Keywords
Antenatal care; Quality of health care; Public health centers; Demba gofa woreda
Introduction
Globally, 287‚000 woman dies every year from complications related to childbirth [1]. Over 300,000 maternal deaths occurred worldwide and almost all of these in low- and middle-income countries [2,3].
It is also estimated that every year 3 million newborn babies die within the first month of life [4] and between 2.1 to 3.8 million babies are stillborn [3,4]. Focused antenatal care (FANC) is one of the recommended interventions to help reduce these alarming maternal and newborn mortalities [5,6]. Most low-income countries have adopted a focused ANC strategy promoted by WHO which includes four visits and structured elements within this [5].
Although the percentage of women attending ANC (for at least one visit) generally tends to be satisfactory even in lowincome countries, maternal and neonatal mortality remain high [4]. In Ethiopia and SNNPR, for example, 82.2% and 84.7% of women attend ANC at least once respectively [7]. While maternal mortality is estimated at 673 maternal deaths per 100,000 live births, and neonatal mortality at 39 neonatal deaths per 1,000 live births [8].
According to 2011 Ethiopian demographic health survey indicated the national antenatal coverage is 34% of mothers received antenatal care from health professionals (Doctors‚ nurse and midwifes) for their most recent births. However, the coverage in Southern nation nationalities by skilled attendant is 27.6% which is when seen from the perspective of profession by Doctor 2.1%, Nurse/midwife 25.3% [8].
Thirty-four percent of women who gave birth in the five years preceding the survey [8] received antenatal care from a skilled provider that is a marked improvement from 28 percent in 2005.
According to Demba Gofa woreda Health office report of 2013/2014, those women who attended ANC with a skilled provider at least once is 70% [9]. This weak relationship between ANC use and maternal and newborn survival has motivated a recent call to focus on content and quality of care provided rather than mere ANC attendance as we aim at achieving MDG 4 and MDG 5 [2].
Although researchers frequently highlight the importance of quality of maternal care in improving maternal and newborn health [10,11], the quality of ANC remains insufficiently studied.
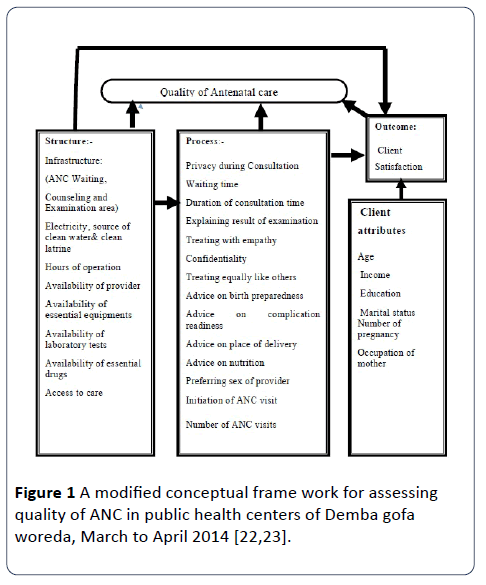
Donabedian proposed a framework for assessing quality of care which distinguishes between the attributes of the health care setting (structure), the actual care delivered (process) and the end result of the interaction between an individual and the health care system (outcome) [12,13].
Maxwell added to this initial concept by arguing that quality of care cannot be measured in a single dimension and suggested six dimensions (access‚ equity‚ appropriate‚ relevant to end‚ acceptability‚ efficient and effectiveness) of quality [14].
These qualities of care dimension have been adopted by various organizations [15,16]. Tools to capture several dimensions of quality of ANC received by mothers have been developed for high-income settings [17,18] but are not easily transferable to low-income settings. Studies in low-income countries usually rely on population-based surveys such as the Demographic and Health Survey [19] which provide some information on quality of ANC received by mothers, or on community surveys in areas with interventions aiming to improve the quality of maternal health care [20,21] where the quality of care is not necessarily representative for the country or region as whole.
In particular, it is necessary that drugs and equipment are available at the facility, that health worker are present and have the necessary knowledge and skills, and that they actually provide the recommended interventions. In settings where health facilities often lack drugs or skilled personnel, evaluating level of service provision may be more diagnostic in terms of identifying where the problem lies, than collecting information from the population on the care received. So far, hardly any published studies have assessed quality of ANC provided at health facilities in SNNPR at large and the study area in particular.
Thus this study addressed quality of antenatal care services from structural, process and outcome aspect of health facilities by focusing on availability of resources ‚ provider client interaction and satisfaction with the service provided using an adapted Donabedian health care quality model (Figure 1).
Figure 1: A modified conceptual frame work for assessing quality of ANC in public health centers of Demba gofa woreda‚ March to April 2014 [22‚23].
Materials and Methods
Study area and period
A facility based cross sectional study was conducted in Demba Gofa woreda from March 25 to April 16‚ 2014. The woreda is one of the 15 woredas of Gammo Gofa Zone in South Nation Nationalities Peoples Regional State. The administrative center, Sawla town, is located at a distance of 525 km from Addis Ababa‚ capital of Ethiopia in the Southwest direction. The Woreda is divided into 38 rural Kebeles [9]. The 2013/2014 population projected for the woreda was 98761 (male: 48393 (49%) and female: 50368) [22-24].
With regard to the health service facilities, there are four governmental health centers and 38 health posts. There are also six private health clinics namely Amanuale clinic and Hanan clinic at Boreda kebele‚ Zulo kalacha clinic‚Worikie wayesara clinic‚Lote clinic and Moja clnic in the woreda but do not undergo ANC services. The 2013/2014 estimated pregnant women of the woreda was 3546 and its ANC first coverage was 70% [9].
Study design
Facility based cross-sectional study design was employed using both quantitative and qualitative approach.
Population
Source population
All pregnant women who attend the service during data collection period and ANC service providers in four public health centers of the study area as well as other health professionals such as laboratory technologist/ technician‚ pharmacy technician/ pharmacist‚ Woreda health office curative and rehabilitation coordinator and head of health center.
Study subjects
Sampled antenatal care service users at public health centers during the study period and four selected antenatal care providers‚ four laboratory technologist /technician and four pharmacy technician/pharmacist of the health centers‚ Woreda health office curative and rehabilitation coordinator and four head of health centers. As well as twelve pregnant women.
Inclusion and exclusion criteria
Inclusion criteria: All pregnant women who reside in the study area and attend antenatal care with in data collection period and pregnant women of other facilities but attend during data collection were also included.
Key informants: ANC service providers who have experience of providing ANC service and directly involved in ANC services currently in order to provide information in amou nt‚ type and quality‚ pregnant women who have at least one ANC visit and not included in quantitative sample and had visited during data collection were included. Other health professionals such as‚ laboratory technologist /technician and pharmacy technician/pharmacist‚ Woreda health office curative and rehabilitation coordinator and head of health center.
Exclusion criteria: Pregnant women who were seriously ill and unable to respond to the questions.
Sampling
Sample size determination
The sample size was calculated using a single population proportion formula by assuming 50% of mothers were satisfied with the service they received because of absence of study in rural Ethiopia for ANC satisfaction level of mothers and it gives maximum sample size. Considering 5% margin of error (d) and confidence level of 95% (zα/2=1.96). By adding 10% non- response rates on each sample. Based on the above information a sample size of 423 was calculated. The following formula for single population proportion was used:

Where n = Sample size
Zα/2 = Confidence level at 95% = 1.96
P = 50% = 0.5
d = margin of error of 5% = 0.05
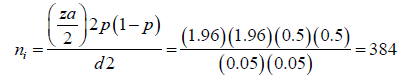
Non response rate = 10%
Nf (final sample size) = 422.4423
Sampling technique
Based on the information obtained from the study area health centers in average 12‚ 16‚ 14 and 18 daily visits which became 252‚ 336‚ 294 and 378 women were attending ANC at Dombe ‘Uba Baerea‚ Lymatsala Tasla and Lote public health centers every day respectively. The interval between selected elements from the list was calculated by dividing ANC attendees to the total sample size that was 1260/423 or 3 and this interval was used in all health centers to select study subjects by systematic random sampling until the required sample size at each health centers was obtained. This interval was obtained from the list registered to be seen by the care providers in the day of the survey. The starting point was a number between 1 and 3 that was selected randomly, which was 2, and then sample included the 2nd, 5th and 8th till satisfying the sample size calculated.
Data collection instrument and techniques
Data collection instrument: Data collection tool for structural‚ observation of service provision and some of process part was adapted from DHS service provision assessment tool [25]. Some process part and outcome category of the questionnaires were adapted from DHS and Ejigu et al. study on quality of ANC [25,26] and the outcome category had internal consistency of 0.84 at Cronbach’s alpha for study done by Ejigu et al. at Northern Ethiopia. The Cronbach’s alpha for this study became 0.894.
The tool was modified according to objectives of this study by the principal investigator. Initially the questionnaire was prepared in English then translated to local language Gofatho and Amharic and back to English by two persons who have the ability of three languages so as to keep its consistency.
Quantitative data collection tools
Structured questionnaire: Comprises socio demographic and economic factors‚ information about visit of antenatal care‚ client Satisfaction.
Qualitative data collection tools
In-depth interview guide for pregnant women comprises demographic data‚ ANC utilization and perception of pregnant women’s towards the services. The guide for providers comprises demographic data ‘quality of ANC and its determinants‚ Problems encountered when providing ANC and comments on quality of ANC.
Inventory check lists that comprise infrastructure‚ laboratory tests‚ essential ANC equipments‚ essential drugs‚ and direct observation checklists which (includes provider information‚ ANC consultation‚ client history‚ danger sign of current pregnancy‚ physical examination‚ routine tests‚ HIV counseling and testing‚ ‘maintaining a healthy pregnancy‚ iron prophylaxis‚ tetanus toxoid injection‚ deworming‚ malaria‚ preparation for delivery‚ new born‚ and post-partum recommendation).
Data Collection Procedure
Quantitative approach
Eight female nurses, who have had in service training on ANC and have experience on data collection selected for data collection and two B.Sc. midwives supervisors from other health institutions, were oriented for one day on data collection process. At the time of the actual data collection, the data collectors arrived early in the morning and give clients’ small card with recorded time of arrival.
Data on the types of services ANC attendees received were collected through interviews and observation. Pregnant women were interviewed on their exit from ANC clinics.
Qualitative approach
Four midwives from other health institution observed the way of history taking, physical examination‚ diagnosis approach and its management to one in every six of the study subjects or 70 study subjects before the exit interview and after oral consent was obtained from both the provider and the client in order to have information on services received by clients and client provider interaction.
In-depth interview with one antenatal care provider‚ head of health center from each health centers and woreda curative and rehabilitation officers was interviewed about the availability and adequacy of resources for antenatal care service provision and ANC quality issues in each health center by the principal investigator. And interview of three pregnant women at four health center catchment area was carried out. Data on structural attributes was collected by conducting resource inventory in each of the study health centers. An inventory checklist was used to see if there was uninterrupted supply of required resources for the provision of comprehensive ANC services.
Data collecting personal
Quantitative data was collected by eight in service trained female nurses whereas qualitative data was collected by principal investigators and supervisors. The supervision was done by two B.Sc. midwives and the principal investigators.
Study variables
Dependant variables: Client satisfaction.
Independent variables: Socio-demographic variables of the client (age, educational status, religion, marital status, occupation, monthly income), preferring sex of provider, frequency of ANC visits, Privacy during consultation, time of initiation of ANC, accessibility, waiting time, duration of consultation time and availability of resources, client-provider interaction‚ explains procedures‚ advice on birth preparedness and nutrition‚ advice on birth complication.
Operational and definition of terms
Health care quality is the ultimate validation of achieving and producing health and satisfaction [13].
Health care quality: The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge as well as clients’ expectations [16].
Client satisfaction: Satisfaction can be defined as the extent of an individual's experience compared with his or her expectations [25-27]. It is measured in this study using twelve indicator items of questions related to satisfaction during examination, respectfulness, time concern, advice and information provided.
Satisfaction: It was measured based on five Likert scale which are named strongly disagree‚ disagree‚ neutral‚ agree and strongly agree “the responses strongly agree and agree are classified as satisfied and responses strongly disagree‚ disagree and neutral as not satisfied. Neutral responses were classified as not satisfied considering that they might represent a fearful way of expressing dissatisfaction. This is likely because the interview is undertaken within the health facilities and mothers might be in fear to express their dissatisfaction feeling of the services they receive. This measures each respondent’s satisfaction level [28].
Overall satisfaction level: 75% response of the twelve satisfaction indicator items were categorized under “satisfied” and those who were satisfied in less than 75% of the items were categorized as “not satisfied” [28].
Quality antenatal care: It was measured in terms of client satisfaction and availability of laboratory tests, drugs‚ supplies‚ infrastructures‚ skilled health personal and equipments for ANC service provision for this study.
Respecting client: Greeted and called by name in the beginning and appointment given at the end.
Waiting time: It is the time starts from the arrival of the client to the health center till the reception of the service. It is measured in this study based on the opinion of the clients.
Privacy: The state of freedom from interference or public attention while antenatal care is provided which is measured in view of the clients.
Consultation time: The time from the start of the consultation to its end. It was measured based on the perception of the clients.
Availability of infrastructure: It is said to be available when it is in line with national standard [29].
Availability of essential drugs: Tetanus vaccine‚ iron folic and ferrous sulphate should not be absent for a day and has to have a minimum stock for at least two month [9]. At least one broad-spectrum antibiotic (amoxicillin or Augment in or Cotrimoxazole); either Albendazole or mebendazole; methyldopa (Aldomet); the first -line antimalarials; and at least one medicine for treating each of the following reproductive tract infections: Trichomanesis, gonorrhea, Chlamydia, syphilis, candidacies‚ and helimenthesiasis in place during data collection period [26].
Training here refers to structured pre-or in-service sessions any time during the 12 months preceding the survey; it does not include instructions that they may have received during supervision.
Availability of laboratory tests: Said to be available when at least the recommended tests such as urine test for infection and protein tests‚ rapid syphilis test‚ hemoglobin‚ blood group and Rh) are observed during data collection period.
Availability of basic equipments: It is said to be available when it is in line with national standard and observed during data collection period in service delivery area (sphygmometer‚ fetoscope‚ thermometer‚ speculum‚ measurin gtape‚ examination coach‚ stethoscope‚ blood pressure apparatus and adult weighing scale [29].
Availability of skilled personal: In maternal and child health case team if three midwifery specifically‚ two health officer‚ two laboratory technicians‚ three pharmacy technician‚ five nurse‚ one sanitarian in the health center in general is said to be available (meets minimum number requirement [29].
Accessibility: The potential ability of women to enter antenatal care services and maintain care for herself and fetus during antenatal care period. According to study participants it includes being able to begin antenatal care as early as possible with health care provider of the women’s choice. It also encompasses having care available in location that are convenient to women’s home or place of work close to bus routes and with adequate free or inexpensive charges. It was measured in this study in terms of physical access‚ financial access and availability of services in the view of ANC clients.
Users’ fee or charges for ANC service: User fees are charges levied at the point of use for any aspect of health services, and may include: registration fees, consultation fees, fees for drugs and medical supplies or charges for any health service rendered. Fees can be paid for each visit can encompass a whole episode of illness in this study‚ it is measured in the view of clients.
Clean latrine: It is said to be clean when it is with no faces on or near the sets of the latrine and have not been disturbed by flies.
Safe/clean/water: When piped or protected well water in the health center available and observed in the ANC counseling and examination room for use.
Structure refers to the conditions under which care is provided. Structural attributes in this study included; human resources (number, variety, qualification of professionals), material resources (infrastructure, equipment and supplies such as sphygmomanometer, foetal scope, tape measure and thermometer etc.).
Process quality refers to activities that constitute health care and interaction between client and care giver. Process in this study included time of initial ANC visit and frequency of visits and client provider interaction. Technical aspect s included history taking, physical examination (general and systematic and blood pressure), and laboratory investigations (blood for VDRL, hemoglobin, and HIV, urine testing for albumin). Process quality also looked at treatment prescription of prophylactic treatments like (Iron and TTV), provision of health promotion messages (specifically on diet, delivery preparation, and obstetric complications) and referral system. It was measured based on the subjects answer for service provision and observation of consultation session with checklist.
Outcome quality according to Donavedian’s changes (desirable or undesirable) in individuals and population that can be attributed to health care provided. Outcomes in this study included women’s satisfaction with the service provided. Here the affirmative answer for the outcome category question assumed to measure the satisfaction level of the respondents.
Provider - client interaction: It is the process of reciprocal action or influence under taken between the service provider and the client. In this study it was measured in terms of inter personal aspects such as privacy‚ confidentiality‚ explaining procedures‚ treating with empathy‚ respect and friendly greeting‚ counseling on birth preparedness complication readiness‚ nutrition‚ consultation time and technical aspects include history taking‚ examination and counseling and it was measured in terms of client view and observation of the service provision during consultation.
Monthly income: It was measured on daily income of workers based on 2013 millennium development report which was used to classify workers in developing country as extremely poor‚ moderately poor‚ near poor‚ developing middle class and developed middle class based on their daily income of (<$1.25‚ ≥$1.25and $2‚ ≥2 $ and $4‚ ≥$4 and <$13 and >$13) dollars respectively. By changing the dollar to current currency that is one USA dollar is equal to 19 Ethiopian birr then this daily income was converted into monthly income of respondents [30].
Data Processing and Analysis
For quantitative data, the response was coded and entered into the computer using EPI Data version 3.1 statistical packages. Data was cleaned accordingly and then exported to SPSS version 20.0 (IBM) for analysis. Descriptive statistics such as frequencies‚ mean‚ median‚ SD‚ percentage was carried out to see the distribution of the study subjects with the variables under the study. The result of the analysis was presented in tables and graphs as appropriate. Bivariate analysis was carried out to select variables for multivariate analysis. Multivariable analysis was carried out to identify factors associated with client satisfaction of quality of ANC service controlling the effect of confounding variables.
A p- value <0.05 was considered as statistically significant. Adjusted odds ratios were used to see the strength of association with 95% CI. Variables with p value <0.25 in the bivariate analysis was candidates for multivariable analysis. Finally the final model was constructed using stepwise logistic regression method.
Qualitative data was analyzed thematically by manually. The results were triangulated with quantitative data so as to strengthen the findings.
Data Quality Management
Training was given for both data collectors and supervisor by the principal investigator for two days. The training covered the objectives of the study ‘method of data collection.
Pre-testing of the questionnaire was carried out on 5% pregnant women at Buli ke health center which is found in the adjacent woreda of the study area in order to evaluate the wording‚ logic behind and consequently edited and used the most applicable questions.
During actual data collection at the end of each day, the questionnaire was checked for completeness, accuracy and consistency by the supervisors and investigator and corrective action was under taken with all the data collectors and the supervisors.
The raw data from the in-depth Interviews was analyzed using content analysis procedures. The audiotapes from the Indepth interviews were transcribed and comparison with written notes was done for completeness, accuracy and as a data quality assurance measure. Each typed transcript was checked against the audiotape by principal investigator before being translated into English. The written transcripts from each interview were read and key words and significant statements were highlighted. The identified themes and sub themes that emerged from each interview were reviewed by the researcher and similar themes was grouped together. Significant statements for each theme was identified and triangulated into the quantitative data to give in-depth analysis of the quality of ANC at Demba Gofa woreda.
Ethical consideration
Ethical clearance was obtained from Ethical Review Committee of college of public health and Medical sciences of Jimma University before the start of the study. Written cooperation letter was obtained from Demba Gofa woreda health department and from the respective health facilities. All the study participants (both clients and providers) were informed about the purpose of the study and finally verbal consent was obtained before interview or observation. The respondents have the right to refuse participation or terminate their involvement at any point during the interview. The information provided by each respondent was kept confidential. Furthermore, report writing was not referred a specific respondent with identifier.
Results
Socio demographic attribute
The response rate was 98.8%. The mean age of respondent was 29.94 with SD‚ 4.3 years. Its range was twenty two. The mean and range of numbers of pregnancy were 2.68 with SD of 1.365 number of pregnancy and seven respectively. The average income and range of the respondents were 379.67 with (SD‚ 365) birr‚ 1950 (minimum 50 birr and maximum 2000 birr) respectively. Three hundred seventy three (89.2%) of the respondents were pregnant before and also 368 (88%) of the mothers were married. 21 (5%) ‚ 12(2.9%) and 3(0.7%) were single‚ divorced and widowed respectively (Table 1).
Table 1 Socio demographic characteristics of respondents in Demba Gofa woreda, March - April 2014.
| Factor |
|
Number |
Percent |
| Occupation |
House wife |
237 |
56.7 |
| |
Government employee |
57 |
13.6 |
| |
Merchant |
54 |
12.9 |
| |
Other* |
42 |
10 |
| Education status |
No formal education |
51 |
12.2 |
| |
Primary |
166 |
39.7 |
| |
High school and above |
198 |
47.4 |
| Religion |
Protestant |
261 |
62.4 |
| |
Orthodox |
102 |
24.4 |
| |
Muslim |
50 |
12 |
| |
other** |
3 |
0.7 |
| Language |
Gofatho |
385 |
93.4 |
| |
Gammotho |
6 |
1.5 |
| |
Amharic |
21 |
5.1 |
| Marital status |
Married |
368 |
91 |
| |
Single |
21 |
5.2 |
| |
Divorced |
12 |
2.9 |
| |
Widowed |
3 |
0.7 |
| Number of pregnancy |
Primigravida |
150 |
35.8 |
| |
Multigravida |
2 48 |
59.3 |
| |
Grandmulti |
21 |
5 |
| Age |
<20 |
60 |
14.4 |
| |
20 -34 |
295 |
70.6 |
| |
35-49 |
14 |
3.3 |
| Income |
<712ETH |
143 |
34.2 |
| |
712.5 - 1139ETH |
270 |
64.6 |
| |
1140 - 2280ETH |
5 |
1.2 |
| |
|
|
|
Others* students** Catholics and Adventists
Structural quality attribute
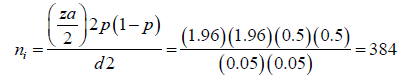
Two hundred sixteen (51.7%) were not comfortable with the waiting area. 30 years old woman noticed her experience as follows: “I really like that they take the time for me to just go through my list of questions. “But I dislike when they made me to stay long time in their uncomfortable and with no seat waiting place”. Likewise‚ 243 (58.1%) and 105 (25.1%) were not comfortable with the toilet and examination bed respectively. Whereas 318 (74.9) and 252 (60.3%) of mothers were comfortable with examination bed and working hours of health center respectively. Provider schedule appointment for the next ANC visit was appropriate for 318 (76.1%). Two hundred fifty six (61.2%) mothers waiting time was long, and for 254 (60.8%) mothers the health facility was not the closest.
As 28 year old women reported‚ ‘it is actually not quite convenient because I cannot walk there on nice days because it is far from my house” A 31 year old woman described that:” My home is very far from the health center as well the road to the health center is mountains in addition it takes me more than six hour to reach the health center‚ imagine how much hour will a single ANC visit take me a day”.
Sixty four (15.3%) mothers were paying for the service with average 19.52 (SD±7.2) birr. A 21 year old Midwifery described her view as follows: “They might pay for the services whenever they are seen at outpatient department but this is not appropriate for cases related to pregnancy and recommended components of services to be delivered free of charge‚ they should have been told to visit ANC clinic for free services' how ever did not”.
Those mothers who did not go back without getting the service because of the absence of the providers accounted 67 (16%) whereas those mothers who did not get the service accounted for 351 (84%). Mothers who did miss the service as a result of lack of money were 371 (88.8%) where as those did not miss accounted 47 (11.2%) (Figure 2).
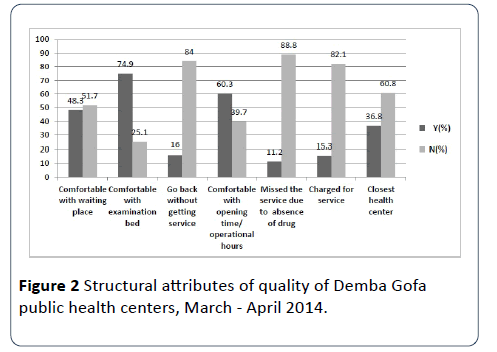
Figure 2: Structural attributes of quality of Demba Gofa public health centers, March - April 2014.
Skilled health personal and providers training situation
According to the inventory result‚ the overall skilled health personal gap was 67.18% nursing professionals was excluded since it was in excess from the National standard. With regard to training almost all of the health personals had not taken training on FANC with in twelve months of the survey. The minimum required number‚ actual availability and the gap in each health center were presented (Table 2).
Table 2 Availability of skilled health human resources in Demba Gofa woreda public health centers March- April‚ 2014.
| |
Nursing professionals |
Environmental |
Laboratory technician |
Pharmacy technician |
HO/BSN |
Midwifery |
Total |
| Lote Health Center |
| Min. NO |
5 |
1 |
2 |
3 |
2 |
3 |
16 |
| Actual |
8 |
0 |
1 |
1 |
1 |
1 |
11 |
| Gap |
+3* |
1 |
1 |
2 |
1 |
2 |
5 |
| %Gap |
|
100 |
33.3 |
66.6 |
50 |
66.6 |
31.5 |
| Trained number |
|
|
|
|
|
2 |
|
| trainingarea |
|
|
|
|
|
EMOCandPMTCT |
|
| U/B Health Center |
| Min. NO |
5 |
1 |
2 |
3 |
2 |
3 |
16 |
| Actual |
9 |
0 |
0 |
1 |
1 |
1 |
12 |
| Gap |
+4* |
1 |
2 |
2 |
1 |
2 |
4 |
| %Gap |
|
100 |
100 |
66.6 |
50 |
66.6 |
25 |
| Trained number |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| Trainingarea |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| LAIMA Health Center |
| Min. NO |
5 |
1 |
2 |
3 |
2 |
3 |
16 |
| Actual |
11 |
0 |
0 |
0 |
0 |
2 |
13 |
| Gap |
+6* |
1 |
2 |
2 |
2 |
1 |
3 |
| %Gap |
|
100 |
100 |
100 |
100 |
33.3 |
23.1 |
| Trained Number |
0 |
0 |
0 |
0 |
0 |
1 |
|
| training area |
|
|
|
|
|
BEMOC |
|
| Dombe Health Center |
| Min. NO |
5 |
1 |
2 |
3 |
2 |
3 |
16 |
| Actual |
5 |
0 |
2 |
1 |
0 |
0 |
7 |
| Gap |
0 |
1 |
0 |
2 |
2 |
3 |
9 |
| %Gap |
0 |
100 |
100 |
66.6 |
100 |
100 |
43.8 |
| Over all gap% by excluding nursing professionals |
|
|
|
|
|
67.18 |
|
*excess when seen with respect to Ethiopian standard
Availability of essential drugs‚ basic equipments‚ selected laboratory tests and infra structures
The interview of service providers and observation of facilities showed that essential drugs such as amoxicillin or Augment in or Cotri-moxazole); Albendazole or mebendazole; the first-line antimalarials were available in the 4 public health facilities where as methyldopa (Aldomet)‚ iron folic and ferrous sulphate were absent in the majority of the health centers. However, pieces of equipment‚ thermometers, sphygmomanometers, vaginal speculum‚ fetoscope, measuring tape, blood pressure apparatus, stethoscope, adult weighing scale, and examination coach were available at the time of visiting in four facilities. Similarly the facilities have private consultation and examination rooms.
From the four health centers Uba barea‚ Lymatsala and Lote health centers do not have clean latrine facilities, clean water supply‚ and all health center do not have private ANC waiting area. Electricity is available in Lote and Dombe health center but not in U/barea and Lymatsala.
With regard to the availability of laboratory tests; in almost all health centers those selected laboratory tests were not under taken during the data collection period. But HIV test was under taken in all health centers.
Process quality attribute
Process attributes of care: interpersonal aspects: Three hundred twenty four (77.5) of mothers started ANC visit after first trimester. Two hundred ninety eight (71.3%) were not given iron pills. Two hundred twenty four (53.6%) had had short examination time. From the total participants 401 (95.9%) mothers prefer female care provider. For three hundred thirty two (79.6%) mothers’ procedure was explained. This was supported by finding from observation in which Women were invited to talk about their medical concerns in 38 (54.3%). Three hundred sixty two (79.6%) were examined respectfully. The qualitative component of the study (by observation) also supported that respectful and friendly greeting was offered for a total of 37 (52.9%) clients. Three hundred twenty one (76.7%) of mothers were not treated with empathy which was also supported by interruption of women speech was observed in 45 (64.3%) of consultations in the facilities. Likewise one hundred ninety eight (47.3%) of mothers had had discussion on nutrition with providers at this and previous visit of this pregnancy whereas 123 (29.4%) were advised on nutrition for this visit only for this pregnancy this finding was supported by the observation result 69 (98.6%) were advised. Women and antenatal care providers identified the importance of health promotion advice to encourage a healthy life style. Midwifery talked about taking time to address counseling about nutrition and appropriate weight gain was identified as an essential component of quality antenatal care. A 20 year old Midwifery described her approach to this as follows: “I think I do for more nutritional counseling than most people do because I do watch their weight gain and I do try to get them to have food three days a day or as needed and try to help them to bring the weight under control or the weight gain under control if it is getting a bit out of control”. A 33 year old woman reported that: “the nurse most of the time tells me to have variety food”. A 35 year old woman described her view as follows: “I usually visit the health center for checkup but most of the time they have not given me advice on nutrition in detail rather than saying eat more food than the usual”.
Ninety seven (23.3%) of mothers missed the opportunity of advice on nutrition for this pregnancy. With regard to birth preparedness‚ Two hundred thirty six (56.4%) of mothers were advised on birth preparedness on this and previous visit of this pregnancy. A 33 year old woman reported that: The nurse at most of the visit let me get prepared for birth in order to prevent problems at birth‚ for this she tells me to save money for transport‚ get programmed with a skilled attendant and the likes” Ninety seven (23.2%) of mothers had got the opportunity of getting advice for this visit only for this pregnancy. Eighty five (20.3%) of mothers were not advised on birth preparedness. A 33 year old woman reported that: “Most of my visits to the health center for ANC services I have not been advised about birth preparedness” In general, interpersonal aspects of quality were good, especially in relation to welcoming the patient and providing seat‚ talk about their medical concerns and respect.
Process attributes of care and technical aspects: The frequency of carrying out specific physical examinations revealed a heterogeneous picture. Some of the examinations were done very regularly (weighing, auscultation of the fetal heart, and palpation of the funds‚ taking blood pressure and the likes) in the public health centers of the woreda where as some of WHO recommended routine tests such as Anemia‚ blood grouping‚ any urine tests and syphilis tests were totally not performed for the observed clients (Table 3). With regard to iron prophylaxis in most of the health centers the services were not delivered during the data collection period for the study. The overall performance was considered weak in the facilities. For example, routine prophylaxis or well-known pregnancy-related risk factors such as anemia was only prescribed in a small proportion of consultations (Table 3).
Table 3 Services and procedures performed for ANC clients at the public health centers at Demba Gofa woreda, March-April‚ 2014.
| Service or procedures(N=70) |
N |
% |
| History taking |
| Client’s age |
70 |
100 |
| Medications the client is taking |
41 |
58.6 |
| Date client’s last menstrual period began |
56 |
80 |
| Number of prior pregnancies client has had |
50 |
71.4 |
| Physical examination |
| Take the client’s blood pressure |
66 |
94.3 |
| Weigh the client |
70 |
100 |
| Examine conjunctiva/palms for anemia |
63 |
90 |
| Examine legs/feet/hands for edema |
54 |
77.1 |
| Examine for swollen glands |
20 |
28.6 |
| Palpate the client’s abdomen for fetal presentation |
57 |
81.4 |
| Palpate the client’s abdomen for uterine height |
56 |
80 |
| Listen to the client’s abdomen for fetal heartbeat |
42 |
60 |
| Conduct an ultrasound/refer client for ultrasound/look at recent ultrasound report |
32 |
45.7 |
| Examine the client's breasts |
14 |
20 |
| Conduct vaginal examination/exam of perinea area |
11 |
15.7 |
| Measure fundal height using tape measure |
57 |
81.4 |
| Routine tests |
| Anemia ( hemoglobin) test |
70 |
0 |
| Blood grouping |
70 |
0 |
| Any urine test |
70 |
0 |
| Syphilis test |
70 |
0 |
| HIV counseling and testing |
| Asked if the client knew her HIV status |
69 |
98.6 |
| Provide counseling related to HIV test |
69 |
98.6 |
| Refer for counseling related to HIV test |
1 |
1.4 |
| Perform HIV test |
69 |
98.6 |
| Refer for HIV test |
1 |
1.4 |
| Maintaining healthy pregnancy |
| Discussed nutrition (i.e., quantity or quality of food to eat) during the pregnancy |
69 |
98.6 |
| Informed the client about the progress of the pregnancy |
50 |
71.4 |
| Discussed the importance of at least 4 ANC visits |
40 |
57.1 |
| Iron prophylaxis |
| Prescribed or gave iron pills or folic acid (IFA) or both |
8 |
11.4 |
| Explained the purpose of iron or folic acid |
6 |
8.6 |
| Explained how to take iron or folic-acid pills |
8 |
11.4 |
| Explained side effects of iron pills |
3 |
4.3 |
| Tetanus Toxoid Injection |
| Prescribed or gave a tetanus toxoid (TT) injection |
66 |
94.3 |
| Explained the purpose of the TT injection |
60 |
85.7 |
| Deworming |
| Prescribed or gave Mebendazole/Albendazole |
1 |
1.4 |
| Explained the purpose of Mebendazole/Albendazole |
1 |
1.4 |
| Malaria |
| Provided ITN to client or instructed client to obtain ITN elsewhere in facility |
67 |
95.7 |
| Explicitly explained importance of using ITN to client |
64 |
91.4 |
| Preparation for delivery |
| Asked the client where she will deliver |
64 |
91.4 |
| Advisedtheclienttopreparefordelivery(e.g.setasidemoney,arrangeforemergency transportation) |
66 |
94.3 |
| Advised the client to use a skilled health worker for delivery |
54 |
77.1 |
| Discussed with client what items to have on hand at home for emergencies |
19 |
27.1 |
| Health worker – women inter action (interpersonal aspect) |
| Interruption of women’s speech |
45 |
64.3 |
| Respect |
37 |
52.9 |
| Concerns of women asked about |
38 |
54.3 |
| Offering seat |
63 |
90 |
| Explaining procedure to women |
28 |
40 |
Concerning antenatal care service delivery‚ one hundred ninety eight (47.4%)‚ 123 (29.4%) were provided advice on nutrition in this and previous visits of this pregnancy respectively. whereas 97 (27.2%) of clients were not advised at all.
One hundred ninety five (46.7%)‚ one hundred eleven (26%) mothers were advised on danger signs of pregnancy on contrary one hundred twelve (26.8%) were not advised at all for this pregnancy of their visit.
Two hundred thirty six (56.5%) and ninety seven (23.2%) mothers were advised on birth preparedness on the other hand eighty five (20.3%) were not advised at all for the visits (Table 4).
Table 4 ANC service delivered for mothers at public health centers of Demba Gofa woreda, March - April‚ 2014.
| Characters |
Number |
Percent |
| Provider talk about nutrition |
| This and previous visit |
198 |
47.4 |
| On one of them |
123 |
29.4 |
| Not at all |
97 |
23.2 |
| Provider talk about danger sign |
| This and previous visit |
195 |
46.7 |
| On one of them |
111 |
26.6 |
| Not at all |
112 |
26.8 |
| Provider talk about birth preparedness |
| This and previous visit |
236 |
56.5 |
| On one of them |
97 |
23.2 |
| Not at all |
85 |
20.3 |
| Saved money to be used at the time of delivery |
| No |
232 |
55.6 |
| Yes |
185 |
44.6 |
| Examined respectfully |
| No |
51 |
12.3 |
| Yes |
362 |
87.6 |
| Decide place of birth |
| No |
34 |
8.5 |
| Yes |
362 |
86.6 |
| Where decided place of birth |
| Home |
109 |
28.3 |
| Health post |
39 |
10.1 |
| Health center |
232 |
60.7 |
| hospital |
2 |
0.5 |
| Provider explained about examination |
| No |
85 |
20.3 |
| Yes |
332 |
79.6 |
| Provider treated with empathy |
|
|
| Yes |
321 |
76.8 |
| No |
97 |
23.2 |
| Provider treated equally |
| Yes |
307 |
73.4 |
| NO |
111 |
26.6 |
Women’s satisfaction with antenatal care service was associated with frequency of the ANC visits. first visits were almost two times more likely unsatisfied than those who had follow up visit (AOR=1.9‚ 95% (1.1,3.3)‚ mothers who were not advised on nutrition were three times seemingly unsatisfied than those who were advised. (AOR=3.3, 95% CI: 1.3‚ 8.5), mothers who were not advised on birth preparedness were three times probably unsatisfied than those who were advised (AOR=3.3, 95% CI: 1.1‚ 9.3). Mothers whose homes not closer to health center were two times more likely unsatisfied than those who had closer home (AOR=2.3‚ 95% CI: 1.3‚ 3.9). Mothers who were charged for service were three times (AOR 3.4‚ 95% CI: (1.2‚ 9.5) more likely unsatisfied than those who were not charged. Mothers who were provided iron pills in one of the visit were 99.86% times less likely unsatisfied than those who were not provided iron at all. (AOR= 0.14‚ 95% CI; 0.05‚ 0.3).
They were statistically significant and associated with overall satisfaction level of ANC service (Table 5).
Table 5 Predictors of client satisfaction greater than 75% satisfaction level among ANC attending pregnant women at four public health centers in South west‚ Ethiopia, March-April‚ 2014.
| |
Satisfaction, n (%) |
|
|
|
| Predictor Variables |
satisfied |
unsatisfied |
COR (95%CI) |
AOR (95%CI) |
p.v |
| Frequency of ANC visit |
| First visit |
41(17.4) |
195(82.6) |
1.8 (1.1, 2.9) |
1.9 (1.1,3.3)* |
0.03 |
| Revisit |
45(27.6) |
118(72.4) |
1.0 |
1.0 |
|
| Irion pills provision |
| This and previous visit |
16(45.7) |
19(54.3) |
1.6(0.7‚3.6) |
|
|
| This visit |
29(34.1) |
56(65.9) |
4.7(2.2‚ 9.8 ) |
0.14(0.05‚ 0.3) |
<0.01 |
| Not at all |
45(15.1) |
253(84.9) |
1 |
1 |
|
| Talked on nutrition |
| This and previous |
53(26.8) |
145(73.2) |
1 |
1 |
|
| This visit |
22(17.9) |
101(82.1) |
1.6 (0.9, 2.9) |
|
|
| Not at all |
15(15.5) |
82(84.5) |
1.9 (1.0, 3.8) |
3.3(1.3‚ 8.5)* |
0.01 |
| Talked on birth preparedness |
| This and previous |
59(25.0) |
177(75.0) |
1 |
1 |
|
| This visit |
17(17.5) |
80(82.5) |
1.5 (0.8, 2.8) |
|
0.02 |
| Not at all |
14(16.5) |
71(83.5) |
1.6 (0.8, 3.2) |
3.3(1.1‚9.3)* |
0.02 |
| Closest health center |
| No |
40(15.7) |
214(84.3) |
2.2(1.3,3.5)* |
2.3(1.3‚3.9)* |
0.006 |
| Yes |
45(29.2) |
109(70.8) |
1 |
1 |
|
| Charge for the services |
| Yes |
82(23.9) |
261(76.1) |
3.03(1.2,7.2)* |
3.4(1.2‚9.5)* |
0.02 |
| No |
6(9.4) |
58(90.6) |
1 |
1 |
|
*Statistically significant at p-value < 0.05‚ adjusted for explain about examination‚ treated with empathy‚ treated respectfully‚ comfortable with waiting place‚ waiting time‚ initiation of ANC visit‚ time of consultation and advice on danger sign of pregnancy.
Model description
Variables significant at bivariate analysis with p -value less than 0.25 were included in the multiple variable logistic regressions. Multicollinearity between explanatory variables was checked via co-linearity diagnosis using variance inflation factor greater than 10 and tolerance value less than 0.1. Assumption of logistic regression was checked by Hosmer- Lemeshow goodness of-fit-test, result 0.22.
Outcome attribute
Client satisfaction was rated by 12 items each having five point Likert scale from strongly disagree (1) to strongly agree (5) as shown in Table 6 which has internal reliability (Cronbach’s α of 0.894). This shows that the items were internally consistent. To see the total score of each respondent, the points obtained from the 12 items by each respondent were computed. A respondent had a minimum 13 and a maximum of 60 points on ANC satisfaction. Its mean and median were 39.74 and 41 respectively. Clients were categorized as not satisfied for strongly disagree‚ disagree and neutral and or satisfied for strongly agree and agree. The overall satisfaction percentage of the client was 21.5% with (CI 17.9‚ 25.6%) that means from 60 maximum points mothers who responded 45 and above points were regarded as they were satisfied and otherwise not. The cut point 75% was used since it is usually recommended percentage and preferred by the public to be said on the safest side of the quality of the service provided [31].
Table 6 Respondents satisfaction level on each category of outcome quality attribute among antenatal clients of Demba Gofa woreda public health centers March - April 2014.
| Items |
Strongly disagree |
disagree |
neutral |
agree |
Strongly agree |
Mean (SD) |
| Waiting time was faire |
17(4.1) |
59(14.1) |
220(52.6) |
103(24.6) |
19(4.5) |
3.1(0.8) |
| Understand what the provider said |
30(7.2) |
38(9.1) |
149(35.6) |
165(39.5) |
36(8.6) |
3.3(1.0) |
| Received full information |
47(11.2 |
27(6.5) |
129(30.9) |
165(39.5) |
50(12.0 |
3.3(1.1) |
| Waiting area was adequate and with seat |
17(4.1) |
104(24.9 |
129(30.9) |
141(33.7) |
27(6.5) |
3.1(0.9) |
| Privacy during consultation |
63(15.1) |
75(17.9) |
99(23.7) |
125(29.9) |
56(13.4 |
3.1(1.2) |
| Greeting was good |
44(10.5) |
40(9.6) |
133(31.8) |
144(34.4) |
57(13.6 |
3.3(1.1) |
| Opening and operation time appropriate |
67(16.0) |
39(9.3) |
107(25.6) |
154(36.8) |
51(12.2 |
3.2(1.2) |
| Health center has clean latrineand adequate water supply |
10(2.4) |
183(43.) |
123(29.4) |
69(16.5) |
33(7.9) |
2.8(0.9) |
| You will continue the rest visit in this H/C |
33(7.9) |
40(9.6) |
103(24.6) |
69(16.5) |
33(7.9) |
3.4(1.1) |
| Cost was faire |
42(10.0) |
33(7.9) |
59(14.1) |
113(27.0) |
171(40.9) |
3.8(1.3) |
| Recommend this HC for your relatives |
18(4.3) |
39(9.3) |
102(24.4) |
204(48.8) |
55(13.2) |
3.5(0.9) |
| You are happy with service provided today |
26(6.2) |
36(8.6) |
107(25.6) |
182(43.5) |
67(16) |
3.5(1.1) |
Dissatisfaction was highest (78.5%) among women receiving ANC at Demba Gofa woreda public health centers. In this regard 318 (75.5%) of mothers were dissatisfied with that the health center has clean latrine and adequate water supply‚ two hundred ninety six (70.9%) of clients were dissatisfied with waiting time was faire and two hundred fifty three (60%) of clients were dissatisfied with waiting area was adequate and with seat. Of all satisfaction levels, cost for service was faire related satisfaction 286 (67%), recommending relatives and others to attend the service at this health center 260 (61.1%)‚ general happiness with the service provided today 251 (59.1%) and continuing the rest ANC visit in this health center 247 (58.1%) were the highest four satisfaction levels (Table 7).
Table 7 Category of care and satisfaction level by dichotomizing strongly disagree‚ disagree and neutral to not satisfied and strongly agree and agree to satisfied mother who received ANC in public health facilities of Demba Gofa, March –April 2014.
| Categoryof care |
|
Number |
Percent |
| waiting time was faire |
Satisfied |
122 |
29.1 |
| Unsatisfied |
296 |
70.9 |
| The provider was easy to understand |
Satisfied |
201 |
48.1 |
| Unsatisfied |
217 |
51.9 |
| Received full information about ANC today |
Satisfied |
215 |
51.4 |
| Unsatisfied |
203 |
48.6 |
| Waiting area was adequate and with seat |
Satisfied |
169 |
40 |
| Unsatisfied |
253 |
60 |
| Privacy during consultation was maintained |
Satisfied |
187 |
43.8 |
| Unsatisfied |
237 |
56.2 |
| Provider’s greeting was good and in a friendly way |
Satisfied |
205 |
48.4 |
| Unsatisfied |
218 |
51.6 |
| The hours of opening and operation time of the H/c is appropriate |
Satisfied |
208 |
49.1 |
| Unsatisfied |
216 |
50.9 |
| The H/C has clean latrine and adequate water supply |
Satisfied |
104 |
24.5 |
| Unsatisfied |
318 |
75.5 |
| You want to continue the rest ANC visits in this H/C |
Satisfied |
247 |
58.1 |
| Unsatisfied |
175 |
41.9 |
| Cost for services or treatmentswas fair |
Satisfied |
286 |
67.3 |
| Unsatisfied |
134 |
32.7 |
| You recommend your relatives and others to attend the H/C |
Satisfied |
260 |
61.1 |
| Unsatisfied |
159 |
38.9 |
| Generally you are happy with all the services you have got today |
Satisfied |
251 |
59.1 |
| Unsatisfied |
162 |
40.9 |
| Overall satisfaction percentage |
21.5 |
Discussion
The study estimated the level of mothers’ satisfaction with antenatal care services at Demba Gofa woreda public health centers at Gammo Gofa Zone in South west Ethiopia. The overall proportion of mothers who were satisfied with antenatal care in this study was 21.5% with (95% CI:17.9%, 25.6%). This percentage is very low compared to other studies in developing countries 81.4% in South west Nigeria [32-40]. In this study ANC mothers satisfaction was predicted by frequency of ANC visit, advise on nutrition, advise on birth preparedness‚ charge for service‚ provision of iron pills and closeness of the health center to pregnant women home. This finding is inconsistent with other studies in Africa [26,32]. This much variation in satisfaction of the service might be explained by lack of orientation on FANC for providers‚ supplies‚ skilled human resource ‘not undertaking the recommended intervention‚ the absence of the pro vider in due time and the expectation of mothers.
Mothers who had first ANC visit were almost two times more likely to be unsatisfied than mothers who had follow up visit. Similar finding was reported in Ethiopia [26]. This might be justified by understanding the benefit of the service‚ familiarity with provider and experience.
The study also showed that mothers who had not got advice on nutrition and birth preparedness and complication readiness were three times more likely to be unsatisfied than mothers who were advised [8,33-35]. This might be explained by the awareness and experience of the clients with regard to the services as well as expectation. Mothers whose homes at long distance from health center were two times more likely unsatisfied than those who were at short distance [32,36-38]. This might be justified by the consumption of the time to reach the health center‚ after arrival the fear of absence of the provider‚ the required drugs and supplies and the work load at home might disappoint. Mothers who were not advised on nutrition were three times more likely unsatisfied than those who were not. This finding is in line with finding in Nigeria [39]. Nutrition is a fundamental pillar of human life and its requirement varies with respect to age, gender and during physiological changes such as pregnancy. Clinical implication of nutrition and birth preparedness. Many women suffer from a combination of chronic energy deficiency, poor weight gain in pregnancy, anemia, and other micronutrient deficiencies, as well as infections like HIV and malaria. These along with inadequate obstetric care, contribute to high rates of maternal mortality and poor birth outcome. Those mothers who were charged for service were three times more likely unsatisfied than those who were not charged. This finding is in agreement with finding in Northern Ethiopia [28]. Those mothers who received iron in one of the visits were 99.86% less likely unsatisfied than those who were not provided at all.
The results revealed the health Centres had inadequate number of skilled personnel to attend to pregnant women at the antenatal clinic. The number was inadequate compared to the minimum number of skilled personal required in public health facilities according to National standard [29] and considering the required services and counseling to be provided. This had an implication on the quality of the services delivered because lack of the required skilled professionals will result in increase in waiting time of the clients and decrease in access of the service [40].
The situation in the Woreda is in agreement with the national situation in Ethiopia where other studies have identified low staff levels in most government health facilities to provide required services of proper infrastructure for providing ANC compared to the standards was identified at the health centres [29]. Antenatal women had to wait for the services outside on the ground due to lack of proper structure such as absence of private waiting area and seats‚ clean latrine‚ lack of clean water supply.
The findings was consistent with another study [26] Where findings showed that there was no proper structures for providing ANC in most public health centers which hindered most women from reporting for ANC. The finding from inventory and observation entails lack of readiness to provide ANC at the facility. There was also severe shortage of material resources for providing ANC identified at the Health Centre. The health center had shortage of vital supplies for providing ANC like, reagents for VDRL check, urine analysis, hemoglobin‚ Rh and blood grouping‚ ANC drugs like iron and others as the in-depth interview result from health center head‚ laboratory technologist‚ druggist and ANC provider ascertained. Both women and health care providers discussed the value of screening and assessment as part of quality of antenatal care: A25 year women talked “primarily about the tests and measurements that provide reassurance the pregnancy and fetal development were progressing normally.”
As one woman commented‚ “Every time they check me really they check weight blood pressure and the likes but they did not do laboratory tests”. A 26 year old Antenatal care provider noted the importance of following guidelines for screening in pregnant to ensure better out comes for mothers and babies. “However majority of laboratory tests such as blood grouping‚ Rh factor syphilis test‚ any urine tests and a nemia tests were not done due to lack of reagents and other resources” the heads of the of health centers confirmed that “we did not under take some laboratory tests since we lacked resources in this regard.
In addition there was inconsistent availability of the supplies. Shortage of material resources supports earlier findings where most public health centers in some study area lacked necessary equipment and supplies like iron, speculum and sphygmomanometers for providing maternal care services [41]. Similar observations were made by WHO, where many public health centers especially developing countries lacked basic supplies and equipment for provision of quality of maternal services which resulted in compromising quality [15]. In agreement with the finding, studies in Eastern Uganda [34] revealed that the quality of ANC in most public health facilities is affected by lack of necessary equipment and resources compared to private facilities mainly due to inadequate funding. This finding implied that the women were denied of services requiring materials which were not available. The study further revealed that the majority of women in Demba Gofa attended antenatal clinic. Despite high antenatal attendance in this study, most women started ANC late that is after first trimester (ideally after 16 weeks) contrary to WHO recommendation of initiation of antenatal care before sixteen weeks [42].
Late starting was due to effect of distance of the health center from clients home and accessibility issue. The clinical implication of late initiation of ANC is the missed opportunity for early intervention for a large proportion of pregnant women in Demba Gofa health centers. This implies that messages regarding the importance of early initiation of ANC have not made any significant impact in the area. The study findings further revealed the skilled staffs at all health centers were not trained on FANC, the new approach proved to have an impact on maternal mortality.
The staff providing ANC concentrated on examinations proven to have less impact on maternal health like weighing, auscultation of the fetal heart and palpation of the funds. Other important examination like, urine and VDRL testing bold grouping and Rh factors and syphilis testes were not done to majority of clients due to lack of reagents and other resources as the qualitative findings from inventory‚ observation and in depth interview revealed. This implied identification of preexisting health conditions that may affect outcome of pregnancies such as anemia, and other sexually transmitted infections were not offered. Such missed opportunities should be regarded as indicators of unsatisfactory quality of ANC services. However the finding could be due to lack of staff training on FANC, and lack of resources. Inadequate staff training or lack of refresher courses to upgrade staff skills on maternal health have also been reported in some studies.
Study findings revealed that health education on HIV, and diet was given to most women during ANC follow up. However other important information like danger signs, after birth complications, and plan for delivery which are emphasized in FANC were not given to some of the antenatal women. This result consistent with a finding in another study on quality where most health workers in public health centers did not dwell much on educating women on topics like danger signs and birth plan during pregnancy. This implied that emergencies and complicated pregnancies were good time. Women in the survey perceived ANC at Demba Gofa public health centres as unsatisfactory. In line with the survey findings, the qualitative data especially the in-depth interviews with ANC provider‚ laboratory technologists‚ druggists and head of health center key informants revealed none under taking of majority of the recommended ANC components due to the fore mentioned reasons. Two hundred fourteen (83.6%) of mothers perceived long waiting hour were reported were strengthened during in-depth interview with pregnant women in the study. Unsatisfaction in the survey could either mean lack of required services‚ long waiting time‚ accessibility issues like financial and physical accessibility by women on what care they could expect at the antenatal clinic or could mean clients avoiding the risk of being denied care during the next visit or clients may also say they are satisfied with care because they want to please the interviewer, worry that care may be withheld in future, or they have cultural reason to fear complaining.
Strength of the study
The study has utilized different methods of data collection as well it was triangulated with qualitative findings. This could increase the validity of the result and the study.
Limitations of the Study
Hawthorn effect: It was the presence of an observer during the client -provider interaction, which might have improved provider performance, as well as reduced client openness, in response to the fact that they are being observed.
Social desirability bias: This was tried to minimize by interviewing mothers in a separate place by trained nurses who are not affiliated with the facilities studied.
Conclusion
The study findings revealed that ANC provided at Demba Gofa public health Centres were below the required standards: The overall satisfaction of antenatal care services in this study was found to be low. First ANC visit‚ lack of advice on nutrition‚ lack of advice on birth preparedness‚ farness of the health center to mother’s home‚ provision of iron and Charge for service were independently associated with mothers unsatisfaction of antenatal care.
Health workers were not implementing current recommended ANC approach known as FANC because they were not oriented at all. In addition unsatisfactory quality was due to lack of proper infrastructure for providing ANC, and inadequate capacity to deal to provide ANC to a large group of antenatal women, shortage of supplies and women in the survey perceived the care received as unsatisfactory which was also indicated by qualitative data lack of satisfaction with the ANC provided due to reasons which are concurring with the shortfalls identified shortage of staff, inadequate resources and lack of training on the new ANC approach for health personals on the quality of ANC at Demba Gofa woreda public health centers.
19344
References
- Igberase GO, Isah EC, Igbekoyi OF (2009) Awareness and perception of maternal mortality among women in semi-urban community in the Niger Delta of Nigeria. Ann Afr Med 8:261-265.
- World Health Organization(2010) WHO, UNICEF, UNFPA, The World Bank: Trends in maternal mortality: 1990 to 2008.
- HoHogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, et al. (2010) Maternal mortality for 181 countries, 1980-2008: A systematic analysis of progress towards Millennium Development Goal 5. Lancet 375:1609-1623.
- Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, et al.(2011) Stillbirths: Where? When? Why? How to make the data count? Lancet 377:1448-1463.
- Lawn JE, Yakoob MY, Haws RA, Soomro T, Darmstadt GL, et al. (2009) 3.2 million stillbirths: epidemiology and overview of the evidence review. BMC Pregnancy Childbirth 9:S2.
- Ministry Of Health (2011) Health and health related indicators, Ethiopia.
- Central Statistics Agency (CSA) and ORC Macro (2011) Demographic Health Survey Ethiopia, 2011, Addis Ababa, Ethiopia, CSA and Macro.
- Graham WJ, Varghese B (2012) Quality, quality, quality: gaps in the continuum of care. Lancet 379:e5-6.
- Broek NR, Graham WJ (2009) Quality of care for maternal and newborn health: The neglected agenda. BJOG 116:18-21.
- Donavedian A (1988) The quality of care. How can it be assessed? JAMA 260:1743- 1748.
- Maxwell RJ (1984) Quality assessment in health. Br Med J 288:1470-1472.
- World Health Organization (2006) WHO: Quality of care: A process for making strategic choices in health systems.
- No Authors Listed (2001) Institute of Medicine: Crossing the quality chasm: a new health system for the 21st Century. National Academies Press, Washington, DC.
- Kotelchuck M (1994) An evaluation of the kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. Am J Public Health 84:1414-1420.
- Beeckman K, Louckx F, Masuy-Stroobant G, Downe S, Putman K (2011) The development and application of a new tool to assess the adequacy of the content and timing of antenatal care. BMC Health Serv Res 11:213.
- Rani M, Bonu S, Harvey S (2008) Differentials in the quality of antenatal care in India. Int J Qual Health Care 20:62-71.
- Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, et al.(2007) Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG -5 targets. BMC Pregnancy Childbirth 7:29.
- Naariyong S, Poudel KC, Rahman M, Yasuoka J, Otsuka K, et al. (2011) Quality of antenatal are services in the Birim north district of Ghana: contribution of the community-based health planning and services program. Matern Child Health J 14:14.
- DonabedianA (2003) An introduction to quality assurance in health care. (1stedn). Oxford University Press, New York.
- White, Glazier (2011) Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Medicine9:58.
- Federal Democratic Republic of Ethiopia/Population Census Commission(FDRE/PCC) (2008) Summary and staistical report of the 2007 population and housing census: Population size by age and sex. Addis Ababa-FDRE/PCC.
- Ejigu T, Woldie M, Kifle Y (2013) Quality of antenatal care services at public health facilities of Bahir-Dar special zone, Northwest Ethiopia. BMC Health Services Res 13: 443.
- Pascoe GC (1983) Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann 6:185-210.
- Tayelgn A, Zegeye DT, Kebede Y (2011) Mothers’ satisfaction with referral hospital delivery service in Amhara Region, Ethiopia. BMC Pregnancy and Childbirth 11:78.
- Ethiopian standard agency (2012) Health center requirements, in human resource management and service standards.
- (2013) United Nations: The millennium development goals report New York.
- Sorra JS, Nieva VF (2004) Hospital survey on patient safety culture: Agency for healthcare research and quality U.S. 2004.
- Banda I, Hazemba A, (2012) Factorsassociated withlateantenatal careattendance in selected rural and urban communities of the copper belt province of Zambia 2012.
- Ramani VK, Radigan AM (2013) Quality of prenatal care as it relates to the source of prenatal care. Int J Med Public Health 3: 261-266.
- Tetu M(2013) Quality of antenatal care services in eastern Uganda: Implications for interventions.
- Onyango-Ouma HBW(2006) Acceptability and sustainability of the who focused antenatal care package in Kenya.
- Nyamtema (2012) The quality of antenatal care in rural Tanzania: What is behind the number of visits? BMC Pregnancy and Childbirth12:70.
- Kyei NNA, Gabrysch S (2012) The influence of distance and level of service provision on antenatal care use in rural Zambia.
- EL-Hamed NA, Helal RM, Megahed WM (2012). Egyptian women's satisfaction and perception of antenatal care: International J Trop Disease Health 2: 145-156.
- Nwaeze IL, Enabor TAO, Aimakhu CO (2013) Perception and satisfaction with quality of antenatal care services among pregnant women at the university college hospital, ibadan, Nigeria. Ann IbdPg Med 11: 22-28.
- Oladapo OT, Osiberu MO (2008) Do Socio demographic characteristics of pregnant women determine their perception of antenatal care quality? Maternal Child Health J.
- WorkuAG,WorkuAY,FentahunMA (2013)Availabilityandcomponentsofmaternityservices according to providers’ users perspectives in North Gondar North west Ethiopia. 10:43.
- USAID (2013)Focused antenatal care: A better, cheaper, faster, evidence–based approach.