Abstract
Background: Even though Ethiopia accepted the strategies to eliminate HIV/AIDS epidemic by 2030 still the burden is continued to be one of the priority agenda at national and regional level, which needs subsequent responses particularly among the hotspot areas and key priority population. The prevalence of HIV in late 2018 was about 74.9 million people of them 32 million had died due to acquired immune deficiency syndrome related illness in the world and 38 million in 2019 of them 1.7 million were newly infected the United Nation program (UNAIDS) and thousands had died of the disease. SubSaharan African (SSA) countries including Ethiopia share the highest global burden of HIV/AIDS. With the introduction of antiretroviral therapies (ARTs), HIV is increasingly becoming a chronic manageable disease. The global efforts on people living with HIV (PLHV) and receiving ART has increased by third since 2013 and reached 17 million people received ART in 2015. Timely ART start among PLHIV donated that a pivotal role to handle the epidemic and can shifts from survival to improve quality of life through adherence, retention in care and speed up of viral suppression. The UNAIDS’ made an ambitious plan that less than 200,000 HIV prevalence worldwide and to end new HIV infection by 2030.
Treatment success requires both a sustainable supply of ART to clinics and lifelong adherence to treatment by patients. In the last 30 years, there was high achievement in effective preventive methods like behavioral, PMTCT care and treatment (ART). Antiretroviral therapy (ART) has played an important role in improving prognosis and quality of life of HIV/AIDS patients, reducing rate of disease progression and death, can also reduce the risk of HIV transmission to sexual partners by 96%, adherence is also considered a major predictor of survival among PLHIV/AIDS, more than 95% adherence to ART reduce destruction of CD4 cells, increase survival, and improve quality of life. The present study aimed to estimate trends of ART utilization among HIV-infected patients in Tigray region.
Method: A quantitative study design was used to know the prevalence of HIV and trend of ART utilization among KPP. Secondary data review (Chart/document) was done for the period of 2012 to 2019. Result According to the survey report, there was inconsistent HIV positivity rate across the reference period among different population segments and the trend in HIV positivity rate has shown a marked decline from 1.92% in 2012 to 0.65% in 2019. Here there were no any indicators which indicate HIV positive clients linked to ART till 2015. However, from 2015 to 2016, almost all the HIV positive clients linked to ART. After 2016, link to enrolments of HIV positive clients to ART clinics showed that declined trend across the years till 2019 which indicates that, many HIV positive clients didn’t get ART care.
Overall, there were fall down of HIV positive patients enrolled to ART care was 85.46%, 75.74% and 69.20% in the years 2017, 2018 and 2019 respectively. However, poor ART adherence can create a dangerous public health problem and limit the effectiveness of available HIV treatments and is the most common reason for treatment failure. Poor ART adherence also leads to increased morbidity and mortality in low-and middle-income countries (LMIC) as patients still show poor ART adherence, become a major obstacle for fighting against HIV/AIDS. Factors affecting ART adherence include patient characteristics, ART regimen, clinical setting, social and environmental factors, and the relationship between patients and their health care providers. The overall HIV prevalence in Tigray was 1.2% greater than the global cut off point declared epidemic (>1%) contributes 9% of PLHIV nationally. Taking different population segments in Tigray, HIV prevalence was inconsistent. Among urban adults of Ethiopian population the HIV impact assessment in Tigray was 2.7% (95% CI: 1.3-4.0). According to survey report on HIV prevalence estimation and projection showed 1.85% in 2015 and 1.7% in 2019. The HIV positivity rate at 18 months among HIV exposed infants showed declining trend 9.2% to 2.49% indicating a promising PMTCT service. The proportion of HIV positive cases among those who tested for HIV was about 0.008% (332/38750) and about 86% (284/332) of them were under clinical care and about 90% initiated ART in 2019 in Tigray.
Conclusion: Trends Link to enrolment of HIV positive clients to ART clinics have declined across years, indicates that, many HIV positive clients didn’t get ART care. Poor ART adherence can create a dangerous public health problem and limit the effectiveness of available HIV treatments and is the most common reason for treatment failure. Fall to-adherence can lead to drug-resistant HIV caused by failure to achieve maximal viral suppression. A number of efforts should be implemented in healthcare services throughout the region to increase ART utilization by KPP patients in Tigray
Keywords
Know your HIV epidemic; Know your HIV response; KPP/MARPs; HIV synthesis; Quantitative
study; Positivity rate; Trends in HIV/AIDS; Response to HIV/AIDS; Antiretroviral treatment (ART)
Background
Acquired Immunodeficiency Syndrome (AIDS) is one of the most
serious public health and development challenges in sub-Saharan
Africa, including Ethiopia [1]. A systematic review in 2014
affirmed that in the glob around 36.7 million people living with
HIV, of which 52% from sub-Saharan Africa (SSA) [2] by the end of
2018, about 74.9 million people were infected and 32 million had
died due to acquired immune deficiency syndrome (AIDS) related
illness in the glob [3]. Other study in 2019 by the United Nation
program (UNAIDS) reported 38 million, among them 1.7 million
were newly infected and thousands had died of the disease [4].
Sub-Saharan African (SSA) countries including Ethiopia share the
highest global burden of H/IV/AIDS [4,5]. With the introduction
of antiretroviral therapies (ARTs), HIV is increasingly becoming
a chronic manageable disease [6]. The global effort on people
living with HIV (PLHV) and receiving ART has increased by third
since 2013 and in 2015 reach 17 million people received ART
globally. Timely ART start among PLHIV donate a pivotal role
to handle the epidemic and it shifts from survival to improving
quality of life through adherence, retention in care and speed
up of viral suppression [7] with the UNAIDS’ ambitious plan of
less than 200,000 HIV prevalence worldwide and to end new
HIV infection by 2030 [4,7]. Treatment success requires both
a sustainable supply of ART to clinics and lifelong adherence
to treatment by patients [2,8,9]. The launching of Millennium
Development Goals (MDG) aimed to reduce incidence of HIV/
AIDS in 2015 by 50%. However, HIV is still the major public health
problem [10] and it remained high in Ethiopia. Thus, to achieve
HIV/AIDS related Sustainable Development Goals (SDGs) in
Ethiopia; require efforts on scaling up comprehensive HIV/AIDS
interventions and robust health management information system
(HMIS) to evaluate the burden of HIV/AIDS. Since 2016 Ethiopia
has integrated the universal test and treat (UTT) strategy in its
national policy and the current ART guideline is adhered to and
implemented accordingly [11]. Its burdens of HIV exhibit varies
across geographic and population groups.[11,12] with universal
HIV test, immediate ART start, and rapid viral suppression with
full benefit of the ART will be achieved [13-15] Time from getting
tested for HIV to start of ART use in newly diagnosed HIV clients
varies from as short as one day to longer than 12 months [16].
There are some distinct transmission pockets among key and
priority populations (KP & PP). The Ethiopian demographic
and Health survey (EDHS) is one of the major sources of data
to determine the level of HIV epidemic and response both at
regional and national level used as an input to plan interventions
in control of HIV epidemics (21-23). According to the three
consecutive EDHS report, the HIV prevalence was 1.4% (2005),
1.5% (2011) and 0.9% (2016), which is higher than in Nepal, HIV
is epidemic with an overall prevalence of 0.30% in the population
aged [15] years. Of them 28.5% were women and 58% were men
of reproductive age. In contrast to this in all EDHS reports, the
HIV burden was almost double among women compared to men
due to various factors that increase vulnerability With significant
reduction of HIV magnitude both in female and male 1.2% and-
.6% respectively in 2016 EDHS report compared to 2005 and
2011 EDHS studies. The HIV prevalence has also varied with age
in both sex despite the inconsistent proportion of the magnitude
in different age groups and high among urban than rural settings
EDHS 2016. Similar report from the Ethiopian Population-based
HIV Impact Assessment (EPHIA) conducted in 2018 has shown
high (3.0%).
In the last 30 years, there was high achievement in advancement
of HIV knowledge related to routes of transmission, effective
preventive methods like behavioral and PMTCT, care and
treatment (ART), and other proven intervention strategies at the
population level (behavioral change interventions). However, the
inability to maintain and reach the population with these effective
interventions has remained a challenge to prevent and control
HIV. As a consequence, new HIV hotspot areas and vulnerable
population who are at risk of HIV infection were emerged across
the region that needs a timely response. According to challenges
in the HIV-care cascade are well documented with low HIV test
uptake as well as poor linkage to care and delay in initiating ART
amongst eligible individuals in care often cited as barriers to
achieving these benefits (Fox et al., 2014; McNairy et al). A systemic
review shows that non-adherence is the most common reason
for treatment failure, demand for second-line treatment often
associated with poorer patient health outcomes and increasing
healthcare costs. For these reasons, a thorough understanding
of determinants of adherence to ART is paramount. Studies on
ART adherence showed that predictors and risk factors differ per
region of the world, necessitating context-specific development
of non-adherence profiles. This will enable healthcare providers
to offer tailored care for patients at risk of non-adherence.
Antiretroviral therapy (ART) has played an important role in
improving prognosis and quality of life of HIV/AIDS patients,
reducing rate of disease progression and death. Increased access
to ART can also reduce the risk of HIV transmission to sexual
partners by 96%. ART adherence is also considered a major
predictor of survival among PLHIV/AIDS. More than 95% adherence
to ART reduce destruction of CD4 cells, increase survival, and
improve quality of life. However, poor ART adherence can create
a dangerous public health problem and limit the effectiveness
of available HIV treatments. Poor ART adherence also leads to
increased morbidity and mortality in low-and middle-income
countries (LMIC) As patients still show poor ART adherence,
become a major obstacle for fighting against HIV/AIDS. Factors
affecting ART adherence include patient characteristics, ART
regimen, clinical setting, social and environmental factors, and
the relationship between patients and their health care providers.
Thus, knowledge of epidemic and transmission dynamics will help
HIV/AIDS programs invest in the right interventions, that enable
targeting resources and interventions on geographic targeting
and hotspot mapping can assist in identifying both geographic
areas of elevated transmission and high-risk groups (46) In the
meantime, greater understanding of transmission dynamics
and more efficient implementation and delivery of prevention,
detection, and treatment programs can prevent a substantial
proportion of new infections.
It is highly important regional and federal government achieving
the targeted goals of 2030. Hence, mapping hotspot areas,
identifying social determinants and affected population groups,
especially in resource-limited settings, would help targeting and
prioritizing interventions. In Tigray, there is an urgent demand for
evidences about the dynamics of HIV/AIDS mainly the epidemic
status and response in hotspot areas, urban, rural and emerging
towns (infant areas) and associated factors. Thus, this study
aimed to explore the risk behavior and social determinants
of HIV infection, magnitude and response to HIV/AIDS and the
intervention of the existing strategies in hotspot areas, and
subpopulation groups which might help to effectively target
interventions in the region with limited resources.
Rationale of the study
HIV/AIDS has been one of the most killer diseases in the history
of human kind particularly in LMIC for the last three decades.
Consequently, it resulted in social, economic and political barriers
that demand the attention of global community. Fighting against
HIV/AIDS, several proven interventions have been invented such
as ART and PMTCT. Besides, intensive educational and counseling
interventions have been given with the aim of awareness creation
and behavioral change with special emphasis to high risk groups.
The interventions that have been done to reduce the burden
of HIV were successful and there was a remarkable declining of
prevalence of HIV in countries like Ethiopia. However, in recent
years survey studies and reports from different organizations
evidenced the increment of HIV prevalence among special groups
or KPPs in hotspot areas.
Despite the availability of multiple proven interventions and
government efforts to reduce the burden of HIV in the country,
HIV continued to be one of the prior agendas both at the national
and regional level. Thus, this study will investigate the hotspot
areas to determine the trend of ART utilization, among KPP in
Tigray regional state.
Significance of the study
The findings of this study helps to understand the regional and local
context for evidence-based decision in improving programs and
targeting the key and priority population groups and implement
possible interventions. And developed a policy document to use
as evidence-based decision making which will be disseminated to
policy makers and other relevant stakeholders. The findings will
also be helpful to update the current situation of the epidemic
to top, mid and low-level health managers so as to, it enables
for planning shorter and long-term solution in prevention and
control of the epidemic. So, the aim of this study was to assess
the prevalence of HIV and trends of ART utilization among Key
and priority population of Tigray regional state.
Methods
Study area and setting
The study was conducted in both Urban and Rural settings of
Tigray Region. The region has 52 administrative districts (34 Rural
and 18 Towns), 799 Kebelles (722 Rural and 77 Urban), with 2.5
annual growth rate. The estimated population of the region was
5,151,998 according to 2016 Population and Housing Census
projection with male to female ratio of 0.97 (CSA, 2016/17). The
young population (15 to 24 years old) constituted about 20% of
the total population (CSA, 2016/17).
Health facilities in the selected hotspot areas were also involved
in the study. On top of HMIS data review studies, documents
and reports were used to enrich the prevalence of HIV and ART
utilization among Key and Priority Population (KPP).
Study design and period
A quantitative study design was used to know the prevalence
of HIV and trend of ART utilization among KPP. Secondary data
review (Chart/document) was done for the period of 2012 to
2019.
Study population
The study populations were all relevant documents of HIV care
and treatment, interventions to mitigate HIV and Survey studies
related to HIV prevalence and ART utilization.
Data collection procedure
Retrospective charts/documents review of potential and
accessible KPPs in selected HIV hotspot areas in Tigray region
were extracted. The documents included in the review for HIV
prevalence were facility-based ANC surveillance, PMTCT, PICT and
HCT services. Administrative reports other relevant documents.
Tigray regional health bureau HMIS annual reports and health
facilities ART utilization was reviewed to see ART trend. Besides, a
review was done from surveys, guidelines, administrative reports
and other relevant documents.
Sample size determination
There was no hard and fast assumption applicable to determine
the sample size for the document review. Any relevant documents
such as the HMIS report from RHB and collaborating organizations,
survey reports in the region, administrative reports and working
guidelines were reviewed. To check the data consistency, the
inflated HMIS reports in the regional health bureau were cross
checked with the reports of respective health facilities within the
hotspot areas. Regarding other sources of information for HIV in
the region, both local and national studies were included.
Data collection tools
The data collection tools adopted from the previous similar
studies conducted by FHAPCO and UNAIDS. For HIV prevalence
and ART utilization, a sort of data extraction format was used to
collect relevant information. Data were reviewed from healthcare
services such as (ANC surveillance, PMTCT, PITC, HCT and other services), surveys (EDHS and other studies) and administrative
reports. Previous survey studies on HIV/AIDS conducted by
different
Organizations were also considered for review. Data were
collected by well trained and experienced health workers. The
collected data were kept confidential and used for the intended
purpose only.
Data analysis
Initially, a simple descriptive analysis was done regarding the
hotspots and KPPs and then the distribution of the HIV infection
among the KPPs in the selected hotspot areas in reference to the
data generated from the health facilities such as ANC surveillance,
PMTCT, PITC, HCT services and other relevant studies in the area
was described. For the analysis of HIV prevalence, ART utilization
and its trends over the specified time, simple proportion and
trend analysis was used. Frequency tables and figures were used
to present data.
Inclusion and exclusion criteria
Charts or documents of HIV/AIDS care and treatment with
complete records and information, all relevant studies on HIV/
AIDS in the region available during 2012 to 2019. Documents and
reports that lack completeness and inconsistency were excluded.
Result
Epidemiology of HIV/AIDS in Tigray
The second KYE/KYR HIV synthesis report was based on different
data sources including survey reports such as demographic and
health survey and relevant literatures and routine health service
reports such as HMIS data, PMTCT data, HIV counseling and
testing (HCT) and provider initiated testing and counseling (PITC).
As 2016 EDHS survey report, overall HIV prevalence in Tigray
was 1.2% greater than the global cut off point declared epidemic
(>1%) contributes 9% of PLHIV nationally.
Taking different population segments in Tigray, HIV prevalence
was inconsistent. Among urban adults of Ethiopian population
HIV impact assessment in Tigray was 2.7% (95% CI: 1.3-4.0)
Study reported by EPHI on HIV estimation and projection showed
prevalence of 1.85% in 2015 and 1.7% in 2019 Other studies
reported that HIV prevalence shows 0.3% and 2.1% among
youth and HIV exposed infants born from HIV positive mothers
respectively In Tigray, the positivity rate of HIV was higher among
children of people living with HIV/AIDS (2.7%). The HIV prevalence
in the rural parts of Ethiopia and Tigray was 0.99% and 0.7%
respectively which show relatively lower than the urban report
and highly varied across the sites, especially in urban areas.
Prevalence of HIV among the vulnerable
population
According to EDHS 2016 report, overall prevalence of HIV among
youth aged 15-24 years was 0.3%. When stratified by young
women and men aged 15-24 years, the HIV prevalence were
0.5% and less than 0.1% respectively in Tigray, refugees from
camps in Tigray 0.003%, prisoners 1.03% in 2019 among MARPs population, daily/seasonal laborers ranges 0.5% to 8.2% where as
0.82% from current quantitative study, among long truck drivers
varied from 4.5% [16] to 4.9 % with 1500 sample size; nationally
and 0.4% with only 228 drivers in Tigray. According to national HIV
prevention road map 2018-2020 reports that the HIV prevalence
among mobile and resident workers in hotspot areas 1.5% from
1,000,000 population. Since scarce information on regional level,
some pocket studies revealed that HIV prevalence among female
sex workers was ranged 11.9% to 32%.
Trends of HIV prevalence in Tigray
The overall trend the HIV positivity rate in Tigray 2012 to 2019
showed that a marked declined from 1.92% in 2012 to 0.065%
in 2019. However, some districts are still in a state of epidemic
based on the review of 2019. Accordingly Setit Humera, Semen
sub city (Meklle), Maichew and Alamata had higher HIV positivity
rate more than 1% compared to the regional positivity rate
(HMIS report). Based on EPHI report, there was an increasing
trend of HIV positive population across the years from 2015
to 2019. However, the trend in HIV prevalence in Tigray has
slightly decreased from 1.85 in 2015 to 1.7 in 2019 among adult
population. Among the HIV positive population reported, females
had a significant contribution to the positivity rate. Similarly,
new HIV infection has shown an increasing trend during the
2015 to 2016. However, it declined through 2017 to 2019. New
HIV infection was also found higher among females across the
survey years. The number of HIV cases among children 0-14 years
declining from 2015-2019, males higher in number than females.
And increasing trend, number of HIV exposed infants from 2005
to 2018 started declining from 2018 to 2019. HIV positivity rate
at 18 months among HIV exposed infants showed declining trend
from 9.2% in 2005 to 2.49% in 2019 indicating a promising PMTCT
service.
The HIV prevalence across rural sites is more homogeneous at
low levels than urban sites. Like in 2014 report, twelve rural sites
have shown 0% HIV prevalence in 2016 in Tigray, in contrast
higher HIV prevalence in Tigray in. Here, there is reduction of HIV
prevalence in several sites of rural areas in this survey compared
to 2014 surveillance report, from 6.8% in 2014 to 2.7% in 2016 in
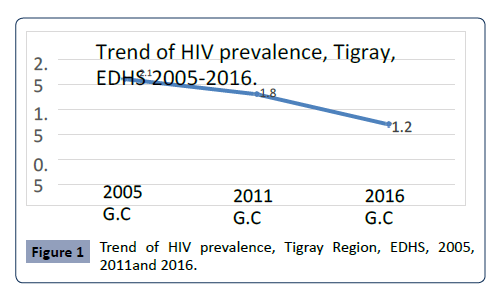
Chercher. Data from EDHS in Tigray showed that declining trend
of HIV prevalence over the past 5 years (1.8% (CI: 0.1-2.5) in
2011 VS 1.2% (CI: 0.7-1.6) in 2016). But greater than the national
average (1.5% in 2011 and 0.9% in 2016) (Figure 1).
Figure 1: Trend of HIV prevalence, Tigray Region, EDHS, 2005,
2011and 2016.
The prevalence of HIV is higher among females than males and
greater than the regional average in all the subsequent surveys.
During the subsequent surveys, the prevalence of HIV was
declining in both sexes but steady in males than females Based
on HMIS data report from 2012 to 2019 the overall trends of HIV
positivity rate significantly declined from 1.92% in 2012 to 0.65%
in 2019. However, in Mekelle and western zone remind more
than the region average. In most of zones, there was inconsistent
HIV trend over the years. Even though in Central and South East
zones have least positivity rate from 2013-2019 but the reverse
was true in most of zones from 2016 to 2017 and then started
declining in 2018.
The HIV testing was done among the key population as HIV control
and prevention responses. As shown in Table 1 below, the HIV
test campaigns did not reach majority of the target population.
Among the key population who tested for HIV, the percentage of
being tested positive were less than 0.1 in all groups.
s
| Key Population |
Target pop |
Tested |
%tested |
Tested pos |
%pos |
| FFSWs |
8,107 |
10884 |
134 |
214 |
0,019 |
| Long Distance truck drivers |
871 |
1403 |
161 |
13 |
0.009 |
| Mobile workers/Daily Laborer |
236229 |
13024 |
6 |
102 |
0.007 |
| Pregnant women |
23,480 |
30379 |
129 |
203 |
0,006 |
| Partners of pregnant women |
11,956 |
5558 |
46 |
30 |
0.005 |
| AIDS orphans |
5,146 |
2159 |
42 |
15 |
0.007 |
| Evening Class attendees |
5,436 |
1847 |
34 |
5 |
0.003 |
| Family members of ART |
21301 |
3583 |
17 |
101 |
0.03 |
| Clients |
|
|
|
|
|
| OPD clients/IPD |
46,761 |
37435 |
65 |
535 |
0,01 |
| TB/Inpatients |
|
4318 |
|
71 |
0.016 |
| Discordant couple |
|
41 |
|
3 |
0.073 |
| Prisoners |
6,003 |
4065 |
68 |
31 |
0.007 |
| HEI |
793 |
203 |
26 |
2 |
0.009 |
| Refugee |
15578 |
2941 |
19 |
15 |
0.005 |
Table1. Campaign based HIV testing among Key population June, 2017 .
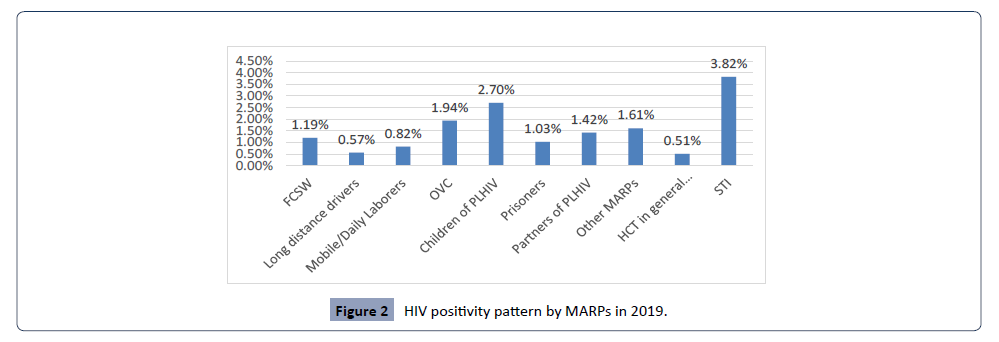
Vulnerability of population for HIV
HIV positive cases were higher among children’s of PLWHIV
and patients presented with STIs as shown in figure two below.
Besides, OVC and partners of PLHIV were also significant
contributors of HIV positivity (Figure 2).
Figure 2: HIV positivity pattern by MARPs in 2019.
Responses for vulnerable and key populations
Different interventions have been implemented to prevent and
control HIV/AIDS by the Government, NGOs or other partners.
Strengthening awareness creation on HIV transmission, peer to
peer discussion and community partnership were among the
main interventions at community level. On top of that condom
distribution and behavioral change towards condom utilization,
distributing SBCC materials, celebrating HIV/AIDS days, early
enrolled HIV positive individuals to ART, integration of HEWs with
high level health professionals, establishment of board working
on HIV follow up and monitoring, health education in hotspots
areas were key interventions implemented. In addition to these
interventions; awareness creation in tea and coffee program,
establishment of "Equb" by FSWs as a bridge or road mapping for
shifting FSWs from sex work to other non-risk work environment,
mobilization, support and care, HIV training were motivating
interventions which has been carried out by partners. To support
these interventions, the government decided all sectors to
allocate 2% of their annual budget for HIV/AIDS prevention and
control program (Table 2).
Indicators |
No HCT |
HIV Positive |
Cases enrolled |
Cases initiated ART |
Cases currently |
| |
|
cases |
In clinical care |
|
On ART |
| FSW |
1231 |
11 |
9 |
14 |
1496 |
| LTD |
208 |
1 |
1 |
1 |
0 |
| DL |
2084 |
14 |
10 |
6 |
0 |
| PW |
5939 |
32 |
27 |
19 |
0 |
| PPW |
1990 |
13 |
12 |
11 |
0 |
| AIDS orphan |
120 |
0 |
0 |
0 |
0 |
| NS. students |
35 |
0 |
0 |
0 |
0 |
| Family ART |
745 |
8 |
8 |
4 |
0 |
| OPD/IPD pts |
15229 |
132 |
115 |
59 |
6 |
| TB/STI pts |
2536 |
39 |
32 |
33 |
0 |
| D.Couple |
30 |
0 |
0 |
0 |
0 |
| Prisoner |
9 |
1 |
0 |
0 |
0 |
| HEI |
90 |
0 |
0 |
0 |
0 |
| Refugee |
1180 |
4 |
4 |
4 |
2 |
| Other |
7324 |
77 |
65 |
147 |
0 |
| Total |
38750 |
332 |
284 |
298 |
6619 |
Table2. HCT, HIV positive cases, enrolled in clinical care, initiated ART, currently on ART among different population in 2019 in Tigray Region
HIV testing and counseling, enrolled in clinical
care and currently on ART
The HIV testing and counseling (HTC) is one of the strategies to
track the HIV cases and to put them under clinical care and on
ART. As indicated in Table 2 the proportion of HIV positive cases
among those who tested for HIV was about 0.008% (332/38750).
Of the HIV positive cases, about 86% (284/332) of the cases were
under clinical care and about 90% initiated ART in 2019 in Tigray
region.
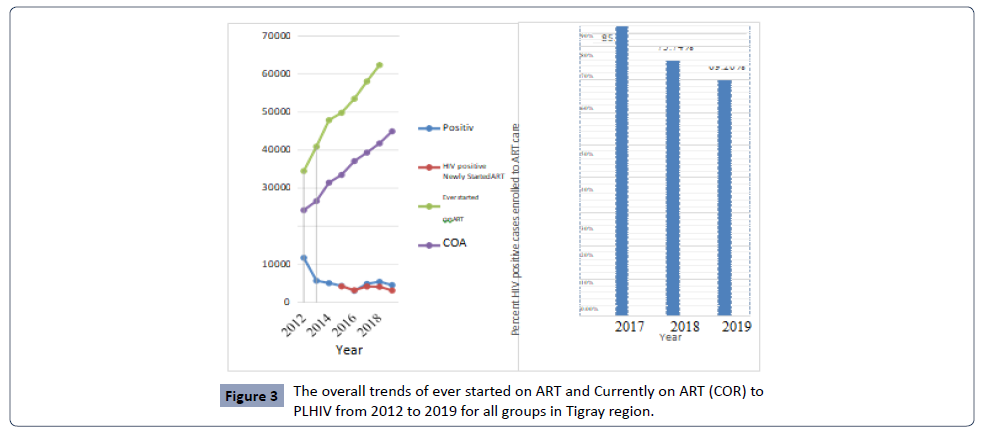
The trend for ART use among HIV positive case
As shown in Figure 3 below, there was no any indicator which
indicated HIV positive clients linked to ART till 2015.
Figure 3: The overall trends of ever started on ART and Currently on ART (COR) to
PLHIV from 2012 to 2019 for all groups in Tigray region.
Discussion
HIV infection among key populations in Tigray
Taking local epidemiology, Ethiopia has defined its key and priority
population groups. The key populations female sex workers and
prisoners and the priority populations widowed, separated or
divorced women; long truck drivers; PLHIV and their partners;
mobile and resident workers in hotspot areas with high risk of HIV
infection, limited access to services, stigma and discrimination.
Female sex workers: Even if scanty evidences in
the region
HIV prevalence among FCSWs showed that 11.9-32% Based on EDHS 2016 reported that, prevalence of HIV among the youth
[15] and College/University students of females and males was
0.5% and <0.1%respectively in Tigray, with overall 0.3% among
them According to UNHCR about 89,591 Eritrean refugees found
in four camps in January 31st 2020 have 0.46% HIV positivity rate.
Regionally, prisoners recognized as high risk groups for HIV
than the general population, exposed to stress, malnutrition,
drugs and violence become more susceptible to illness and HIV
prevalence among them is very limited nationally including
Tigray. However, campaign HIV testing showed that 7.9% national
positivity rate in 2017 and 1.03% in 2019 in Tigary among the
MARPs. Factory workers are the other vulnerable to HIV become
a global problem due to their high risk behaviors and negative
effects on production, human capital, increase AIDS dependent
orphans and child labours remain major challenge for social
security systems. According to the national HIV prevention road
map 2018-2020 report, the HIV prevalence among mobile and
resident workers in hotspot areas was 1.5% from population
of 1,000,000. Data in Tigray regional health bureau and FGD
participants reported that the known agricultural site of Tigray
attracts so many seasonal workers from all parts of Ethiopia
looking for higher wages, driving HIV epidemic with prevalence
of HIV ranges 0.5% to 8.2%. However, the current quantitative
study revealed that 0.82%, which is comparable with a study in
Metma, Ethiopia (0.5%). Furthermore HIV infection among long
truck drivers is the public health problem due to their movement
crossing Addis Ababa-Alamata-Mekelle-Adigrat-Shire-Humera
routes and Mekelle is a major destination for Tigray bound trucks
departed from Djibouti and Addis Ababa. Alamata, Makoni and
Hi-wane are known overnight truck stations. As different studies
reported that low condom utilization, making transactional sex
with CSWs have high-risk behaviors of HIV with their national HIV
prevalence ranging 4.5 to 4.9 % and 0.4% in Tigray.
Knowledge of HIV prevention methods in Tigray accounts 84.2%
in men and 66% in women compared to the national 68.6% in
men and 48.7% in women among the age group 15-49. People
who had 2+partners in the age of 25-49 years in the past 12
months found to have HIV prevalence of 0.3% in Ethiopia and
0.5% in Tigray region. Nation wise there was 57% of women and
77.1% of men have used condom compared to 75% of women
and 89.8 % of men in Tigray.
HIV/AIDS response/interventions in Tigray
Both clinical and non-clinical interventions to HIV/AIDS have been
provided regionally. At national level, the HIV AIDS policies and law
have been formulated to respond HIV/AIDS pandemic. Ethiopia
has also designed a functional strategic plan as part and package
of the HIV/AIDS response ultimately to control and prevent HIV.
All the interventions that respond to HIV/AIDS prevention and
control at regional, district and facility level are derived from
the national policy, laws and strategies. To implement these
intervention strategies, guidelines related to HIV prevention
and treatment and care have been developed. The most recent
strategic plan covers condom promotion and distribution, VCT,
PMTCT, IEC/BCC, care and support service, capacity building, HIV
mainstreaming, school-based education and Anti-HIV club.
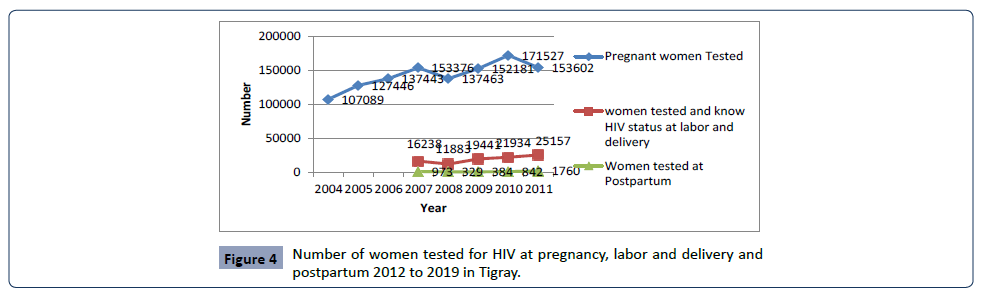
Clinical Interventions to HIV/AIDS
According to the reviewed report, the number of women tested
for HIV during pregnancy forth last 8 years steadily increased till
2018 and started declining 2018 to 2019. In contrast, number
of women tested for HIV during labor, delivery and postpartum
relatively lower compared to women tested during pregnancy
(see Figure 4 below). This disparity may indicate that mothers
who know their HIV status during pregnancy don’t repeat HIV
test during labor and post-natal.
Figure 4:Number of women tested for HIV at pregnancy, labor and delivery and
postpartum 2012 to 2019 in Tigray.
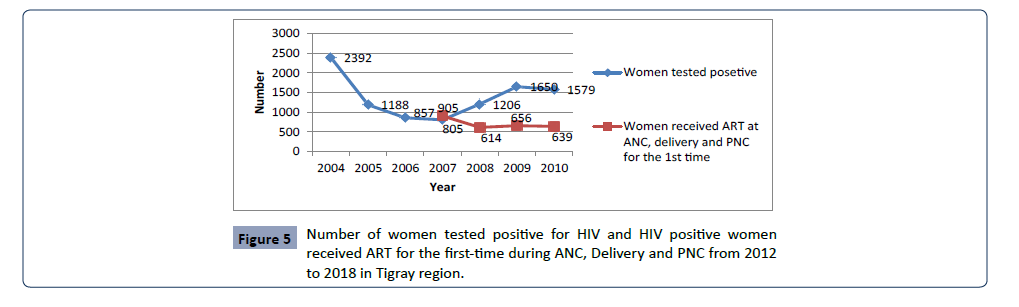
HIV positivity rate and provision of ART
HIV positivity rate among routine tested women was not
consistent. They decreased steadily from 2012 to 2015 and again
increased 2015 to 2017 and then decline slowly in 2019. With
regard to provision of ART, there was irregular trend starting
2015 to 2018. The number of women who received ART during
ANC, delivery and post-natal care were far from the women
tested positive and trend was almost constant 2016-2018 (see Figure 5 below). Other study finding showed that patients with
a history of substance use are significantly less engaged with
their health care provider, and are likely to exhibit a higher
rate of treatment refusal. A review of ART adherence, (Mills et
al) showed that reminders in the form of support from friends
and family facilitates successful ART adherence and disclosing
one’s HIV status to others had a positive influence on adherence.
However, several other studies have shown that ART adherence decreases with an increasing number of tablets and number of
daily doses. Nevertheless, various studies reported that despite
new ART regimen with fewer tablets and daily doses, adherence
remains a problem.
Figure 5: Number of women tested positive for HIV and HIV positive women
received ART for the first-time during ANC, Delivery and PNC from 2012
to 2018 in Tigray region.
HIV testing and counseling, enrolled in clinical
care and currently on ART
HIV testing and counseling (HTC) is one of the strategies to track
HIV cases and to put them under clinical care and on ART. HTC
mainly focuses on most at risk population groups such as FSWs,
long truck drivers, daily laborers and other population segment
like pregnant women, AIDS Orphan, night shift students, patients
from OPD/IPD, TB/STIs patients and prisoners. Higher number of
HCT was observed from OPD/IPD followed by pregnant women.
As indicated in Table 3 the proportion of HIV positive cases among
those who tested for HIV was about 0.008% (332/38750). About
86% (284/332) of them were under clinical care and 90% initiated
ART in 2019 in Tigray.
| Indicator |
No HCT
|
HIV Positive cases |
HIV-positive cases enrolled in clinical care |
HIV positive cases-initiated ART |
HIV positive cases currently on ART |
| Age |
<15M |
<15F |
>15M |
>15F |
<15M |
<15F |
>15M |
>15F |
<15M |
<15F |
>15M |
>15F |
<15M |
<15F |
>15M |
>15F |
<15M |
<15F |
>15M |
>15F |
| FSW |
0 |
4 |
0 |
1227 |
0 |
0 |
0 |
11 |
0 |
0 |
0 |
9 |
0 |
3 |
0 |
11 |
65 |
535 |
41 |
855 |
| LTD |
0 |
6 |
191 |
11 |
0 |
0 |
1 |
0 |
0 |
0 |
1 |
0 |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
0 |
| DL |
4 |
0 |
1430 |
650 |
0 |
0 |
11 |
3 |
0 |
0 |
8 |
2 |
0 |
0 |
4 |
2 |
0 |
0 |
0 |
0 |
| PW |
0 |
41 |
31 |
5830 |
0 |
0 |
2 |
30 |
0 |
1 |
0 |
26 |
1 |
0 |
0 |
18 |
0 |
0 |
0 |
0 |
| PPW |
0 |
7 |
1394 |
589 |
0 |
2 |
7 |
4 |
0 |
2 |
6 |
4 |
2 |
2 |
3 |
4 |
0 |
0 |
0 |
0 |
| AIDS orphan |
9 |
3 |
108 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| E. students |
0 |
0 |
16 |
19 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| Family ART |
228 |
226 |
160 |
131 |
2 |
1 |
2 |
3 |
1 |
3 |
3 |
1 |
1 |
1 |
2 |
0 |
0 |
0 |
0 |
0 |
| OPD/IPD pts |
1307 |
#### |
4594 |
8134 |
1 |
13 |
56 |
67 |
2 |
11 |
49 |
53 |
3 |
16 |
16 |
24 |
0 |
0 |
6 |
0 |
| TB/STI pts |
234 |
247 |
925 |
1130 |
3 |
3 |
16 |
17 |
2 |
15 |
2 |
13 |
2 |
15 |
2 |
14 |
0 |
0 |
0 |
0 |
| Discordant Couple |
1 |
3 |
17 |
9 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| Prisoner |
3 |
0 |
2 |
4 |
0 |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| HEI |
42 |
26 |
22 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| Refugee |
63 |
31 |
548 |
538 |
0 |
1 |
1 |
2 |
0 |
1 |
1 |
2 |
0 |
0 |
1 |
3 |
0 |
0 |
0 |
2 |
| Other |
113 |
246 |
3400 |
3565 |
1 |
5 |
28 |
44 |
1 |
4 |
24 |
36 |
5 |
11 |
98 |
33 |
0 |
0 |
0 |
0 |
| Total |
2004 |
#### |
#### |
##### |
7 |
25 |
124 |
18 |
9 |
37 |
91 |
147 |
14 |
48 |
127 |
109 |
317 |
2470 |
570 |
4460 |
Table 3. HIV testing and counseling, enrolled in clinical care and currently on ART.
Trend for ART use among HIV positive cases
As Figure 3 above showed that, there were no any indicators
which indicate HIV positive clients linked to ART till 2015.
However, from 2015 to 2016, almost all the HIV positive clients
linked to ART. After 2016, link to enrolment of HIV positive clients
to ART clinics showed that declined trend across the years till
2019 which indicate that, many HIV positive clients didn’t get
ART care. Overall there were fall down of HIV positive patients
enrolled to ART care was 85.46%, 75.74% and 69.20% in the years
2017, 2018 and 2019 respectively. A study in rural South Africa
results showed that ART uptake was high, with more than four
out of five individuals initiating ART within the first three months
of entering care, a promising observation. Furthermore, the rates
of those with CD4>350 cells/mm3 and without WHO stage 3/4 or
pregnancy who initiated ART were as high as 79.8% at month 3 and
85.3% at Month 6. Even in the context of overall high ART uptake,
only half the individuals initiated ART within one month with their
findings suggesting a more rapid initiation in sicker patients.
HIV Treatment and Care Programmers’
A meta-analysis study result; prevalence of adherence to Highly
Active Antiretroviral Therapy (HAART) among Children was 87.3%
in Tigray and the national average was 88.8%. Moreover; in Tigray
85.1% of patients who start ART were able to retain after one
year of ART initiation with different identified determinants like;
level of health facilities, gender differences and having active TB.
Another longitudinal study in Tigray, attrition was mainly due
to loss to follow-up, patients transferred-out and documented
mortality. Another studies from India and Africa showed that
traveling from distant places to ART centers was one of the
barriers to ART adherence; in contrast to this study in Nepal has
been reported that, despite the extension of ART centers into
different regions of Nepal, people living with HIV are unwilling
to seek treatment at the nearest health institution due to fear of
stigmatization in addition, one meta-analysis showed that varying
from mild to severe and from acute to chronic, adverse effects
and toxicity of the complex ART drugs was an important reason
for non-adherence; though ART program has been successful over
several critical areas, equitability issues, variability in retention of
care, and slow and low shift to second-line ART still remained to
be important challenges.
Non-clinical response/interventions to HIV/AIDS: HIV/AIDS has
been one of the top public health problems in Ethiopia and the
study area in Tigray. In response to the public health problem/
concern of HIV/AIDS, various interventions have been exercising
to avert the disease burden. The interventions that have been
implementing in response to HIV/AIDS prevention and control
strategy include: Condom promotion and distribution, expansion
of community conversation, school based HIV prevention
programmers’, life skills education, school CC programme,
training for IGA and start-up capital for sex workers and vulnerable
women, food and nutritional support for PLHIV& OVC, training
for and for OVCs, training for IGA and start-up capital for PLHIV,
educational and psychosocial support to OVC, HIV mainstreaming
in government sectors, Social mobilization and distribution of IEC/
BCC materials and partners allocated to respond HIV and AIDS.
Condom promotion and distribution
Distribution among the general population was increased
from 3,882,237 in 2016 to 4,615,935 in 2019. However, among
MARPs/KPP was declined from 7,834,076 in 2016 to 6,290,103
in 2019, furthermore the overall distribution was declined from
11,716,313 in 2016 to 10,906,028 in 2019. This might be due to
phase out of partners working on HIV/AIDS and under reporting
from different sectors or health facilities.
HIV mainstreaming: It is one of the key activities of all sectors in
the region, which is conducting in government, non-government
and private sectors to protect employees and surrounding
communities from HIV and ensure provision of treatment, care
and support for infected and affected employees and their
families. Sectors or organizations are expected to assess the
vulnerability and impact of HIV on employees, develop HIV
work place policies, prepare evidence-based plans of action,
and implement activities; allocating the necessary resources
and ownership of the HIV response. Mainstreaming was done at
different level including at regional and woreda levels. Different
sectors are implementing HIV mainstreaming at different level.
For instance, a total of 817 sectors implementing mainstreaming
activities in the region including 22, 17 and 778 in regional,
woreda and non-governmental and private sectors respectively.
These various activities were implemented to create an enabling
environment such as work place policy, establishing AIDS fund
committee and assigning focal person. Work place policy was
developed and implemented by most regional sectors and woreda
offices to guide implementation of HIV and AIDS prevention and
control [16-18]. Aids Fund Committee for HIV mainstreaming was
established at all regional sectors and woreda offices. This shows
sectors and offices are developing a sense of ownership in the
prevention and control of HIV/AIDS.
Conclusion and Recommendations
Trends Link to enrollment of HIV positive clients to ART clinics
have declined across years indicates that, many HIV positive
clients didn’t get ART care. Overall, there were fall down of HIV
positive patients enrolled to ART care was 85.46%, 75.74% and
69.20% in the years 2017, 2018 and 2019 respectively. Poor ART
adherence can create a dangerous public health problem and
limit the effectiveness of available HIV treatments and is the most
common reason for treatment failure. Fall to-adherence can lead
to drug-resistant HIV caused by failure to achieve maximal viral
suppression. A thorough understanding of factors associated
with ART (non-) adherence allows for targeted interventions. A
number of interventions should be implemented in health care
services throughout the region to increase ART utilization by KPP
patients in Tigary and disclosing one’s HIV status to others had a
positive influence on adherence.
Conflicts of Interest
The authors declare that they have no any conflicts of interest.
Authors Contributions
All the authors conceived the study idea and performed the
analysis, participated in designing data collection tools, data
management and the write-up of the manuscript. The authors
agree to be accountable for all aspects of the work related to
the integrity of any part of the work. All authors have read and
approved the manuscript.
Acknowledgments
The authors would like to acknowledge Tigray health research
institute and Tigray regional health bureau, the health facilities,
and study participants for their cooperation during the study.
Abbreviations
AIDS: Acquired Immune Deficiency Syndrome; ANC: Antenatal
Care; ART: Antiretroviral Treatment/therapy; BCC: Behavioral
Change and Communication; CDC: Center for Disease Control and
Prevention; CSA: Central Statistics Agency; DHS: Demographic
and Health Survey; EDHS: Ethiopian Population-based HIV Impact
Assessment; FCSWS: Female Commercial Sex Workers; HAART:
Highly Active Antiretroviral Treatment/Therapy; FHAPCO: Federal
HIV Prevention and Control Office; HC: Health Centers; HCPs: Health care Provider; HCT: HIV Counseling and Testing; HEI: HIV
exposed infant 6; HEW: Health extension workers; HIV: Human
Immunodeficiency; HMIS: Health Resource Information System;
KPP: Key and priority Population; KYE: Know your Epidemic; KYR:
Know your Response; MARPS : Most at Risk Populations; MDG:
Millennium Development Goals; OCV: Orphan and Vulnerable
Children; PLHIV: People living with HIV; SDG: Sustainable
Development Goal; SSA: Sub Saharan Africa; STIs: Sexually
Transmitted Infection; UNAIDS: United Nation Programme on HIV
and AIDS; UNHCR: United Nation High Commission for Refugees