Mohamed Zouari, Hamdi Louati *, Mahdi Ben Dhaou, Imen Abid and Riadh Mhiri
Department of Pediatric Surgery. Hedi Chaker Hospital. 30219 Sfax, Tunisia
*Corresponding Author:
Hamdi Louati
Department of Pediatric Surgery. Hedi
Chaker Hospital. 30219 Sfax, Tunisia.
Tel: 0021652225719
E-mail: drhamdilouati85@yahoo.com
Received date: May 17, 2018; Accepted date: May 22, 2018; Published date: May 29, 2018
Citation: Zouari M, Louati H, Dhaou MB, Abid I, Mhiri R (2018) Primary Peritonitis in Immunocompetent Children. J Univer Surg. Vol.6 No.2:14
Keywords
Primary peritonitis; Immunocompetent; Children
Dear Sir,
Primary peritonitis is defined as peritoneal infection without an evident intra peritoneal septic focus [1]. It is mainly reported in patients with nephrotic syndrome, liver cirrhosis and Immunodeficiency disorders [2]. In the absence of these conditions, primary peritonitis is exceptional, and only few cases were reported in the literature [3]. Here we report two cases of primary peritonitis in immunocompetent children.
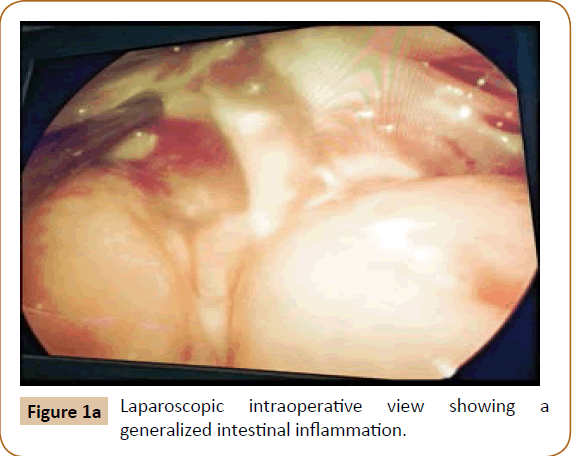
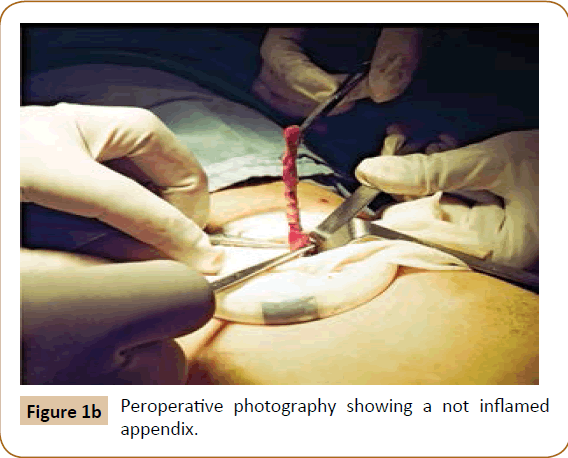
A 5 year-old girl, in prior excellent health, presented with a 4-day history of intermittent fever, abdominal pain, vomiting and diarrhea. Blood tests were performed showing elevated inflammatory markers: peripheral WBC count of 15600/mm3 with 86% neutrophils and C-reactive protein of 198 mg/L. Abdominal and pelvic ultrasound examination showed extra luminal fluid with normal appendix. Laparoscopy revealed abundant purulent fluid, with generalized intestinal inflammation (Figure 1a) but no obvious appendicitis (Figure 1b) or other intra-abdominal source. Fluid was recovered for microbiology and an appendectomy was performed and sent for histopathological examination. Culture of the peritoneal fluid was negative. The histopathological analyses of the appendix showed no inflammatory alterations. The patient was discharged home on the 7th post-operative day, and is now at 6 months of follow-up.
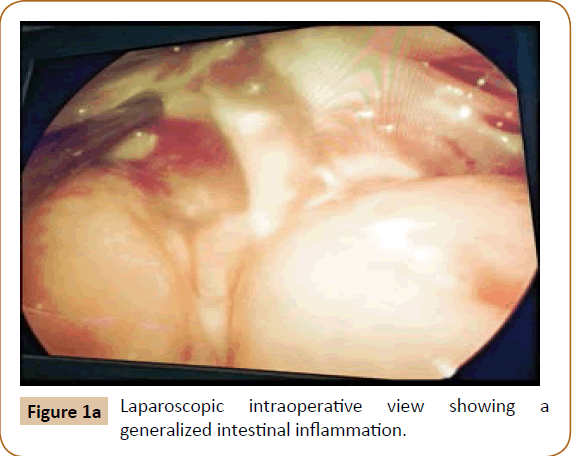
Figure 1a: Laparoscopic intraoperative view showing a generalized intestinal inflammation.
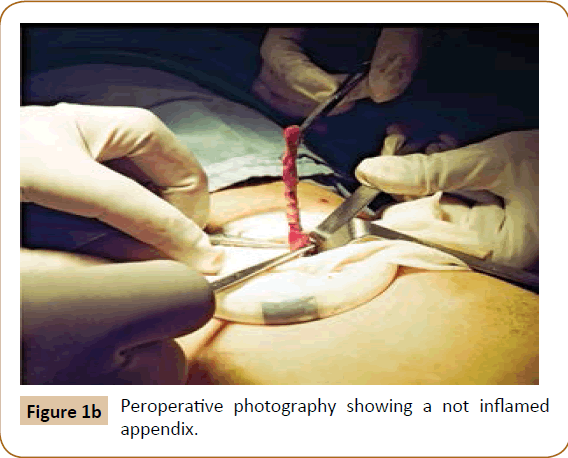
Figure 1b: Peroperative photography showing a not inflamed appendix.
A previously healthy 8-year-old girl presented with continuous abdominal pain, vomiting, diarrhea and fever up to 40°. Physical examinations revealed a positive rebound sign and diffuse tenderness. The white blood cell count was 22100/mm3, predominantly neutrophils and a C-reactive protein elevated at 230 mg/L. On laparoscopy, an odorless fibrino-purulent material was found in the abdominal cavity, covering the abdominal wall and the intra-abdominal organs. The appendix was removed and was sent for histological examination, which did not identify any kind of inflammatory process alterations. The culture from the abdominal fluid produced bacterium: Streptococcus pneumoniae sensitive to penicillin, erythromycin, cotrimoxazole, ciprofloxacine and ceftriaxone. An antimicrobial regimen (ceftriaxone) was administered for 10 days. The patient was discharged home on the 11th post-operative day, and is now at 2 years of follow-up.
Primary peritonitis is an uncommon disease accounting for 2.1% of patients presenting with an acute abdominal emergency [4]. The correct preoperative diagnosis can be made with reasonable assurity by noting several diagnostic features [2,4]. In the child who presents with abdominal findings of diffuse peritonitis occurring in less than 24 hours from the onset of symptoms without a mass or free air on abdominal roentgenograms and who gives a history of nephrosis, post necrotic cirrhosis or urinary tract infection or demonstrates bacteriuria, pyuria and a urine free of acetone should be highly suspect of primary peritonitis [4]. Temperature and white blood count, although reported to be most helpful.
The origin of the infecting organism has been a point of major controversy. Four sources are generally cited: 1) blood; 2) genital; 3) Trans-diaphragmatic lymphatics; and 4) transmural migration through the gut wall [4]. Regardless of the primary etiology of the infecting organism, it is evident that urinary pathology often precedes or accompanies primary peritonitis and that a smear of spun urine may be helpful in suggesting the correct diagnosis and proper choice of antibiotic therapy [1-4].
Although rarely encountered, primary peritonitis should be included in the differential diagnosis of acute abdominal pain in children.
Conflict of Interest
The authors declare that there is no conflict of interest.
22960
References
- Maraki S, Spathopoulou T, Ntaoukakis M, Vlachakis J (2012) Primary pneumococcal peritonitis in an immunocompetent child. Braz J Infect Dis 16: 107-108.
- Levison ME, Bush LM (2014) Peritonitis and intraperitoneal abscesses. In: Mandell BL, Bennett JE, Mandell DR, Douglas & Bennett’s Principles and Practice of Infectious Diseases (7th edn). Churchill Livingstone: 1011-1032.
- Brändle G, L'Huillier AG, Wagner N, Gervaix A, Wildhaber BE, et al. (2014) First report of Kocuria marina spontaneous peritonitis in a child. BMC Infect Dis 14: 719.
- McDougal WS, Izant RJ, Zollinger RM (1975) Primary peritonitis in infancy and childhood. Annals of surgery 181: 310-313.