Keywords
Infection; Nosocomial infection; NICU; Risk factors; Neonates
Introduction
Although it has been a long time since nosocomial infections in Neonatal Intensive Care Units (NICUs) have been described, they hardly recently have been recognized as one of the problems of importance [1-3] for premature infants hospitalized in NICU [4].
U.S. Center for Disease Control and Prevention (CDC) defines as Nosocomial Infection the infection that occurs 48-72 hours after the admission of a person in the hospital, due to microbial agents either of the patient’s microbial flora or the hospital environment [5-7]. More specifically, CDC defines all the neonatal infections, acquired either at birth or during hospitalization, as nosocomials, unless there is evidence of transplacental transmission [8-10].
Nosocomial infections constitute one of the leading causes of morbidity and mortality in neonates in NICU [9,11,12] with serious effects on the quality of care, as they increase the duration and the cost of hospitalization [3,4,11-14].
The infections are frequent in NICU compared to neonatal wards15. Premature infants are prone because of the prematurity of their organic systems, the immaturity of their immune system [13], the low birth weight [10,13,16,17], the low gestational age [18], the intravascular catheters’ use and the prolonged duration of hospitalization [10,19,20]. In other studies, the use of parenteral nutrition has been associated with an increased risk of bacteremia and concomitant nosocomial infection [11,21,22].
However, according to several studies, the risk for nosocomial infections increases due to exposure to numerous health care staff and the use of invasive technology [13], as developments in NICU have allowed the survival of underweight and ill premature infants and at the same time have created risks for occurrence of nosocomial infections [9].
Every year, more than one million neonatal deaths are estimated worldwide [23]. Also, it has been estimated that nosocomial infections cause the 40% of neonatal deaths in developing countries [10]. A recent study in NICU, in Greece, showed that mortality of infants who developed nosocomial infections (due to a specific infectious agent) exceeds 45% [24].
The overall incidence of neonatal nosocomial infections is estimated to 30% [10]. The bacteremia is the most frequent nosocomial infection and it is responsible for 10% to 30% of cases [25]. Schulman et al. [26], indicate that the incidence of bacteremia due to central intravascular catheters rises from 2.1 to 6.4 per 1000 central catheter days respectively. In the study of Tavora et al. [10] pneumonia was the second most common nosocomial infection (8.6%), followed by the omphalitis (4.3%), surgical infections (2.4%) and the impetigo (1.2%). While 15.4% of premature neonates develop other infections including in particular meningitis, infections of the eyes, mouth or skin.
Studies carried out in NICU, in Greece indicate pneumonia due to the ventilator (35.2%) as the most frequent nosocomial infection, followed bacteremia (32.4%), infections of the urinary tract (19.7%) and surgical wound infections (12.7%) [27].
Methodology
The study was carried out in order to record and describe the risk factors for nosocomial infections in neonates hospitalized in NICUs.
This study is prospective cross-sectional and was realized in the NICUs (A and B) of the General Pediatric Hospital “Agia Sophia”, from November 2009 to May 2010 and the NICU of the General and Maternity Hospital “Helena Venizelou”, from January to August 2012.
The population of the study consisted of all the neonates (100%) who were admitted and hospitalized during the period of the study. Specifically, a total of 474 neonates were recorded, of which 51 in A NICU and 103 in B NICU of the General Pediatric Hospital “Agia Sophia” and 320 neonates in the NICU of the General and Maternity Hospital “Helena Venizelou”.
A record card of nosocomial infections constituted the instrument of the study. This card was created after an extended literature review about the ways of recording data in terms of surveillance of nosocomial infections [28].
The card-instrument of the study included data about Demographics (twenty-six parameters), Consumption of Antibiotics (seven parameters), Infections’ Surveillance (presence of infection, Microorganism Identity, Risk Factors: thirty three parameters), Clinical Identification of the Infection (twenty-seven parameters), Laboratory Confirmation of the Infection (twentyone parameters).
In order to carry out the study the researchers asked, via formal application, the permission of the Scientific Committee and the Administration of the hospitals. In addition, the oral and written consensus of everyone involved was obtained. Throughout the study no action that could be harmful for the health status of hospitalized neonates took place. Besides, the legal rights of newborns and their parents in privacy and confidentiality were protected.
Statistical Analysis
Statistical analysis was performed using descriptive statistics. The mean values, standard deviations (SD) and medians as well as interquartile ranges were used for the description of the quantitative variables, while absolute (N) and relative (%) frequencies were used for the description of the qualitative variables. For the comparisons of proportions Pearson's chisquare tests and Fisher's exact test were used, where appropriate. For the comparison of quantitative variables, between two groups, Student's t-test or the non-parametric Mann-Whitney test were used. Proportionally, for the comparison of quantitative variables, between more than two groups, parametric analysis of variance (ANOVA) was used. In order to control the type I error, due to multiple comparisons, the Bonferroni correction was used, whereby the significance level was set to 0.05 / n (n=number of comparisons). Data, concerning independent factors, associated with the occurrence of nosocomial infection, sepsis, primary bacteremia or their combination, was modeled using stepwise multiple logistic regression analysis. Adjusted odds ratios, with 95% confidence intervals, were computed from the results of the logistic regression analyses. All p values reported were two-tailed and the statistical significance was set at 0.05. Analyses were conducted using SPSS statistical software (version 18.0).
Results
In the context of present study, data concerning infections of 474 neonates hospitalized in NICUs was recorded. Premature newborns were 301; 63,5% of the total population of the research. To the 5.7% (27 of 474) of the neonates sepsis was diagnosed and to the 5.3% (25 of 474) of them primary bacteremia was recognized as well.
The mean age of the mother was 30.6 years (± 6.1 years). The nationality of the 60.9% of newborns was Hellenic. The mean birth weight was 2362.8 gr (± 866.9 gr) and the mean gestational age was 34.7 weeks (± 4.2 weeks). The majority of newborns were boys (54.5%). Additionally, 89.4% of the subjects were born in Athens and 93.2% were born in a public hospital.
65.2% of the neonates were premature; 14.3% were born before 29 weeks, 23.2% between 29-34 weeks and the remaining 27.7% between weeks 34-37. To the 11.1% of the neonates had been recognized intrauterine growth retardation (IUGR). 71.7% of the population of the study was born via caesarean section (CS) (Table 1).

Coagulase Negative Staphylococcus (CoNS), Candida and Klebsiella were the microbes recognized at significantly higher rates; 12.0%, 5.1% and 4.6% respectively. Microbes such as Vancomycin Resistant Enterococcus (3.8%), Enterobacter (3.2%) and Enterococcus (2.7%) were recorded in lower percentages. At even lower rates (0.4%), microbes such as Serratia Marcescens and Staphylococcus Haemoliticus were described (Table 2).

Regarding the kinds of nosocomial infections recorded in the study, 40,9% of the newborns developed sepsis (27 of 66) and 34.9% had a primary bacteremia (23 of 66). Only 9 neonates (13.7%) had an upper respiratory infection; while the colonization reached 7.2% (33 of 474 neonates). The incidence of the rest infections recorded during the study, enterocolitis, peritonitis, and thrombophlebitis due to intravenous therapy, was low (3%) (Table 3).

The duration of hospitalization (patients days) was significantly longer when a nosocomial infection occurred (38.8 ± 27.5 vs 11.1 ± 12 p<0.001). Additionally, in the case of a nosocomial infection, the gestational age was significantly lower (32.4 ± 4.7 vs 35.1 ± 4 με p<0.001), as well as the weight of the neonates, at birth and the admission to the NICU (1969.2 ± 876.6 vs 2470.7 ± 831.3 p<0.001+). Proportionally, a nosocomial infection prolonged the duration, expressed in days, of the intravenous therapy, of the use of Levin-nasogastric tube (28.9 ± 22 vs. 10.2 ± 12.2 p<0.001) as well as of the use of the umbilical artery catheter, of intubation (8.8 ± 11. vs. 5.2 ± 7.1 p<0.007), of all central catheters (22.7 ± 19.8 vs. 11.9 ± 11.1 p=0.012), of the use of N-CPAP and Hood (8.1 ± 7.5 vs. 2.4 ± 2.6 p<0.001) (Table 4).

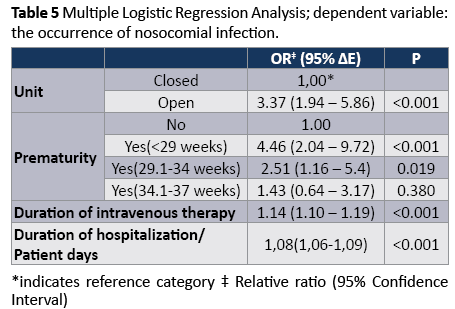
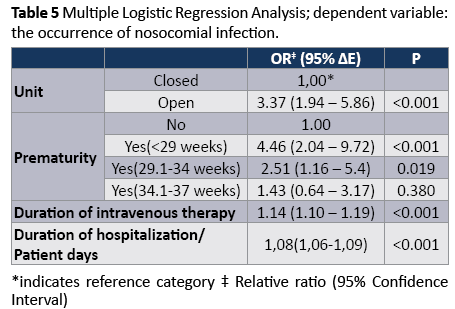
Eventually, by the multiple logistic regression analysis (considering “nosocomial infection” as the dependent variable) and by the stepwise multiple logistic regression analysis, it became obvious that the kind of unit, the prematurity of the neonate, the duration of intravenous therapy and the duration of hospitalization were independently associated with the occurrence of nosocomial infection. So, neonates hospitalized in an open unit were 3.37 times more likely to develop a nosocomial infection, compared with those hospitalized in a closed unit (OR 3.37, 95% CI 1.94 to 5.86, p<0,001). Respectively, neonates with gestational age lower than 29 weeks were 4.46 times more likely to develop a nosocomial infection, compared with those who were not born prematurely (OR 4.46, 95% CI 2.04 to 9.72, p<0,001). Finally, prolonging the duration of the intravenous therapy (OR 1.14, 95% CI 1.10 to 1.19. P <0.001) and of the hospitalization the likelihood of nosocomial infection increased (Table 5).
Discussion
In present study, mother’s mean age was estimated to 30.6 years. This point is in accordance with Bilali et al. [29], who claimed that the young age of the mother constitutes a risk factor of importance for nosocomial infections.
The mean gestational age was less than 36 weeks. According to Glen Mayhall [9] Heath et al. [11] Schulman et al. [26] and Bilali et al. [29], gestational age is described as a determinant key for the increased risk of acquiring nosocomial infections.
The majority of newborns were boys, but in most of studies, although boys seem to be hospitalized in NICUs in higher rates compared to girls, the gender of the neonate was not associated with the risk of a nosocomial infection. On the other hand, birth weight was the most important factor that was positively correlated with the occurrence of nosocomial infections. The mean birth weight was less than 2.5 Kg, which indicates that, in broader terms, the neonates of the study were underweight. This finding is consistent with the studies of Goldmann [16], Tavora et al. [10], Decembrino et al. [13], Umscheid et al. [30] and Bilali et al. [29], which showed that newborns are prone to infections because of the low birth weight. Also, this finding was confirmed by the studies of Glen Mayhall [9] and Heath et al. [11], where the infections in neonates seem to be inversely proportional to birth weight; the lower is the birth weight ,the higher is the risk for nosocomial infection.
Most of neonates were born in a public hospital. This fact makes difficult the connection of public or private sector with the risk for nosocomial infections. Also, a great percentage of the subjects were hospitalized in a limited unit (NICU); specifically in the General and Maternity Hospital “Helena Venizelou”. This finding is consistent with Van der Zwet et al. [15], who claimed that infections are more common in the NICU compared with neonatal wards.
Approximately, six out of ten of the neonates were born prematurely; (most of them during the 29th -37th week). This is in accordance with the studies of Heath et al. [11], where premature neonates are described as an extremely vulnerable population group at increased risk for nosocomial infections. Besides, Billali et al. [29], argued that sepsis in premature neonates is attributable to microorganisms, that colonize the NICUs and is associated with the increased frequency of necrotizing enterocolitis (NEC).
In the present study the majority of births were completed by cesarean section. In most studies, the cesarean section has not been associated with nosocomial infections. On the contrary, in the studies of Foca et al. [31] and Heath et al. [11], normal birth (vaginal delivery) is associated with nosocomial infections, such neonatal conjunctivitis mainly due to factors derived from the mother.
Staphylococcus Epidermidis, Candida and Klebsiella were the microbes found in significantly higher rates. These percentages are in accordance with the studies of Foca et al. [31], Gill et al. [12], Souli [32], Daikos et al. [33], Sydnor et al. [34] and Rasigade et al. [22], given that the coagulase -negative staphylococci (CoNS) are the most common infectious agents causing bacteremia in a NICU and are associated with higher morbidity and mortality. On the other hand, infections due to Serratia Marcescens, in this study were described in a small percentage, in contrast to the studies of Polilli et al. [35] and Maltezou [24], also carried out in Greece, who concluded that nosocomial infections in NICUs were septicemias caused by Serratia Μarcescens, with a high mortality.
Sepsis was the most frequent disease recorded followed by nosocomial infections with colonization, and primary bacteremia. But, in the studies of Heath et al. [11] and Tavora et al. [10] the bacteremia was the most frequent nosocomial infection, while septicemia was recognized in half of the cases and in the study of Foca et al. [31] the frequency of fulminant neonatal sepsis was recorded in high percentages.
More specifically, in this study, upper respiratory tract infection was recorded at 13.7% and enterocolitis at 3%. Proportionally, in the study of Heath et al. [11], infections of the lower respiratory tract (mainly pneumonia), as well as infections of the earnose- throat and urinary tract infections were described in high percentages. Present study is in accordance with the results of Billali et al. [29] who claimed that necrotizing enterocolitis (NEC) is the most common infection of the gastrointestinal tract for newborns with very low birth weight.
According the relative literature, the frequent use of invasive medical devices (central venous catheters, ventilators etc) for diagnostic or therapeutic purposes, is the most important risk factor for the occurrence of nosocomial infections. In the present study, intravenous interventions were described in most of the subjects with median duration 6.0 days. Also, Levin nasogastric catheter was placed in the majority of neonates with a median duration of 7 days. These findings are in accordance with the results of Umscheid et al. [30], Daikos et al. [33] who implicated factors such as the use of central venous catheters and the parenteral nutrition for the occurrence of nosocomial infections. Proportionally, Couto et al. [36], inter alia, claimed that the prolonged central venous catheterization increases the risk of infections of newborns hospitalized in NICU, and Heath, [11] recorded the increased incidence of infections per 1000 days catheter-related infections comparing to infections per 1000 days non-use of catheter.
Additionally, in the present study it was revealed that, when primary bacteremia or septicemia were present, intravenous devices- central intravenous catheters, Levin nasogastric catheters, catheters of the umbilical vein and Hood intubation’s use was significantly prolonged. While Heath et al. [11], Garland et al. [37], Arslan et al. [21], Rasigade et al. [22] concluded that, among other factors, intravascular catheters (mainly central), mechanical ventilation and parenteral nutrition are strongly associated with the increased risk of bacteremia.
This study, in full agreement with the existing literature, characterized mechanical ventilation as the major risk factor for lower respiratory nosocomial infections. Also, Couto et al. [36] and Heath et al. [11] highlighted intubation, a mechanical ventilation and their prolonged use as main factors that increase the risk of infections of newborns hospitalized in NICU. Proportionally, Heath et al. [11] and Maltezou [27] claimed that mechanical ventilation of neonates constitutes a particular risk factor for bacteremia and pneumonia due to ventilator.
Conclusions
In conclusion, nosocomial infections constitute one of the leading causes of morbidity and mortality of the neonates in NICUs and affect seriously the quality of their care. The present study revealed that factors such as low birth weight, prematurity, duration of hospitalization, the use of a central venous catheter and mechanical ventilation were significantly associated with increased incidence of nosocomial infections. Respectively, the interdisciplinary health professionals’ team should identify risk factors and implement strategies in order to reduce the rates of nosocomial infections in NICUs. Towards this direction, health professionals have to apply all the appropriate protocols when they use invasive methods and devices and adhere to all the principles and procedures of aseptic techniques.
5192
References
- Hellenic Center for Disease Control & Prevention, European Center for Disease Prevention and Control (2012) Point Prevalence Survey of Nosocomial Infections and Antimicrobial Use in Greek Hospitals. Manual of criteria and guidelines for the diagnosis, record and description of nosocomial infections (Criteria ECDC,2011).
- Dixon RE; Centers for Disease Control and Prevention (CDC) (2011) Control of health-care-associated infections, 1961-2011. MMWR Surveill Summ 60 Suppl 4: 58-63.
- Dedoukou X, Gourgoulis GM, Kontopidou F,Tsonou P, Papadima K, et al. (2011) Nosocomial Infections : National action plan ÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâ¦ââ¬Ã
ÂProkroustisÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂÃÂ. First results and next step. KEELPNO. Prospectus 2011.
- Cooley K, Grady S (2009) Minimizing catheter-related bloodstream infections: one unit's approach. Adv Neonatal Care 9: 209-226.
- Papadopoulos G, Kalovoulou L, Sofos AG (1997) Nosocomial Infections. Epidimiology-Prevention-Control. Parisianos, Athens.
- Kouchak F, Askarian M (2012) Nosocomial infections: the definition criteria. Iran J Med Sci 37: 72-73.
- Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16: 128-140.
- Clen Mayhall C (2005) Hospital Epidemiology and Infection Control. (3rd edn), Lippincott Williams & Wilkins.
- TÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂávora AC, Castro AB, MilitÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂão MA, GirÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂão JE, Ribeiro Kde C, et al. (2008) Risk factors for nosocomial infection in a Brazilian neonatal intensive care unit. Braz J Infect Dis 12: 75-79.
- Heath J, Zerr DM (2006) Infectious Diseases of the Fetus and Newborn Infant: Infection Acquired in the Nursery: Epidemiology and Control. (6th edn), WB Saunders Company. Philadelphia.
- Gill AW, Keil AD, Jones C, Aydon L, Biggs S (2011) Tracking neonatal nosocomial infection: the continuous quality improvement cycle. J Hosp Infect 78: 20-25.
- Decembrino L, Perrini S, Stronati M (2010) [Surveillance of infection events in neonatal intensive care]. Minerva Pediatr 62: 41-45.
- Schwaber MJ, Lev B, Israeli A, Solter E, Smollan G, et al. (2011) Containment of a country-wide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Israel Carbapenem-Resistant Enterobacteriaceae Working Group. Clin Infect Dis 52: 848-855.
- Van der Zwet WC, Kaiser AM, Van Elburg RM, Berkhof J, Fetter WP, et al. (2005) Nosocomial infections in a Dutch neonatal intensive care unit: surveillance study with definitions for infection specifically adapted for neonates. J Hosp Infect 61: 300-311.
- Goldmann DA (1989) Prevention and management of neonatal infections. Infect Dis Clin North Am 3: 779-813.
- National Nosocomial Infections Surveillance System (2004) National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 32: 470-485.
- Cheung GY, Otto M (2010) Understanding the significance of Staphylococcus epidermidis bacteremia in babies and children. Curr Opin Infect Dis 23: 208-216.
- Lachassinne E, Letamendia-Richard E, Gaudelus J (2004) [Epidemiology of nosocomial infections in neonates]. Arch Pediatr 11: 229-233.
- Brito DV, von Dolinger EJ, Abdallah VO, Darini AL, Gontijo Filho PP (2009) Two outbreaks of mixed etiology associated with central venous catheters inserted by phlebotomy in critical neonates. Braz J Infect Dis 13: 177-182.
- Arslan U, Erayman I, Kirdar S, Yuksekkaya S, Cimen O, et al. (2010) Serratia marcescens sepsis outbreak in a neonatal intensive care unit. Pediatr Int 52: 208-212.
- Rasigade JP, Laurent F, Lina G, Meugnier H, Bes M, et al. (2010) Global distribution and evolution of Panton-Valentine leukocidin-positive methicillin-susceptible Staphylococcus aureus, 1981-2007. J Infect Dis. 201: 1589-1597.
- Tzialla C, Borghesi A, Perotti GF, Garofoli F, Manzoni P, et al. (2012) Use and misuse of antibiotics in the neonatal intensive care unit. J Matern Fetal Neonatal Med 25 Suppl 4: 35-37.
- Maltezou HC, Tryfinopoulou K, Katerelos P, Ftika L, Pappa O, et al. (2012) Consecutive Serratia marcescens multiclone outbreaks in a neonatal intensive care unit. Am J Infect Control 40: 637-642.
- Arnoni MV, Berezin EN, Martino MD (2007) Risk factors for nosocomial bloodstream infection caused by multidrug resistant gram-negative bacilli in pediatrics. Braz J Infect Dis 11: 267-271.
- Schulman J, Stricof R, Stevens PT, Horgan M, Gase K, et al. (2011) Statewide NICU Central-Line-Associated Bloodstream Infection Rates Decline After Bundles and Checklists. Pediatrics 127: 436-444.
- Maltezou HC, Kontopidou F, Katerelos P, Daikos G, Roilides E, et al. (2013) Infections caused by carbapenem-resistant Gram-negative pathogens in hospitalized children. Pediatr Infect Dis J 32: e151-154.
- WHO (2006) Managing Newborn Problems: a guide for doctors, nurse and midwives.
- Bilali A. Bartsocas C. Velonakis E (2012) Necrotizing enterocolitis and premature infants. Arch Hellen Med 29: 290-310.
- Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, et al. (2011) Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol 32: 101-114.
- Foca M, Jakob K, Whittier S, Della Latta P, Factor S, et al. (2000) Endemic Pseudomonas aeruginosa infection in a neonatal intensive care unit. N Engl J Med 343: 695-700.
- Souli M, Galani I, Antoniadou A, Papadomichelakis E, Poulakou G, et al. (2010) An outbreak of infection due to beta-Lactamase Klebsiella pneumoniae Carbapenemase 2-producing K. pneumoniae in a Greek University Hospital: molecular characterization, epidemiology, and outcomes. Clin Infect Dis 50: 364-373.
- Daikos GL, Markogiannakis A (2011) Carbapenemase-producing Klebsiella pneumoniae: (when) might we still consider treating with carbapenems? Clin Microbiol Infect 17: 1135-1141.
- Sydnor ER, Perl TM (2011) Hospital epidemiology and infection control in acute-care settings. Clin Microbiol Rev 24: 141-173.
- Polilli E, Parruti G, Fazii P, D'Antonio D, Palmieri D, et al. (2011) Rapidly controlled outbreak of Serratia marcescens infection/colonisations in a neonatal intensive care unit. Euro Surveill 16: 1-3.
- Couto RC, Pedrosa TM, Tofani Cde P, Pedroso ER (2006) Risk factors for nosocomial infection in a neonatal intensive care unit. Infect Control Hosp Epidemiol 27: 571-575.
- Garland JS, Uhing MR (2009) Strategies to prevent bacterial and fungal infection in the neonatal intensive care unit. Clin Perinatol 36: 1-13.