Keywords
Mental health reform- Community mental health services-Satisfaction
Introduction
During recent years, there has been a focus on deinstitutionalisation of mentally ill patients including reduction of hospital-based long stay towards community-based mental health services [1,2].
Indeed, significant efforts have been made in many European countries to move from a mental health system dominated by institutional care towards to community mental health services [1,2]. However, all countries have not successfully implemented the community based mental health services as the procedure demands major changes in service structures, additional investments in services, increase of staff and strong commitment of many agencies [3,4].
De-institutionalization, as an aspect of psychiatric reform has a diachronic character [5,6]. Community based mental health services are considered as ‘a long term challenge’ that moreover demand improvement of quality of care [1,2] “Psychosocial re-establishment offers the opportunity to mentally ill patients to attain a more independent living in community. Interestingly, prerequisite for this transition is that patients are at their best possible level of functioning, thus, allowing their smoothly integration in society [1,2,4].
Over the last 20 years, Greece has been modernizing an outdated mental health system which was previously based on institutional care. More in detail, psychiatric reform in Greece mainly includes the deinstitutionalization of chronic psychiatric hospital patients and the development of a wide range of community mental health services. Various forms of community-based mental health services have been developed including supported living facilities, community mental health centres and employment opportunities [1,2].
In this frame belong the establishment of psychiatric departments within general hospitals, Boarding houses and Guest houses. Boarding houses are community residential places accommodating up to 25 patients with 24 hours high staff support. Guest houses accommodate up to 15 chronic mentally ill patients or with psychosocial problems with 24 hours staff support [1,2].
Indeed, after the reform effort that started in the mid 1980s, including de-institutionalization and establishment of numerous community services, Greek psychiatry has been in a transitional period. Psychiatric reform needs continuation including re-orientation of the national mental health strategy towards more realistic and priority-orientated goals and guaranteeing adequate and continuous flow of resources to support the patients moving in community [5,6].
Satisfaction of mentally ill patients by community based mental health services is the ultimate goal within the frame of the psychiatric reform not only in our country but also globally [1,2].
The aim of the present study was to compare satisfaction of mentally ill patients moving from hospital to community based settings (Guest houses, Boarding houses) to their previous hospital stay.
Method and Material
The sample studied included 200 mentally -ill patients moving from a public psychiatric hospital to community-based settings : a) Guest Houses, b) Boarding Houses.
Data were collected by the completion of a specially designed questionnaire for the needs of the present research. This tool consists of 74 variables, of which 20 concerning socio-demographic and clinical characteristics. Of the remaining 54 variables, which are the dependent variables, the first 12 (A1 - A12), evaluate the satisfaction by personal hygiene, the next 10 (B1 - B10) the satisfaction by nutrition of the mentally ill, the next 10 variables (C1 - C10) satisfaction relating to safety, followed by 12 questions (D1 - D12), which explore the satisfaction of the mentally ill referred to sociability. Here are five variables (E1 - E5) exploring satisfaction with opportunities for education and professional rehabilitation and finally five variables (Z1 - Z5) exploring satisfaction of the mentally ill by the financial. Evaluation of the internal consistency of the questionnaire was carried out by calculating the Cronbach Alpha coefficient that was 0,89.
The method for the data collection was interview and completion of this specially modified questionnaire, which it fully met the requirements of the current study. All patients who met the inclusion criteria of the study had been hospitalized in the psychiatric hospital and had a good knowledge / use of the Greek language. Patients were excluded if they had a primary diagnosis of mental retardation or a dementing illness.
This particular patient sample was a convenience sample.
Statistical analysis was carried out using SPSS-16 and statistical method were t-test and Anova.
The study was approved by the Medical Research Ethics Committee of each hospital and was conducted in accordance to the World Medical Association’s Declaration of Helsinki (1989).
RESULTS
Descriptive Results
Of the 200 patients who participated in the research, 109 was men (54,5%) and 91 women (45,5%). 40,5% lived in Guest Houses and 59,5% in Boarding houses. Of the sample-studied, 4% was 20-29 years old, 9% was 30-39 years old, 26% was 40-49 years old and 61,5% was older than 50. In regard to marital status, 16% was married, 64% was single and 19% was divorced or widowed. 22% had children. Regarding educational status, 18% was uneducated, 33% was of primary education, 37% of secondary education and only 12% was of higher/university education. According to the occupational status, 14% was unemployed, 7% public servants, 48% private employees, 19% free- lancers and 12% was occupied in domestic duties. 67% of the sample studied, had relatives in the wide area of Athens, 10% in province, 9% in a village, 10% both in the wide area of Athens and 3% abroad. Of the 200 patients studied, 32% was 20-29 years old at the onset of mental illness, 17% was younger than 20 years old, 23% was 30-39 years old and 28% was older than 40. As regards the years that patients lived in the psychiatric hospital, 24% was less than 6 months, 20% was over than 20 years, 5% was less than a year, 15% was 1-2 years, 10% was 3-5 years, 10% was 6-10 years and 16% was 10-20 years. According to the years that patients moved to community-based settings, 10% lived there less than 1 year, 27% lived 1-2 years, 19% lived 3-5 years, 36% lived 6-10 years, 7% 11-20 years and only 1% lived there over than 20 years. 22% of the participants, reported another member in their family suffering from mental illness, of whom in 7% was the father, in 29% was the mother, 11% was siblings, 19% was the sister, 4% was the one parent and the siblings, in 5% was both parents and siblings, in 5% was the grandfather, in 5% was only the siblings and in 5% was both parents.
Regarding the frequency of relatives and friends’ visits, 21% reported that had no visitors, 22% that seldom had visits, 31% often and 26% very often, while regarding communication through telephone, 20% reported that they had no calls from relatives and friends, 14% seldom, 25% often and 41% very often.
14% of patients reported co-existence of other health problem. More in detail, 8% had diabetes, 1,5% had cancer, 1% had hepatitis, 3% had a cardiovascular disease and 1% had pneumonopathy.
As regards re-admission to the psychiatric hospital, in 7% of participants was necessary to return to hospital more than 2 times, 3% only 2 times, 6% 1 time and 84% had no need to return to the hospital.
24% of participants met their personal expenses by a pension as a protected member of family, 24% by personal pension, 37% by a subsidy, whereas in a percentage of 15% personal expenses were met by family or personal income.
95% reported satisfied by the hygiene and 80% by nutrition.
Regarding quality of food, 66,5% of participants reported that it was the same to hospital one.
According to the sense of safety, more than 75% felt more safe in community-based settings than in hospital. Furthermore, 80% of patients reported that they had more opportunities to be socialized than in the hospital.
Of the 200 patients only a percentage of 1-2% considered that they had the same or less opportunities in educational and professional re-establishment in community than in hospital.
Statistical Results
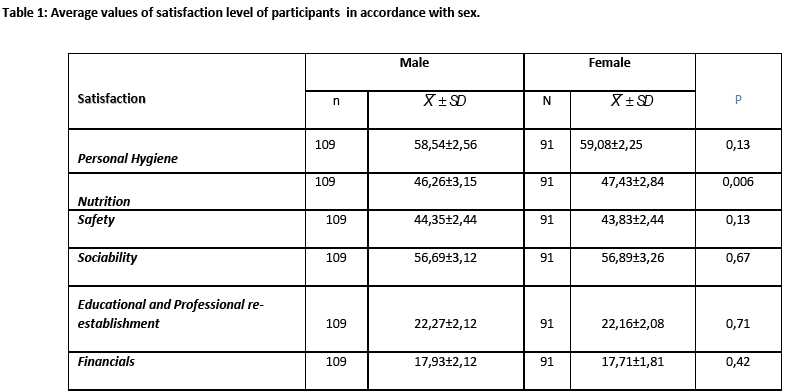
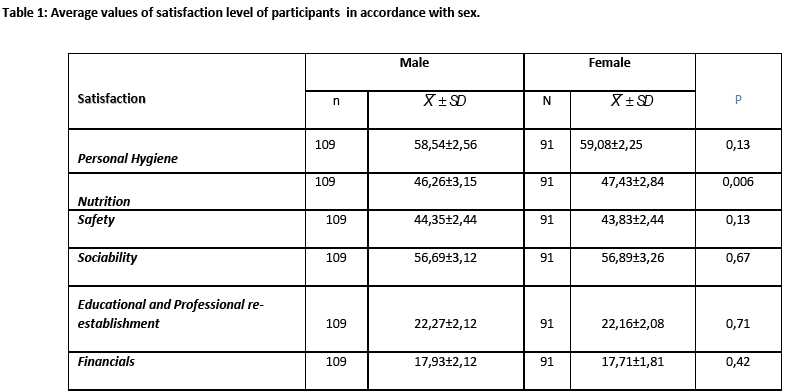
The statistical analysis showed that women were more satisfied by nutrition in community with statistically significant difference compared to men, p=0,006, whereas, there was no statistically significant difference related to personal hygiene p=0,132, to sense of safety p=0,134, to sociability p=0,672, to the opportunities of educational and professional re-establishment p=0,712 and financially p=0,407. (Table 1)
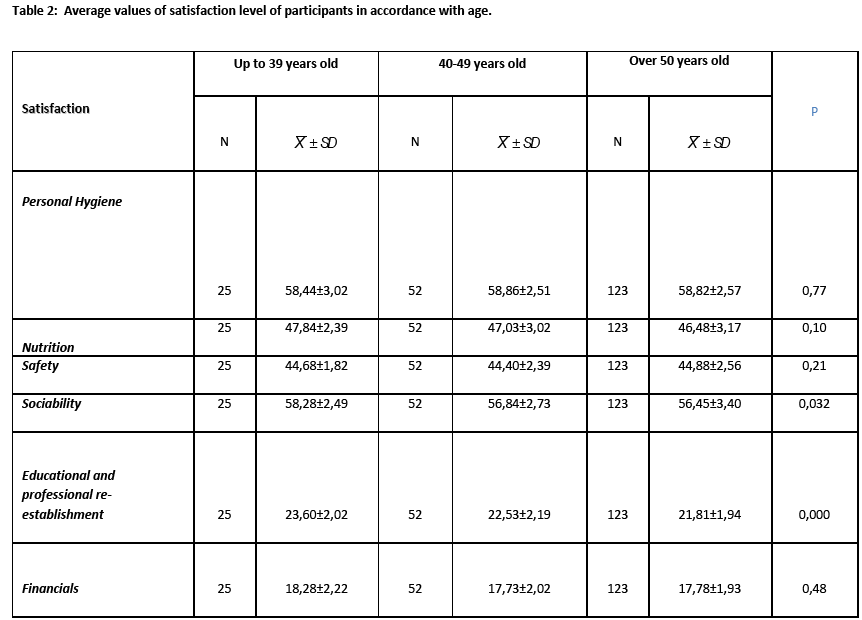
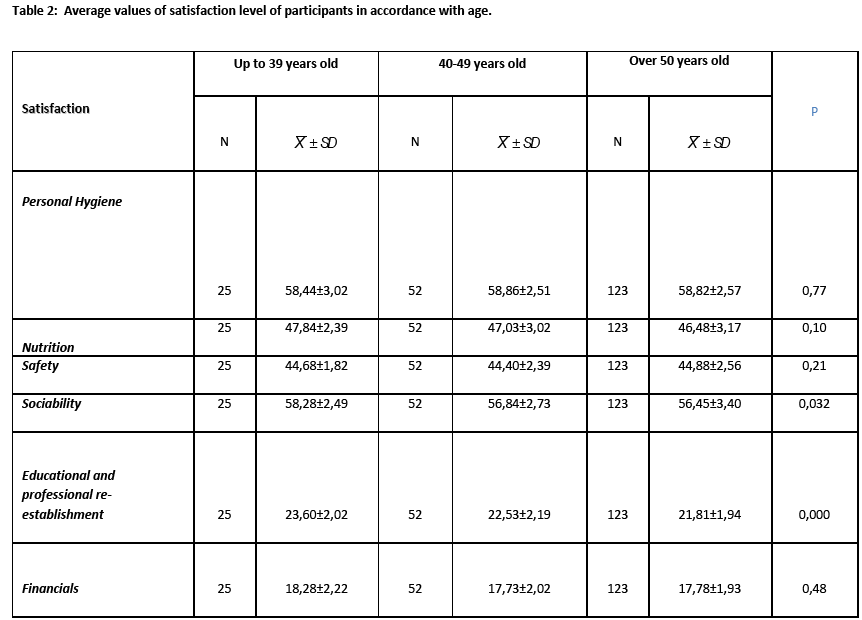
According to the age, the group age of 30-39 years old, it was found to be more satisfied by opportunities for educational and professional re-establishment but also more satisfied financially, p=<0,01 and p=0,009, respectively. (Table 2)
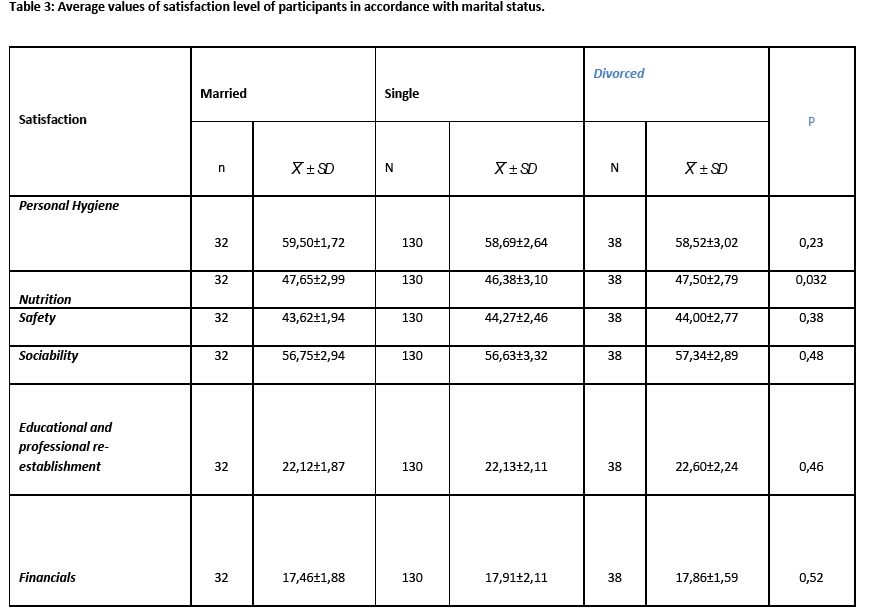
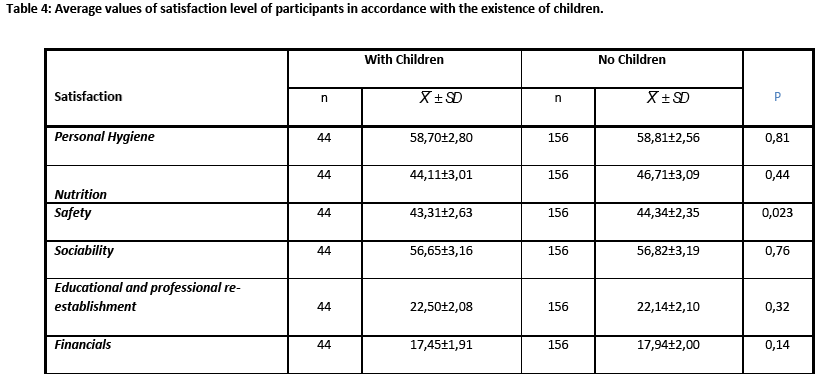
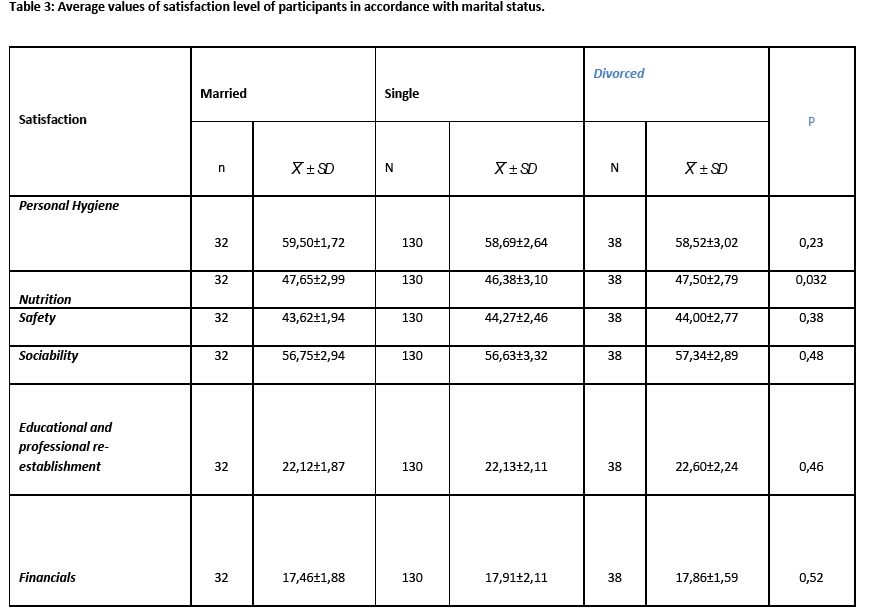
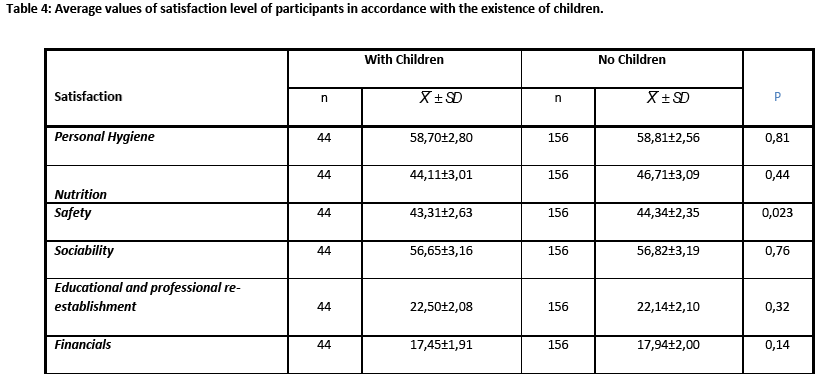
As far as the marital status is concerned, it was found that married individuals were more satisfied by their nutrition, p=0,032. Furthermore, it was found that patients with no children felt more safe, p=0,023. (Table 3 and 4)
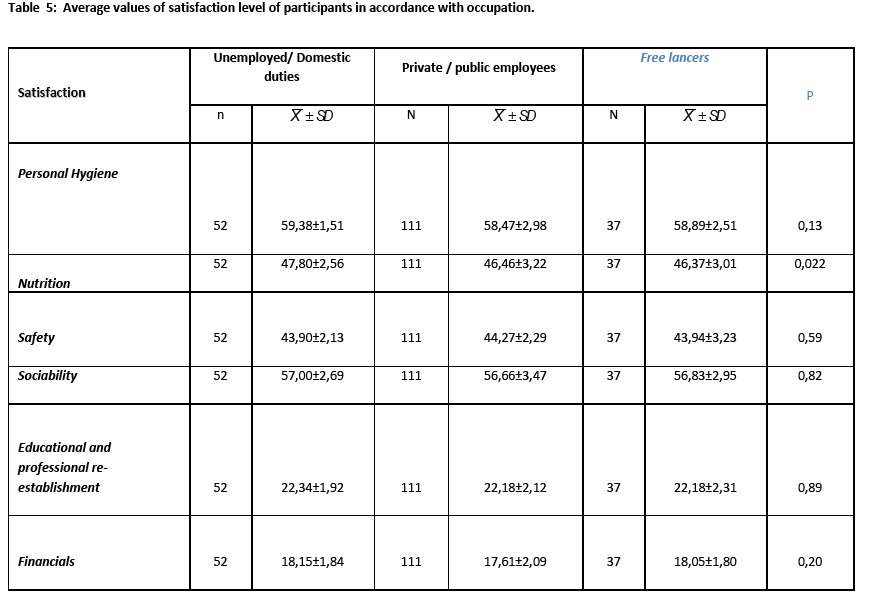
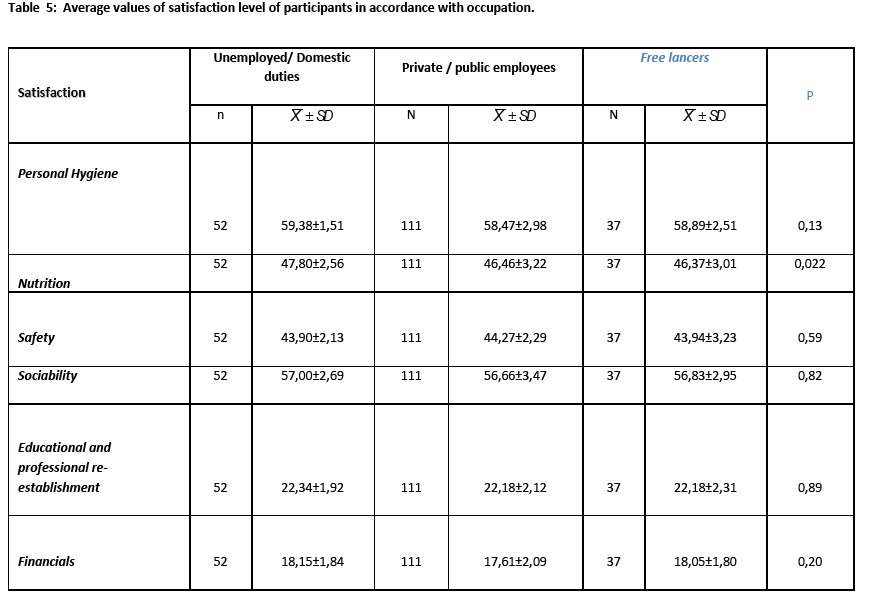
In regard to marital status, the unemployed and those of domestic duties were more satisfied by nutrition, p=0,022. (Table 5)
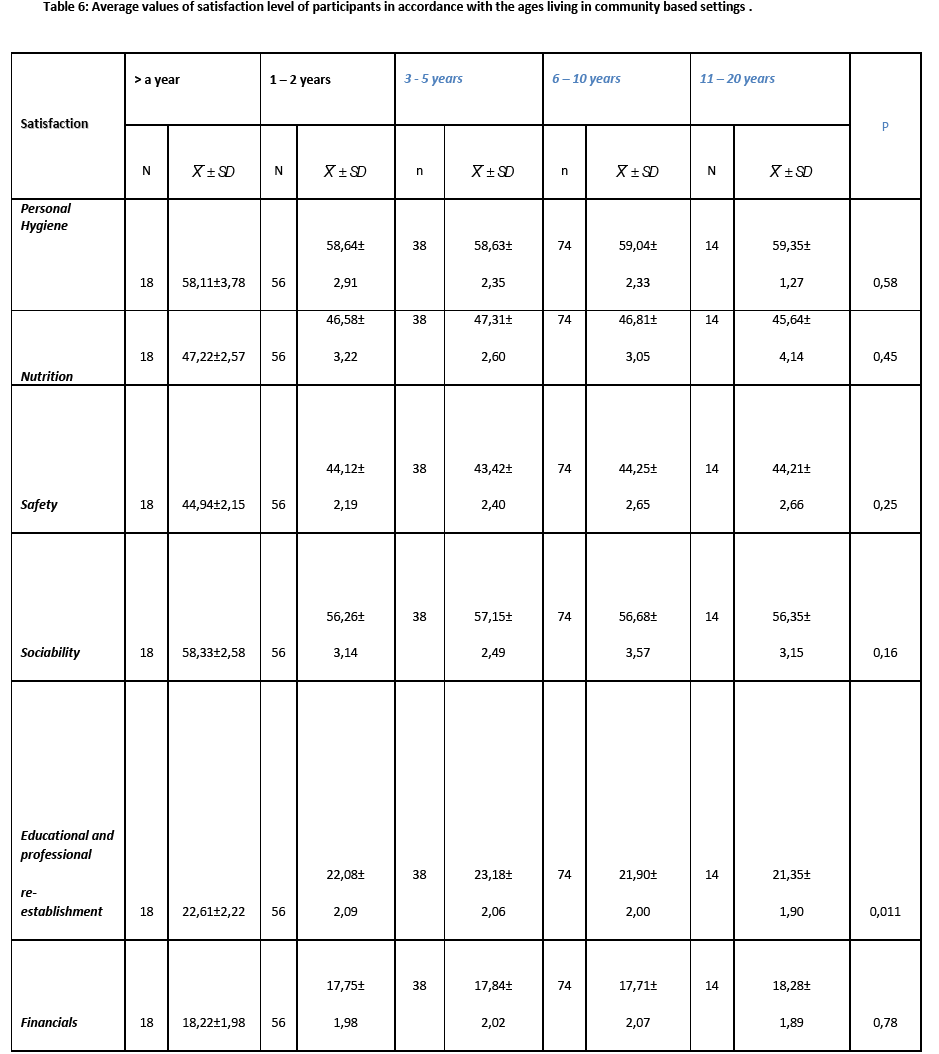
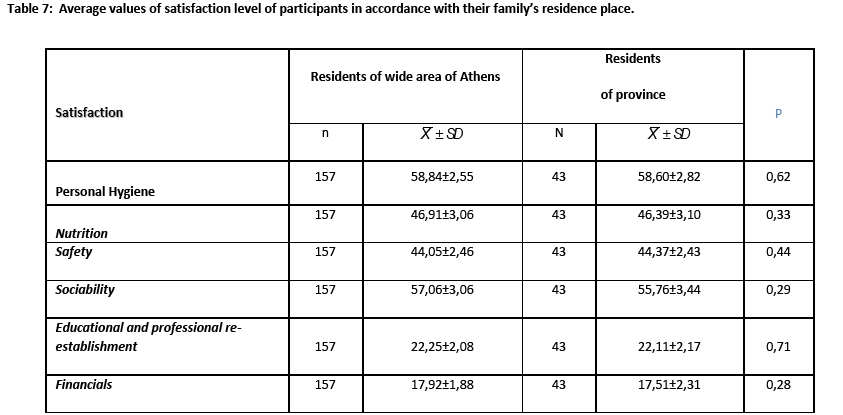
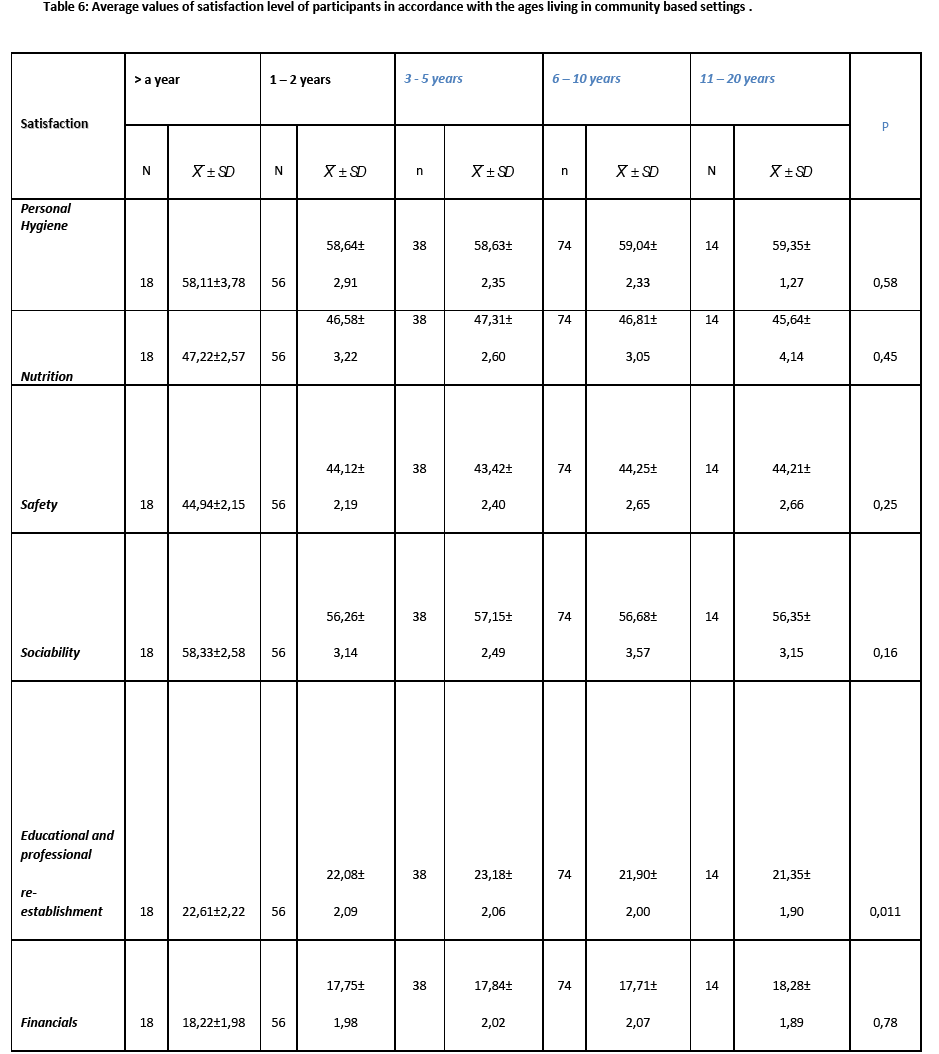
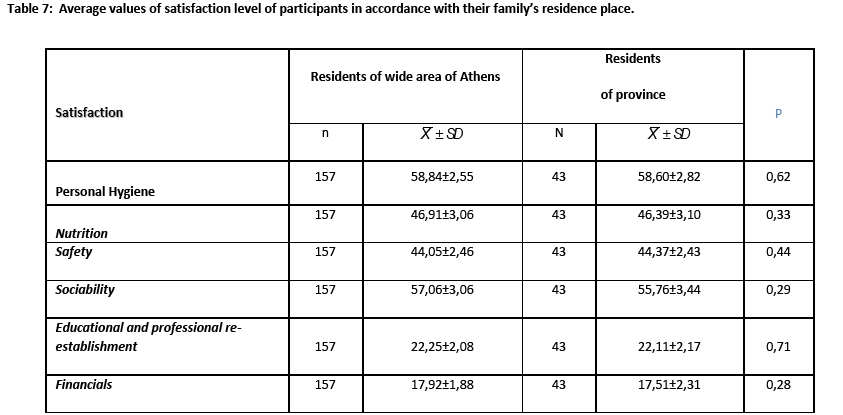
More socialized were patients who lived 3-5 years in community-based settings and those whose family lived in the wide area of Athens, p=0,011 and p=0,029, respectively. (Tables 6 and 7)
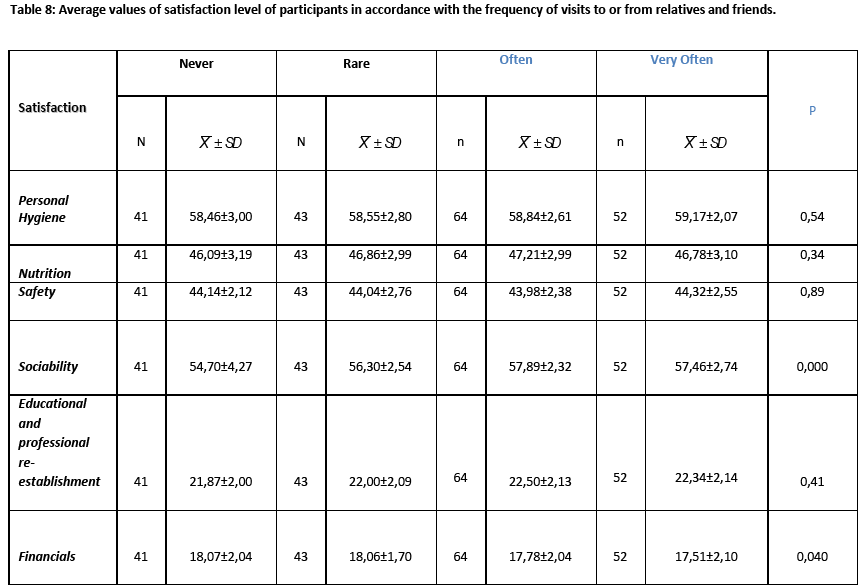
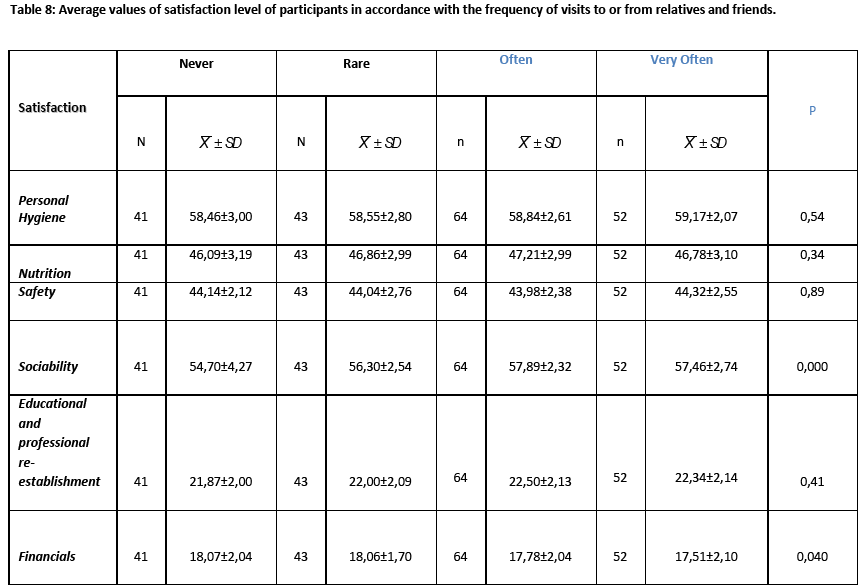
More satisfied by their sociability, were those visited often by relatives and friends and those satisfied by their finances, p=<0,001 and p=0,004 respectively. (Table 8)
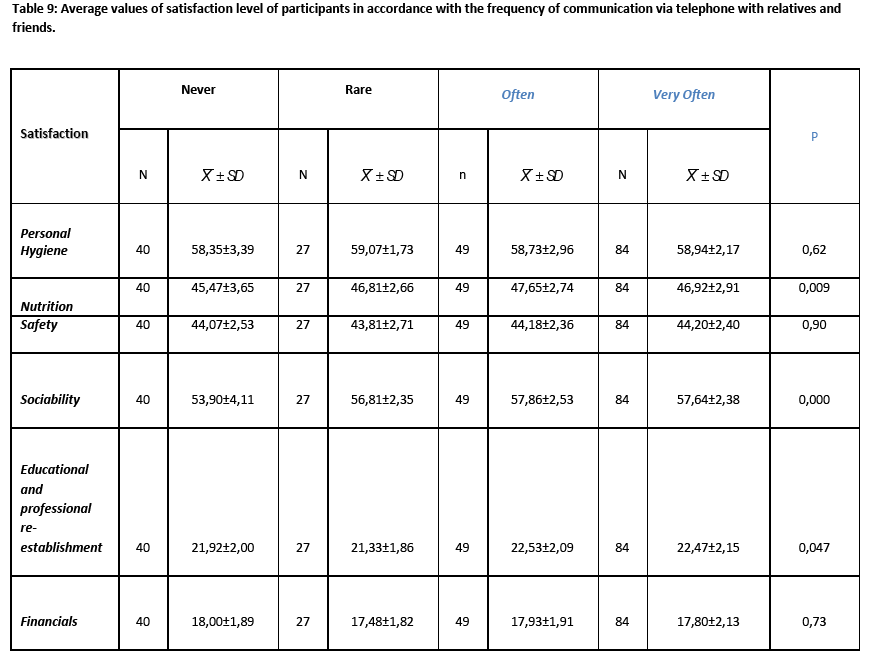
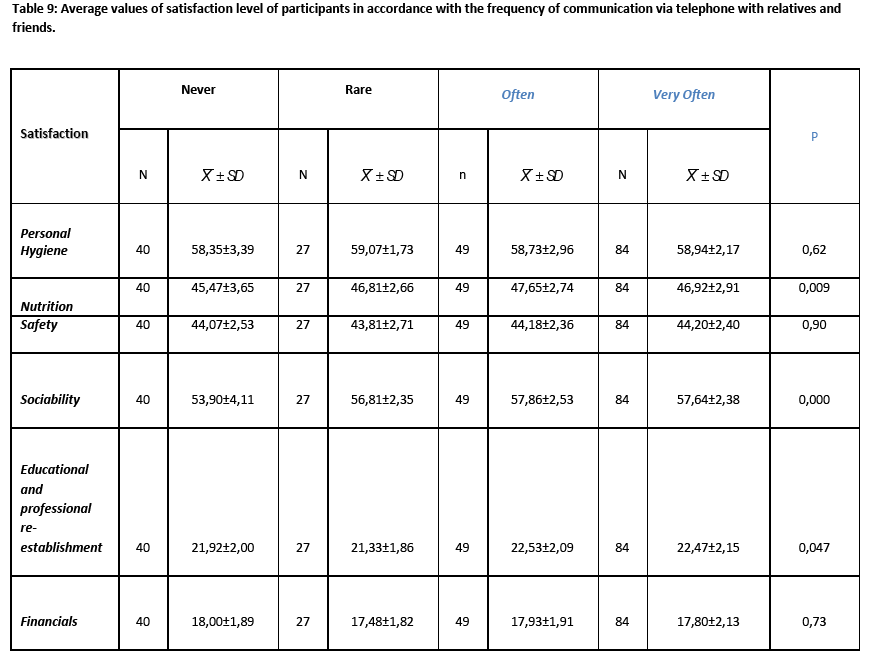
Patients who communicate often with relatives and friends by the phone were more satisfied by their nutrition p=0,009, by sociability p=<0,001, by the opportunities of educational and professional re-establishment p=0,047 and by their finances, p=0,001. (Table 9)
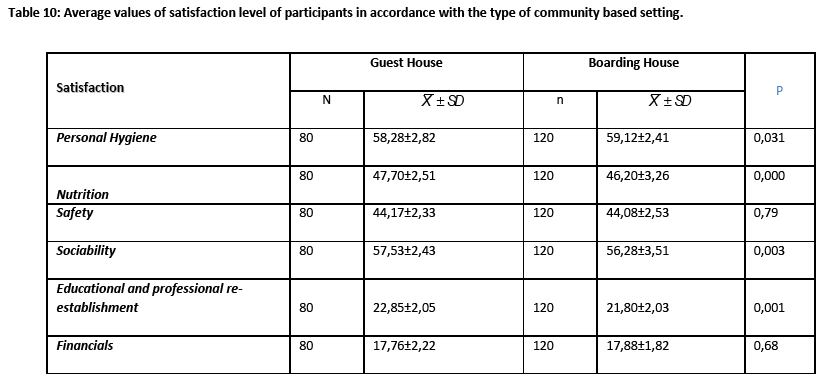
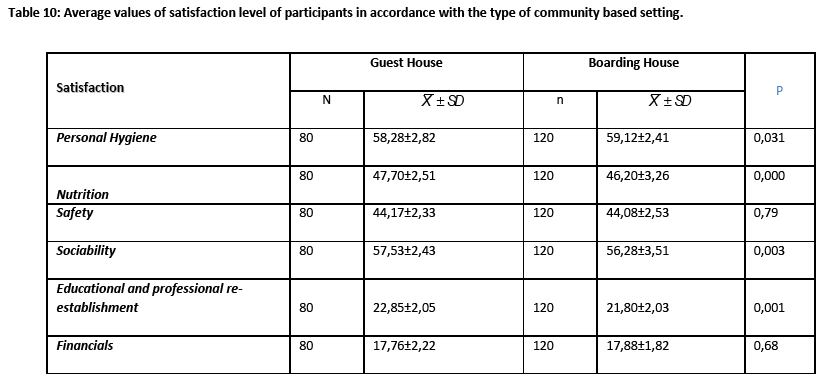
Those living in Boarding houses were more satisfied by their personal hygiene, p=0,031, whereas, those living in Guest Houses were more satisfied by their nutrition, p=<0,001, their communication and sociability, p=0,003, the opportunities of educational and professional re-establishment, p=0,001 and the finances, p=0,019. (Table 10)
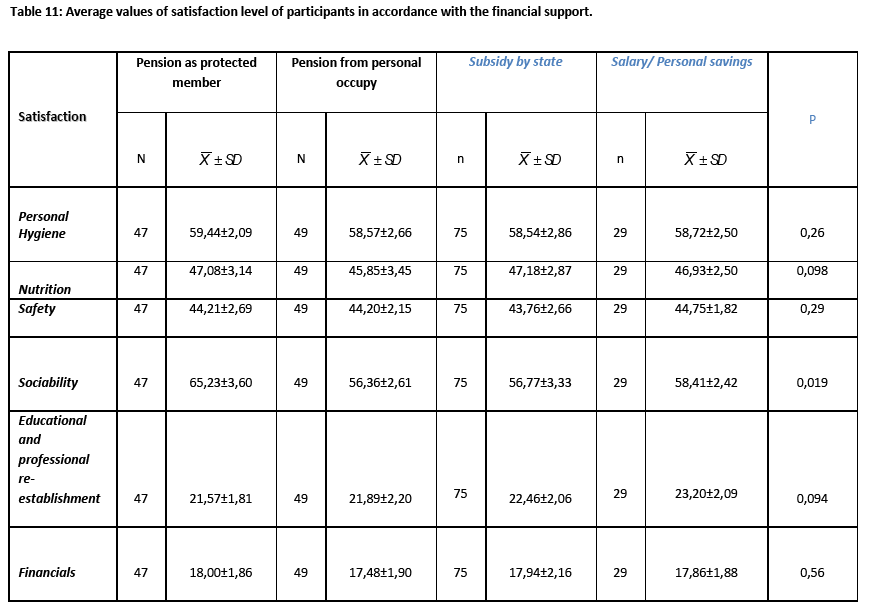
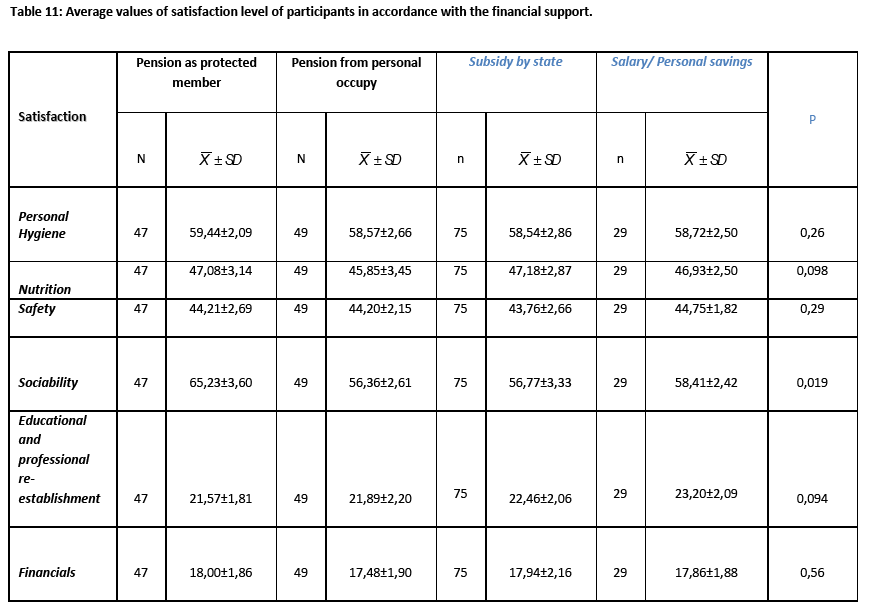
As far as the satisfaction by sociability is concerned, more satisfied were those who had salary or their family supported them financially, p=0,019 and those who believed they had more opportunities in education, p=0,094. (Table 11)
Discussion
From the studied population the 54,5% were men and the 45,5% women of age above 40 years at a percentage of 87,5%.
The present study showed that 84,5% of the moving patients from hospital to community-based settings did not need to return to the Psychiatric Hospital. This finding is mainly attributed to early screening and treatment of relapse of the disease. This may also be attributed to patients' deeper belief that is better to live as independent individual which has a beneficial effect on the prognosis of psychiatric disorders. Finally, this finding possibly reflects a more personalized approach to mental health intervention including individual’s functioning as a whole.
The results of the present study are congruent in with those by Ercole et al., [7] who found that only 4,4% of patients needed re-admission for psychiatric help in the hospital. The same researchers also supported that effective outpatient and community services offer another option for meeting patients' needs and resolving the crises thus reducing rehospitalization rates. Lin et al., [8] suggested that readmission occurring very close to the time of discharge is strongly related to the quality of care delivered in hospitals whereas readmission that occurs at a time distant from hospital discharge can be influenced by aftercare and psychiatric services provided in both community and outpatient settings. The same authors also showed that 6,1% of psychiatric patients were readmitted within 14 days after discharge and the number increased to 37,8% as the period of the study extended to five years. Irmiter et al., [9] showed that homelessness, medical morbidity and substance use were associated with increased risks for reinstitutionalization. Bonsack et al., [10] showed that deinstitutionalisation and more respect of patients' rights were considered as positive changes for most patients, but as a risk for the most vulnerable ones. Thornicroft et al., [11] indicated that 86% of patients moving from hospital to community-based settings reported that they would recommend their new home to others. Possibly, long-term patients discharged within a planned program prefer their new community homes to the hospital. This change of attitude is mainly attributed to the environmental quality of the community community-based settings which offer greater choice and autonomy in terms of everyday activities.
The vast majority of participants reported that their health problem can be equally faced as in the hospital. Probably, patients feel more safe because having not lost their independence, they maintain control on their personal live. Furthermore, in psychiatric hospitals are often admitted patients with violent behavior or crisis, thus resulting to the adoption of the same behavior by the other patients. Such behaviors do not often take place in community-based settings where a more safe living environment is prevalent. Last but not least, the secure and supportive close relationship with the nurses in community based help services enhance rehabilitation and prevent relapses and recurrences of the disease. It is worth noting that recognizing patients' needs entails personal involvement which help the professional to achieve a deeper understanding of the individual. According to Eriksen et al., [12] in a busy general medical ward it is impossible to monitor patients’ behavior up to a detailed extend which makes their management difficult and can result in an escalation of the behavior.
Individuals of 30-39 years were more satisfied by their living in community compared to older ages. Younger individuals, reported more satisfied by nutrition, sociability, professional re-establishment and education due to the fact that they have more social and family support, more possibilities in education and professional re-establishment.
According to Stelling et al., [13] young people suffering from mental illness are trying to integrate their illness into daily life. Consequently, their needs are different from the elder patients. Usually, young individuals have the advantage to receive a great deal of attention by health professionals regarding education and professional re-establishment, despite difficulties, such as the stigma of mental illness. On the other hand, Evans-Lacko et al., [14] showed that unemployment rates in mentally ill patients have increased concluding that at contemporary times of economic crisis individuals with mental health problems experience social exclusion, especially males and those with lower education. The same researchers also claimed that interventions to combat economic exclusion of mentally ill patients as well as to promote their social integration are even more important during times of economic crisis.
From the statistical analysis it was also found, that participants who had no children felt more safe in community-based settings. Possibly, being deprived of the family support they consider their current living environment as a family that provides them safety.
More satisfied reported those who had contacts with relatives and friends often and very often or even communicate with their family by the phone. The present finding illustrates the importance of social and family support that exerts a beneficial effect on the prognosis of the disease. Given the importance of family, it is understandable why they should be more systematically and extensively involved in the therapeutic regimen.
It is worth noting that Chiappelli et al., [15] showed that patients' satisfaction by Community Mental Health Service differs according to their demographic and clinical features. More in detail, in young patients with serious mental disease high frequency of visits seemed to correlate with low satisfaction and t relative's involvement is judged as insufficiently effective.
It is important to incorporate family to care of mentally ill patients by increasing their knowledge and widening their coping abilities. Enhancing awareness among members of family about the disease would benefit mentally ill patients. It would be an essential step if the supportive environment could help patients without imposing a further emotional burden upon them with feelings of insecurity and rejection [16-18]. According to Brady et al., [19] family responses to having a member with mental illness include: care burden, fear and embarrassment about illness symptoms, uncertainty about the outcome of the disease, lack of social support and stigma. Information provided to family by mental health empower their involvement to the therapeutic regimen.
The results of the present study also showed that patents living in community-based settings were more satisfied by the quality of their hygiene. Health professional provide holistic care, meting all patients' needs including individual hygiene. Another possible explanation is that in community-based settings, patients' care is more individualised, a fact that strengthens the effort of patient for personal improvement.
Those having an income or personal financial resources provided by their relatives are more satisfied socially and they have more chances for professional re-establishment and education. In terms of deinstitutionalization, financial resources help the individual to cover the personal needs and take better advantages of the opportunities offered.
Traditionally, therapeutic intervention of mentally ill patients has been focused on the absence or reduction of symptoms of mental illness. However, available effective treatments do not necessarily address a holistic approach. In some cases it might even further impair a person’s ability to function in everyday life. Intervention focus on a personalized approach where individual characteristics, (biological, cultural, socioeconomic) are considered is expected to optimize outcomes, to provide substantial opportunity for the reduction of disability, regain good social functioning and minimize mental illness-related mortality. Moreover, patient preference is a powerful indicator of the level of adherence to treatment. Mental health interventions should meet patients' needs taking also into account cultural and ethnic factors [20].
Conclusions
The results of present research, showed that the quality of life and more in detail, whatever concerns the nutrition, the individual hygiene, the sociability, the sense of safety, the educational and professional re-establishment in the community, as reported by the patients, is much better in community compared to Psychiatric Hospital.
The role of health professionals and specifically the nurses should be focused on the promotion of health of mental patients, on the elimination of negative sentiments and the improvement of self esteem having as ultimate goal smooth integration in community.
2809
References
- Loukidou E, Mastroyiannakis A, Power T, Craig T, Thornicroft G, Bouras N. Evaluation of Greek psychiatric reforms: methodological issues International Journal of Mental Health Systems. 2013, 7:11.
- Loukidou E, Mastroyiannakis A, Power T, Craig T, Thornicroft G, Bouras N. Greek mental health reform: Views and perceptions of professionals and service users. Psychiatrike. 2013;24(1):37-44.
- Muijen M. Local Excellence and National Strategy: Bridging the Gap. Psychiatr Serv. 2011;62(12):1405.
- Antai - Otong D. Psychosocial rehabilitation. Nurse Clin. North. AM. 2003;38:151-160.
- Christodoulou GN, Ploumpidis DN, Christodoulou NG, Anagnostopoulos DC. The state of psychiatry in Greece. Int Rev Psychiatry. 2012;24(4):3016.
- Christodoulou G. Psychiatric reform revisited World Psychiatry.2009;8(2):121?122.
- D' Ercole A, Struening E, Curtis J. Effects of Diagnosis, Demographic Characteristics, and Case Management on Re-hospitalization. Psychiatric Services. 1997;48(5):682-688.
- Lin CH, Chen WL, Lin CM, Lee MD, Ko MC, Li CY. Predictors of psychiatric readmissions in the short- and long-term: a population-based study in Taiwan. Clinics (Sao Paulo). 2010;65(5):481-9.
- Irmiter C, McCarthy JF, Barry KL, Soliman S, Blow FC Reinstitutionalization following psychiatric discharge among VA patients with serious mental illness: a national longitudinal study. Psychiatr Q. 2007;78(4):279-86.
- Bonsack C, Schaffter M, Singy P, Charbon Y, Eggimann A, Guex P. Qualitative study of a social and health network's expectations for community treatment of severe mental health problems. Encephale. 2007;33(5):751-61.
- Thornicroft G, Bebbington P, Leff J. Outcomes for long-term patients one year after discharge from a psychiatric hospital. Psychiatr Serv. 2005;56(11):1416-22.
- Eriksen K?, Sundf?r B, Karlsson B, R?holm MB, Arman M. Recognition as a valued human being: perspectives of mental health service users. Nurs Ethics. 2012;19(3):357-68.
- Stelling K, Kuhn K, Riedel-Heller SG, Jungbauer J. Developmental problems in young adults suffering from mental illness: results from an in-depth interview study. Psychiatr Prax. 2009;36(3):119-24.
- Evans-Lacko S, Knapp M, McCrone P, Thornicroft G, Mojtabai R. The mental health consequences of the recession: economic hardship and employment of people with mental health problems in 27 European countries. PLoS One. 2013;8(7):e69792.
- Chiappelli M, Berardi S. Pattern of intervention and patients' satisfaction with community mental health services in Bologna. Epidemiol Psichiatr Soc. 2000;9(4):272-81.
- Pack S. Empowering families to care for people with schizophrenia. Nurs Times. 2005;101(30):32-4.
- Caqueo-Ur?zar A, Guti?rrez-Maldonado J. Satisfaction with mental health services in a Latin American community of carers of patients with schizophrenia. Community Ment Health J. 2009;45(4):285-9.
- Klam J, McLay M, Grabke D. Personal empowerment program: addressing health concerns in people with schizophrenia. Psychosoc Nurs Ment Health Serv. 2006;44(8):20-8.
- Brady N, McCain GC. Living with schizophrenia: a family perspective.Online J Issues Nurs. 2004;10(1):7.
- Web site : The National Institute of Mental Health Strategic Plan. https://www.nimh.nih.gov/about/strategic-planning reports/index.shtml. Accessed on : 17-7-2012.