients were admitted once whereas 25.5% were admitted more than 5 times. Acute splenic sequestration crisis was reported among 3.1% of Saudi patients compared to 12.8% of non-Saudi patients. This difference was statistically significant. Other complications were not significantly related to patients` nationality.
Conclusion: The most frequent complication of SCD was VOC. Primary prevention of the acute complications of SCD should base on health care provider with expertise in SCD, preferably hematologist. In addition to prevention of complications through the use of penicillin prophylaxis started in the newborn period, appropriate immunizations, and blood transfusions for those at risk for stroke.
Keywords
Sickle cell disease; Sickle cell anemia; Vasoocclusive crisis; Splenic sequestration crisis; Hemoglobin S
Introduction
Sickle cell disease (SCD) is an autosomal recessive disorder characterized by production of abnormal hemoglobin S and is associated with high morbidity and mortality [1,2]. Worldwide, 257,000 sicklier out of 330,000 children born with a major hemoglobinopathy, make it the commonest international hemoglobin disorder. It was first recognized by Herrick in 1910 [3], however the first case in Saudi Arabia (KSA) reported in 1963 by Lehmann was in the eastern province of the country [4].
The hemoglobin polymerization is considered as the main mechanism of the pathophysiology of SCD. An inherited genetic mutation will cause the red blood cells (RBCs) to undergo major changes. Instead of its spherical biconcave disc, it converts into characteristic sickle shape. The more sickling of the RBCs, the more hemolysis begins which ends with chronic anemia with subsequent more occurrences of the complications. Abnormal (sickled) RBCs block the blood vessels leading to Vaso-occlusive crisis which causes an episodic pain. Sickle cell disease can present by different pictures. Lately two clinical phenotypes of SCD have been reported. Hemolysis related phenotype manifested as (severe anemia, leg ulcer and pulmonary hypertension) and Vaso-occlusive-associated phenotype manifested as frequent pain attacks, acute chest syndrome, splenic infarction, transient ischemic attack (TIA) and avascular necrosis of predominant joints. Several factors can cause them, including stress, dehydration, infections, and weather changes [5-9]. As studies showed, most of these severe complications can be prevented by regular follow up and early interventions compared to those with poor follow up compliance [10].
Many studies have discussed the prevalence of SCD. The studies in the Middle East Arab Countries have found that there are specific risk factors making SCD more prevalent in this part of the world, which are the fast growing in the population and the increase in consanguinity marriage [11].
A study conducted in KSA, discovered 108 sickler out of 45,682 children and adolescents. The regional distribution of SCD varies from the highest prevalence to the lowest one as follow: eastern, southern, western, and finally central region. However in Northern region, the study did not found any cases [12].
SCD may result in different acute and chronic complications that have mostly a high fatality rate [13]. Acute complications include the vaso-occlusive crisis, splenic sequestration crisis, hemolytic crisis, and others. Most of sickle-cell crises episodes last between 5-7 days [14].
Up to our knowledge, there are no recent studies conducted in Makkah Al-Mukarramah or even other regions in KSA that, focusing on the complications of SCD and its related risk factors. Therefore, our goal is health promotion of patients with SCD and prevention of its complications, however the specific objective is to determine the pattern of admission and estimate the prevalence and risk factors of different complications of SCD among children in Makkah Al- Mukaramah, KSA, 2017.
Patients and Methods
An analytic non interventional retrospective cohort study was carried out over a 6 months period from the first of June 2017 to the end of December 2017. The study is conducted in the pediatric wards of the three major hospitals in Makkah Al- Mukaramah KSA; which are, Maternity and Children's hospital, Security Forces hospital and Hera’a General hospital. These three hospitals are the only hospitals which admit pediatric patients in Makkah Al-Mukaramah, KSA. All medical records of sickler patients who have been admitted to the involved hospitals in the given time were included in the study except those with combined thalassemia disease and/or Glucose 6 Phosphate Dehydrogenase Deficiency (G6PD). The required data were collected from the medical records by using hard copies of a well-designed, semi structured checklist included demographic data, clinical status, cause of admission, laboratory results, treatment, complications, clinical status and date of discharge as well as adherence to the follow up regimen.
Statistical Analysis
Data were entered and analyzed by using the Statistical Program for Social Sciences (SPSS) version 21. The standard methods of descriptive statistics were used to describe the data (i.e., frequencies and percentages for categorical variables and mean and standard deviation for continuous variables). Chi-square test was used for analysis of the association between categorical variables. Significance was set at p values less than 0.05.
Results
The study included 145 medical files of pediatric patients with SCD (Table 1). Their age ranged from one day to 14 years with a mean of 7 years and standard deviation of ± 3.6 years. Males represent 54.5%. Almost two-thirds of patients (67.6%) were Saudis. Majority of them (96.6%) live in Makkah and admitted through the emergency departments of involved hospitals (89%).
| Variables |
Frequency |
Percentage |
| Gender |
| Male |
79 |
54.5 |
| Female |
66 |
45.5 |
| Nationality |
| Saudi |
98 |
67.6 |
| Non-Saudi |
47 |
32.4 |
| Residence |
| Makkah |
140 |
96.6 |
| Outside Makkah |
5 |
3.4 |
| Admitted through |
| Emergency department |
129 |
89 |
| Out-patient department |
16 |
11 |
Table 1: General characteristics of pediatric patients with Sickle cell disease (n=145).
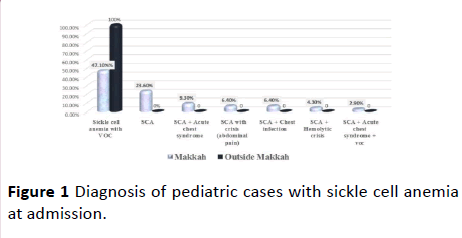
Diagnosis of cases at admission is presented in Figure 1. All cases live outside Makkah (n=5) were diagnosed by Sickle cell anemia with Vaso-occlusive crisis (VOC) whereas 47.1% of those live in Makkah were diagnosed by VOC at admission. Almost one quarter of patients live in Makkah (23.6%) were admitted with only sickle cell anemia (SCA) whereas 9.3% of them were diagnosed with SCA with acute chest syndrome at time of admission.
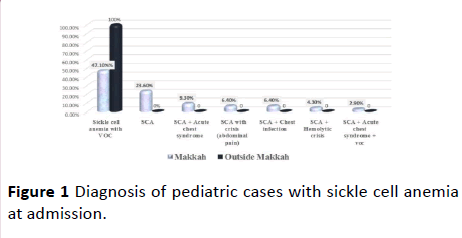
Figure 1: Diagnosis of pediatric cases with sickle cell anemia at admission.
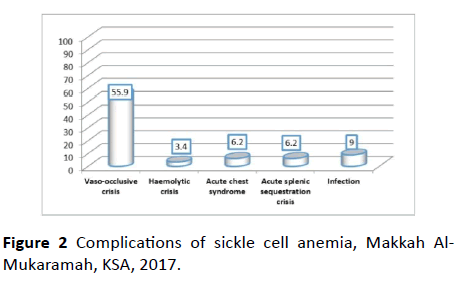
Figure 2 summarizes the complications of sickle cell anemia. The most frequent complication was VOC (55.9%), followed by infection (9%).
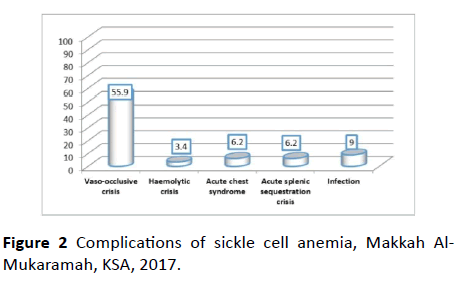
Figure 2: Complications of sickle cell anemia, Makkah Al- Mukaramah, KSA, 2017.
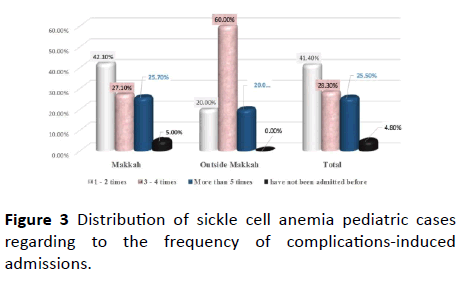
Overall, 41.4% of SCA pediatric cases were admitted once whereas 25.5% were admitted more than 5 times as illustrated in Figure 3.
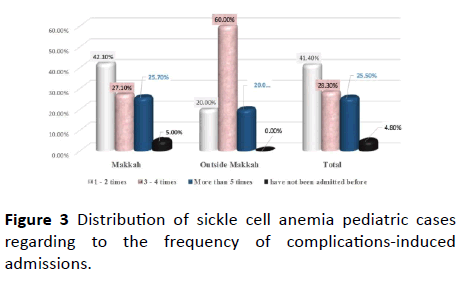
Figure 3: Distribution of sickle cell anemia pediatric cases regarding to the frequency of complications-induced admissions.
As obvious from Table 2, acute splenic sequestration crisis was reported among 3.1% of Saudi patients compared to 12.8% of non-Saudi patients. This difference was statistically significant, p=0.032. Other complications were not significantly associated with patients’ nationality.
| Variables |
Complication |
Chi square |
p-value |
| Saudi N=98 |
Non-Saudi N=47 |
Total N=145 |
| No |
% |
No |
% |
No |
% |
| Vaso-occlusive crisis |
| Yes |
58 |
59.2 |
23 |
48.9 |
81 |
55.9 |
- |
- |
| No |
40 |
40.8 |
24 |
51.1 |
64 |
44.1 |
1.353 |
0.162 |
| Hemolytic crisis |
| Yes |
5 |
5.1 |
0 |
0 |
5 |
3.4 |
2.484 |
0.136 |
| No |
93 |
94.9 |
47 |
100 |
140 |
96.6 |
- |
- |
| Acute chest syndrome |
| Yes |
6 |
6.1 |
3 |
6.4 |
9 |
6.2 |
- |
- |
| No |
92 |
93.9 |
44 |
93.6 |
136 |
93.8 |
0.004 |
0.605 |
| Acute splenic sequestration crisis |
| Yes |
- |
- |
- |
- |
- |
- |
- |
- |
| No |
3 |
3.1 |
6 |
12.8 |
9 |
6.2 |
- |
- |
| - |
95 |
96.9 |
41 |
87.2 |
136 |
93.8 |
5.139 |
0.032 |
| Infection |
| Yes |
9 |
9.2 |
4 |
8.5 |
13 |
9 |
- |
- |
| No |
89 |
90.8 |
43 |
91.5 |
132 |
91 |
0.018 |
0.582 |
| Frequency of admissions |
| 1 - 2 times |
42 |
42.9 |
18 |
38.3 |
60 |
41.4 |
- |
- |
| 3 - 4 times |
31 |
31.6 |
10 |
21.3 |
41 |
28.3 |
- |
- |
| More than 5 times |
19 |
19.4 |
18 |
38.3 |
37 |
25.5 |
- |
- |
| have not been admitted before |
6 |
6.1 |
1 |
2.1 |
7 |
4.8 |
6.866 |
0.076 |
Table 2: Comparison between Saudi and non-Saudi patients regarding sickle cell anemia complications.
Discussion
Sickle cell disease is one of the major health problems in KSA, especially in southern, western and eastern areas where the gene frequency of the disease is quite prevalent [15].
Many studies were carried out to detect and compare the prevalence of the SCD complications around the world [10,16,17]. Up to our knowledge, there is no study carried out in KSA to estimate the frequency of SCD complications. Therefore, this study investigated the frequency of SCD complication among pediatrics in Makkah hospitals and compared it with findings of other studies.
In the present study, the commonest reported complication was VOC (55.9%), followed by infection (9%), acute chest syndrome (6.2%), acute splenic sequestration crisis (6.2%) and hemolytic crisis (3.4%). In addition, VOC was the commonest reason for hospital admission because of SCA (47.1%), followed by SCA alone (23.6%), SCA with acute chest syndrome (9.3%). In a similar study carried out in Kuwait, reasons for SCD visits were VOC (63.2%), splenic sequestration (9.2%), hemolytic crises (8.8%), and acute chest syndrome (6.6%) while only one case for each of transient ischemic attacks (TIAs) and acute osteomyelitis due to salmonella had been recorded, with no deaths [10]. Previous studies also confirmed the findings that, the commonest complication of SCD and the most frequent reason for hospitalization was VOC [18-22]. The present study confirmed other findings [10,18] that although SCD is quite mild in our patients, a subset is admitted repeatedly mainly because of Vaso-occlusive crisis. As VOC is the most frequent reason for hospitalization because of SCD complications, parents of patients with SCD should be adequately educated about the triggers of the crisis, especially avoiding excessive physical exertion and extremes of weather and the need for proper hydration [23]. Health education for parents has been successive in preventing VOC at the critical periods of extreme weather in Kuwait [10].
Acute chest syndrome is not uncommon cause of hospital admission among our set of pediatric patients. It is the most common cause of morbidity and mortality in children and adult with SCD [23]. Quite often, patients required ICU care with ventilation and/or exchange blood transfusion [24]. In our patients, acute chest syndrome tends to be relatively mild; none of them required ICU care or exchange blood transfusion. Acute chest syndrome was probably triggered by chest infection, especially since many were preceded by cough and coryzal symptoms [25].
Among complications reported in the present study is the splenic sequestration crisis. However, it has been reported that pediatric SCD patients tend to retain their spleen function till adolescence and adulthood as about 80% of those aged between 6 and 16 years have viable splenic tissue [26]. The management of such patients is done through blood transfusion and for recurrent patients, splenectomy is indicated [27].
Infection was amongst complications reported among our patients. There are many factors that predispose those patients to severe bacterial infections, the most important of which is poor splenic function [28].
Some few patients in the present study were admitted with pain crisis. The use of hydroxy urea in such patients has been proved to be effective [10].
There was a limitation in the current study that it wasn’t possible to calculate the frequency of hospitalization among patient in general because our patients who have been hospitalized were generally referred to the clinic for follow up. Despite of that, the study highlights the most frequent complications of SCD in Makkah that require hospital admission.
Conclusion
The most frequent complication of SCD was VOC. Primary prevention of the acute complications of SCD should base on health care provider with expertise in SCD, preferably hematologist. In addition to prevention of complications through the use of penicillin prophylaxis started in the newborn period, appropriate immunizations, and blood transfusions for those at risk for stroke.
22278
References
- Jastaniah W (2011) Epidemiology of sickle cell disease in Saudi Arabia. Ann Saudi Med 31: 289–293.
- Creary M, Williamson D, Kulkarni R (2007) Sickle cell disease: current activities, public health implications, and future directions. J Womens Health (Larchmt) 16: 575-582.
- Strouse J (2016) Sickle cell disease. Handb Clin Neurol 138: 311-324.
- Lehmann H, Maranjia G, Mourant AE (1963) Distribution of sickle-cell hemoglobin in Saudi Arabia. Nature 198: 492-493.
- Kaul DK, Fabry ME, Nagel RL (1989) Microvascular sites and characteristics of sickle cell adhesion to vascular endothelium in shear flow conditions: pathophysiological implications. Proc Natl Acad Sci U S A 86: 3356–3360.
- Weatherall D, Clegg JB (1981) The thalassemia syndrome. (3rd edn) Oxford: Blackwell Science Ltd, UK. pp. 1-876
- Steinberg MH, Forget BG, Higgs D, Nagel (2000) Disorders of hemoglobin: Genetics, pathophysiology, clinical management. Cambridge: Cambridge University Press. pp. 1-1282.
- Caughey WS (1978) Biochemical and clinical aspects of hemoglobin abnormalities. New York: Academic Press, USA.
- Kato GJ, Gladwin MT, Steinberg MH (2007) Deconstructing sickle cell disease: reappraisal of the role of hemolysis in the development of clinical subphenotypes. Blood Rev 21: 37-47.
- Akar NA, Adekile A (2008) Ten-year review of hospital admissions among children with sickle cell disease in Kuwait. Med Princ Pract 17: 404-408.
- El-Hazmi MAF, Al-Hazmi AM, Warsy AS (2011) Sickle cell disease in Middle East Arab countries. Indian J Med Res 134: 597–610.
- Al-Qurashi MM, El-Mouzan MI, Al-Herbish AS, Al-Salloum AA, Al-Omar AA (2008) The prevalence of sickle cell disease in Saudi children and adolescents . A community-based survey. Saudi Med J 229: 1480-1483.
- Yawn BP, Buchanan GR, Afenyi-Annan AN, Ballas SK, Hassell KL, et al. (2014) Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA 312: 1033–1048.
- Alabdulaali MK (2007) Sickle cell disease patients in eastern province of Saudi Arabia suffer less severe acute chest syndrome than patients with African haplotypes. Ann Thorac Med 2: 158-162.
- Bartolucci P, Lionnet F (2014) Chronic complications of sickle cell disease. Rev Prat Oct 64: 1120-1126.
- Lionnet F, Hammoudi N, Stojanovic KS, Avellino V, Grateau G, et al. (2012) Hemoglobin sickle cell disease complications: a clinical study of 179 cases. Haematologica 97: 1136-1141.
- Pandey R, Sreekrishna Y, Zaki F, Krishnamoorthy N (2002) Sickle cell morbidity profile in Omani children. Ann Trop Paediatr 22: 45-52.
- Izuora GI, Al-Dusari SN, Fakunle YM (2003) Sickle cell anemia morbidity in northern Saudi Arabia. Saudi Med J24: 269-272.
- Coyne P, Smith VS, Mercier B (2003) Temperature changes, temperature extremes, and their relationship to emergency department visits and hospitalizations for sickle cell crisis. Pain Manag Nurs 4: 106-111.
- Lanzkron S, Carroll CP, Haywood C. The burden of emergency department use for sickle-cell disease: an analysis of the national emergency department sample database". Am J Hematol 85: 797-799.
- Yale SH, Nagib N, Guthrie T (2000) Approach to the vaso-occlusive crisis in adults with sickle cell disease. Am Fam Physician. 61: 1349-1356.
- Knight-Madden JM, Hambleton IR (2014) Inhaled bronchodilators for acute chest syndrome in people with sickle cell disease". The Cochrane Database of Systematic Reviews 11: 3733.
- Howard J, Hart N, Roberts-Harewood M, Cummins M, Moji Awogbade M, et al. (2015) Guideline on the management of acute chest syndrome in sickle cell disease. Br J Haematol. 169: 492-505.
- Adekile AD, Owunwanne A, Al-Za’abi K, Haider MZ, Tuli M, et al. (2002) Temporal sequence of splenic dysfunction in sickle cell disease. Am J Hematol 69: 23-27.
- Adekile AD, Akar N, Ayyash K, Saldanha W, Prakash B (2002) Indications for splenectomy among children with sickle cell disease in Kuwait. KMJ 34: 33-35.
- Booth C, Inusa B, Obaro SK (2010) Infection in sickle cell disease: A review. Int J Infect Dis.14: e2-e12.