Historical Overview & Future Implications
The COVID-19 pandemic has brought to light, for perhaps the first time since the Spanish Flu just over 100 years ago, the danger cities face during an outbreak of disease. The dystopian landscape of a city in quarantine, where those few out of their houses shuffle about carefully in their masks and the urban white noise is instead just the wail of an ambulance, is a far cry from the environment city dwellers have come to love and expect. This dark reality will pass but the uniquely dangerous threat of disease a city faces will not. Due to their very nature, cities and their inhabitants are more at-risk for disease, the threat of disease spread decreases the interest and attractiveness of city dwelling, and disease in cities leads to quarantine, decreasing the livelihood, wellbeing, and quality of life for city dwellers [1-7]. This poses a serious threat to the long-term sustainability, resiliency, and health of cities and their inhabitants. There is arguably no more direct path towards the United Nations Sustainable Development Goal 11 to “make cities and human settlements inclusive, safe, resilient and sustainable” [8] than confronting this catastrophic threat. Therefore, it is critical to build sustainable, resilient, and healthy cities by 2030 through the prevention of and reduction in spread of disease.
Sustainable Development Goal 11 seeks to make cities and human settlements inclusive, safe, resilient and sustainable. The priorities by the United Nations have thus far been focused on slum reduction, availability of public transportation, growth management, improvement in waste collection, healthier air, and open space [8]. While these topics are pivotal to the sustainability of cities and tie in to public health, efforts to curb down disease spread can enormously contribute to sustainable cities [9-23]. Reducing disease in urban environments is critical for health of the general population. For one, cities are the general population as most people globally live in urban areas; currently over 5 billion people and projected to be at 7 billion people by 2050 [24]. City dwellers account for roughly 55% of the world population in 2020, and this is projected to be closer to 66% by 2030. Thus, statistically speaking, healthier cities will result in a healthier general populations.
Sustainable Development Goal 8 focuses on promoting sustained, inclusive and sustainable economic growth, full and productive employment and decent work for all. As the world is currently seeing during the COVID-19 pandemic, contagious disease and pandemics are very harmful to economies, both macro and micro; “Pandemics can cause economic damage through multiple channels, including short-term fiscal shocks and longer-term negative shocks to economic growth” [23]. In the short term, the immediate public health response tactics towards pandemics are quarantine and travel bans. Quarantine leads to dramatic job loss and unemployment. In March-April of 2020, at the height of the COVID-19 pandemic, the number of unemployment claims in the United States alone reached 22 million — the highest mark since the Great Depression and roughly the net number of jobs created in a nine-and-a-half-year stretch that began after the last recession and ended with the pandemic’s arrival [20]. Unlike financial industry recessions, such as 2008, which particularly targets assets and those with assets, the pandemic recession has been devastating for working class and blue collar jobs which require physical human-to-human contact, such as the service, food, travel, construction, transportation, and retail industries. Even those who remain employed, but whose organizations are undergoing financial hardships, are likely to experience furloughs and reduced wages.
In the long-term financial picture, pandemics lead to panic though perceived risk. In this sense, a perceived threat can often have a bigger economic impact than the virus itself. As COVID-19 continues to dominate headlines, it is easy for individuals to convince themselves that the threat to their life is serious and immediate, typically contributing to a chain reaction of panic over social media or word of mouth. While not necessarily untrue, this potentially distorts the actual risk and leads to a panic towards the future. This panic towards the future has incredibly negative effects on the economy, particularly investments and futures; “Put simply, social media hastens the spread of panic and misinformation around a virus, causing the global economy to hemorrhage money – according to Markets Insider, the S&P 500 lost 11 percent of its value over five days at the end of February, [when panic was setting in] its worst weekly drop since the 2008 financial crisis” [20]. Another example, when Peru disclosed an outbreak of cholera in 1991, its South American neighbors imposed bans on Peruvian food products. The subsequent $700 million loss in exports ultimately exceeded the health and productivity costs of the actual epidemic [20,25-28]. It would be repetitive and common sense, but needless to say dramatic economic repercussions caused by pandemics would in its own right have an impact on nearly all of the other Sustainable Development Goals in one way or another; loss of housing, food insecurity, cities overburdened reduce public systems, closed schools lead to lessened education, resource scarcity leads to international hostility, etc.
Background
First and foremost, cities are highly at-risk for disease because they are both crammed and connected. The concentration of people living in cities (density) makes urban populations more susceptible to person-to-person spread of disease [2,9,15]. In fact, increasing population density has an exponential correlation to increase in disease spread; “As density approaches 4x [the standard deviation of average density], the disease spreads rapidly, affects a large proportion of the at-risk population, and will result in an epidemic close to 98% of the time” [29]. Further, cities are commonly home to two extremes in high density housing. One, highly populated low-income urban housing, or slums, result in high density areas coupled with poor basic infrastructure and a lack of sanitation. From a public health perspective, these are the two largest threats to the spread of disease [2,26]. The United Nations predicts that over one billion people globally live in these slums, accounting for 23% of the world’s urban population. The other housing extreme which contributes to population density is high-priced real estate, where expensive housing forces residents to room together to afford housing, leading to higher density and tighter living spaces [9]. This danger of density is nothing new, as history has shown again and again the dangerous pairing of cities and disease. From the plague of Athens in 430 B.C and the Plague of Justinian in Constantinople 1,000 years later, to 1600’s London where there was a six-year life-expectancy loss by living in London relative to the rest of England, to then 1900, when nearly half of all deaths in America’s major cities were still caused by infectious illnesses [5,9]. Even now his pattern continues, as COVID-19 epicenters develop in major cities on opposite sides of the world, including Wuhan and New York City.
Which leads to the next trait of cities which make them particularly susceptible to disease, their connection to each other. With advancing technology in transportation and an increasingly globalized international market, globalized travel has never been easier. It’s now merely hours between the time hundreds or thousands of travelers are from one end of the earth to the other. Cities serve as this port of entry, as they are home to the airports, seaports, train stations, and highways which serve as the veins of transportation. This also makes cities the ports of entry for new disease, “whether it’s the rats carrying the fleas or a traveler from Wuhan carrying the virus” [5]. From the cities, it is practically instantaneous for that disease to travel with commuters, tourists, or on surfaces from those cities into the suburbs and eventually the countryside. Whereas countries, or certainly regions, used to be innately isolated and easily locked down, now the globe has become one communal petri dish.
The other connection point that leaves cities particularly vulnerable to the spread, and conception, of disease is their increasing proximity to nature. As the boundaries between cities and nature shrink and altogether disappear, the risk of trans-species infections becomes immediately apparent; “Rapid urbanization enables the spread of infectious disease, with peripheral sites being particularly susceptible to disease vectors like mosquitoes or ticks and diseases that jump the animal-to-human species boundary” [12]. Coupled with urbanization, agricultural intensification and deforestation are also “part of the land-use change variable that has significantly correlated with emerging infectious diseases" [10]. It is not just these perimeter areas that pose a high risk for trans-species infections, as animal markets and disease-laden rodents and insects are also unique risk factors for cities. A string of recent pandemics can all be traced back in some way to the connectivity between cities and animals: Severe Acute Respiratory Syndrome, avian influenza, Nipah virus, Hendra virus, Ebola, Marburg fever, Lassa fever, Zika, and now COVID-19 [7].
The inherent density and connectivity of cities makes them not just particularly at risk for disease, but also other threats. For example, density makes city dwellers more vulnerable to not just novel disease, but terrorist attacks, crime, pollution, invasions of privacy, traffic accidents, and natural disasters [21]. This goes against the priorities of city planners in modern history, who have encouraged density as a sustainable solution while prioritizing development of high-density housing and public transportation. Thus, cities have become and will continue to become denser and therefore more susceptible to threats; “Rethinking density management is a key for long-term survival in a pandemic world” [14].
Without the knowledge of the inherent risks, inhabitants of cities are automatically at higher risk of disease for the reasons previously explained, and thereby cities will see the impact on public health and mortality rates. This alone will affect the urban experience. Further, as cities respond to disease with reactive measures such as quarantine and social distancing, there will be higher unemployment and homelessness, more remote work, less need for and interest in public transportation, less large gatherings, and less socialization overall. All of these are core components of city living and decrease the livelihood, wellbeing, and quality of life for city dwellers. Cities are, by definition, the “absence of physical space between people… Their success depends on the face-to-face contact now perilous to health. Contagion turns the logic of cities on its head. If you’re close enough to share an idea, you’re close enough to spread a contagious disease” [3].
Global health systems strengthening
The current global pandemic is an example of survival of the fittest. The cities that are emerging resilient have secured commitment of local leaders and strengthening public health networks to prevent, detect, and respond to disease threats early. This approach strengthens the capacity for stakeholders within city governments to build strong preparedness systems that are better adapted to increasingly urbanized settings. In Epidemic preparedness in urban settings: new challenges and opportunities, Lee et al. [17] suggest that strengthening the capacities of urban centers enables stakeholders to be proactive when it comes to dealing with the sociocultural shifts that their residents may be experiencing.
Global pandemics such as COVID-19 present cities with a myriad of challenges and opportunities. Lee et al. [17] explore the interplay that exists among the following factors: population density and public transportation, population heterogeneity, and the dissemination of information. Metropolitan governments are grappling with the multidimensional makeup of the cities that they govern. These cities are not only heavily congested but may have exceeded their population carrying capacity resulting in poor housing environments that hinder outbreak prevention measures. To make matters worse, the public transportation systems of these large urban areas make it arduous to trace contacts that might have been exposed to the virus.
In some countries, low-income groups as well as ethnic minorities are disproportionately affected by COVID-19. Lee et al [17] note that there are “a wide range of cultural factors, including modes of social interactions and acceptable control measures; some subpopulations might be difficult to reach” (p. 527). Therefore, an increase in the amount of testing kits does not necessarily translate to an equitable distribution to certain demographics in a city. For example, in the United States, African-American and Hispanic American communities have been hard hit by the epidemic. They are not only recording a faster rate of infection but are also dying at alarming rates - recent statistics show that the 28% and 34% of all deaths in New York City have been black and Hispanic people respectively [18].
Conversely, indigenous groups in Taiwan have been spared from high rates of infection. This is because of the uniform population dispersion that characterizes Taiwan. The nine indigenous tribes are quite heterogeneous among one another due to long-term isolation that has persisted since Taiwan became an island about 12,000 years ago. As a result, Taiwan is not susceptible to the overcrowded settlements that other nations are grappling with. Taiwan’s heterogeneous subpopulation also had to be under scrutiny. The influx of Chinese residents in Taiwan also led to the use of unconventional means of communication. For example, persons with low risk (no travel to level 3 alert areas) were sent a health declaration border pass via SMS (short message service) messaging to their phones for faster immigration clearance; those with higher risk (recent travel to level 3 alert areas) were quarantined at home and tracked through their mobile phone to ensure that they remained at home during the incubation period [30].
How is Singapore responding COVID-19?
Singapore - like many other countries- has a world class health system that delivers the best possible care to its citizens. Unlike the health systems of other countries that have been overstretched, Singapore has actually been prepared for a pandemic of this magnitude for some time now. In 2003, a task force was created for the purposes of coordinating government’s messages to citizens during pandemics. The task force operates as a decentralized agency and is able to facilitate coordination between different government arms. The first reported cases of COVID in Singapore involved the Ministry of Health working in conjunction with the police force to trace individuals who might have been exposed [11]. The task force serves as the middleman between the Ministry of Health’s objectives and the Singaporean sense of civic duty - whereby the well-being of society takes precedence over an individual’s comfort. The rule of law during a public health crisis is paramount to sustaining short-term gains that a metropolitan has made. These short-term gains - when sustained effectively - have the power to accelerate the timeline in which the pandemic ends. In an effort to understand the population breakdown of who has the most need, Singaporean officials standardized the hospital intake process by providing public health preparedness clinics with the ability to identify and triage the highest risk patients such as patients with respiratory symptoms. Moreover, at-risk patients were also provided government-subsidized treatments which alleviated the costs associated with seeking care.
How is Taiwan responding to COVID-19?
Taiwan leverages the power of its communication networks as a tool for disseminating information to its citizens. Travelers who have not traveled to level 3 countries or higher receive SMS messages which notify them of where to go for a declaration border pass. The mere nature of not having to wait in queues reduces their likelihood of being exposed to the virus from someone who might be coming from a highly prevalent area. Moreover, the national health insurance database is highly utilized to generate big data for analytics based on travel history and clinical symptoms of individuals to aid case identification. The national health insurance database functions as a repertory for identifying patients who are at a higher risk of contracting the virus. Through the national health insurance database, Taiwanese officials have found a way to seek out patients who have severe respiratory symptoms. Patients who have previously tested negative for influenza are then retested for COVID-19. According to recent statistics, 1 out of 113 cases in that sample have also tested positive for the coronavirus.
Curbing the spread of the coronavirus also entails strict monitoring of people in order to ensure that they practice social distancing. The Taiwanese government used “technologies such as cell phone applications in tracking user data body-heat sensors to determine contacts and monitor body temperatures” [19]. These mobile phone applications also enforce quarantines by being able to alert officials of any movement of newly discovered COVID patients as well as who their close contacts are. As a result, the government is not only aware of an individual’s bill of health but is also positioned to intervene [30]. Taiwan’s ongoing success in suppressing SARS-CoV-2 has also led to member states of the World Health Organization calling for her return to the World Health Organization [6]. Similar to Singapore, the cost of care does not pose a financial burden to patients. Following the lessons learnt from the severe acute respiratory syndrome (SARS) epidemic in 2003, Taiwan took measures to ensure that its national health insurance scheme has a 99% coverage rate [30].
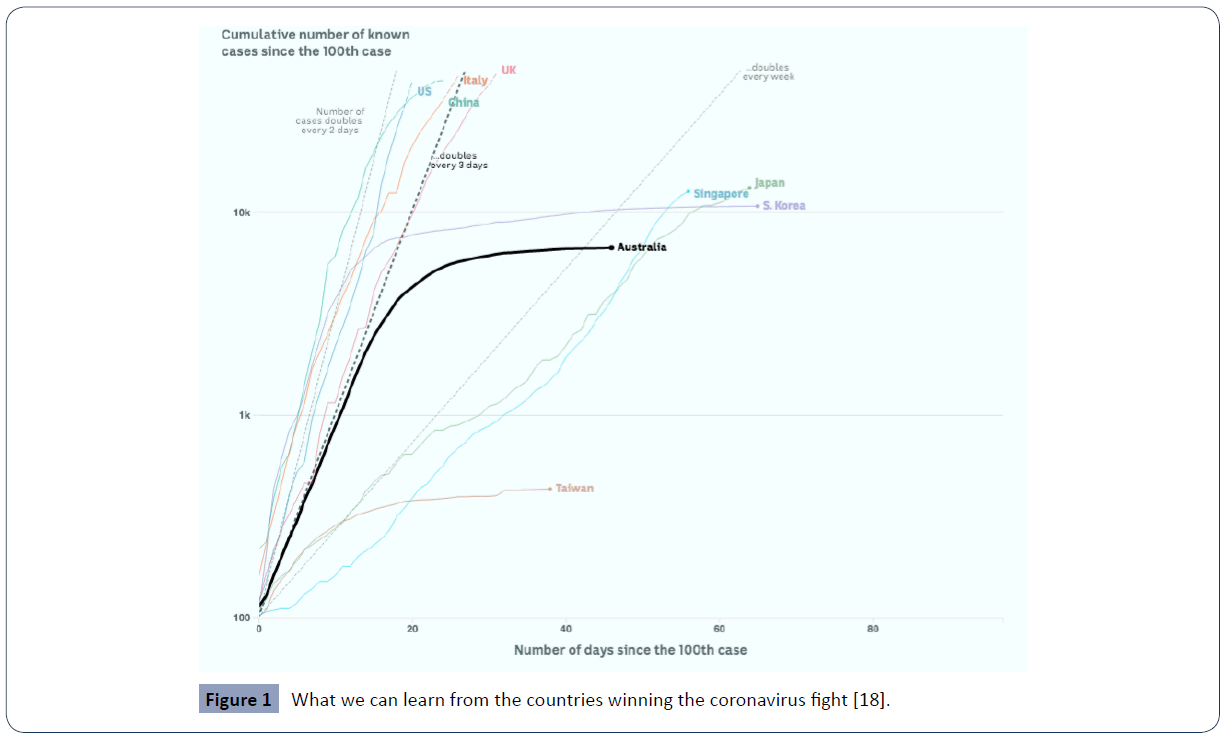
Singapore and Taiwan provide a strong case for the role that public health governance plays during public health crisis. Lee et al. [17] note that the COVID-19 pandemic presents an opportunity for leaders in cities to be better positioned to “develop and implement effective and contextually appropriate solutions” (p. 527). Leaders in cities such as Pulau Ujong (Singapore’s capital) or Taipei (Taiwan’s capital) are reaping off the benefits of greater investments in their respective local systems (Figure 1).
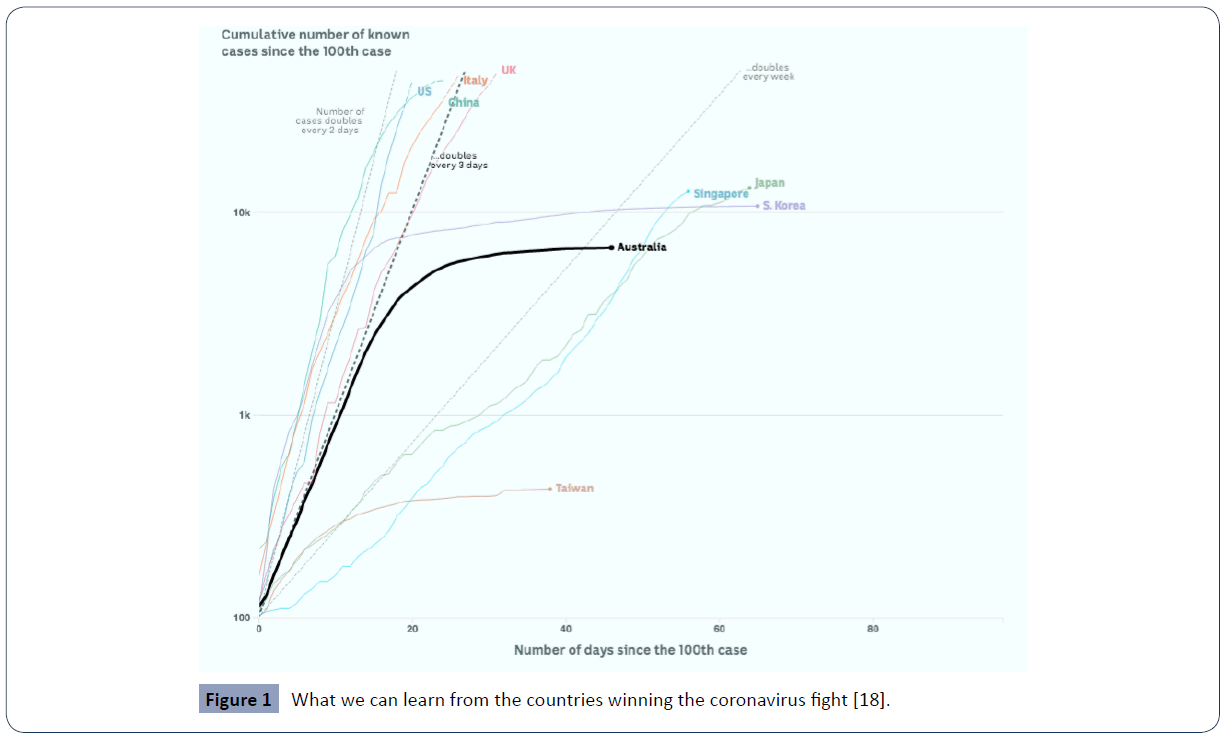
Figure 1 What we can learn from the countries winning the coronavirus fight [18].
How is Nigeria responding to COVID-19?
Following the arrival of a Nigerian expatriate, the first COVID-19 case in Nigeria was reported on February 28 in Lagos, the country’s most populous city. Like many countries, the virus began to spread to other parts of the nation. This led to the government being in a state of frenzy and calling for a nationwide lockdown on March 30. In addition, the Coalition against COVID-19 was formed as a private sector response towards tackling the epidemic. This coalition also serves as a philanthropic vehicle for providing marginalized and vulnerable communities with the necessary relief materials that they need during this lockdown. Despite the ongoing national lockdown, Nigeria recorded a significant spike in the number of active COVID-19 cases. Specifically, Kano (a predominantly Muslim state) has emerged as the new epicenter with 90 new cases everyday - which is higher. One of the reasons why the number of cases in Nigeria has increased is because of the fact that, the public health advisories being issued to the public are not being followed. People are finding ways to still move from one state to another amid the lockdown. As a result, the purpose of having a lockdown whereby interstate travel is barred is defeated by people's decision to disobey the law and travel between cities.
Poor decisions being made by individuals exacerbates the likelihood for others to stand a fighting chance against the virus. In Nigeria, there are social inequalities that make it arduous for healthy behavior practices. According to the United Nations, there are 69 million Nigerians do not have access to clean water [1]. Similarly, 90% of Nigerians do not wash their hands properly which increases their risk of infection [22]. Therefore, communities that are poverty stricken are at a significant disadvantage when it comes to fighting the coronavirus. Most Nigerians have small to medium size enterprises and as a result, the need to go to their places of work is paramount to their daily wellbeing. Therefore, the notion of social distancing is one that might work great in theory but does resonate well in practice. As expected, people have also publicly expressed that they stand a higher chance dying from hunger than from the virus. That said, they would rather risk their chances of being outside their homes than being told to endure more weeks of lockdown. As of May 3, 2020, the Nigerian Centre for Disease Control (NCDC) reveals that there are 2,558 confirmed cases of COVID-19 in Nigeria and 87 deaths. Unfortunately, there is a shortage of isolation spaces in the country and the need for people to adhere to public health messages is more needed now than ever while government exercises effective leadership.
Future Preparation for Pandemics – What can we do differently?
Often society finds itself criticizing or questioning the actions of leadership in situations where outcomes are either unclear or misunderstood. In the case of pandemics, we as a modern society have dealt with several varying instances, each with different approaches to solving the issues but also, each with somewhat similar outcomes. The solution to our current pandemic has been argued with a variety of approaches and should be analyzed appropriately from every angle. With both health and economic stakes as high as they are, it is important to understand past response successes and failures. Moreover, it is crucial that we analyze the current data to better dictate what measures a society should undertake when faced with similar catastrophes in the first place.
The more recent pandemic has exposed the three critical challenges in a public response: viral differentiation, healthcare costs, and critical action analysis. Firstly, the viral differences between influenzas are slight enough to avoid clinical preparation as it stands today. The aforementioned reason for having multiple influenza pandemics is just as described. However, none of them are exactly the same. Secondly as far as healthcare is concerned, there are two sides to the conversation. Public access to healthcare should be a foundational aspect of any societal system where, in parts of the world, these systems are implemented. In the US for instance, many would make a fair argument that the vast majority of pharmaceutical innovation is achieved to solve these public health problems, but generally at the cost of unaffordable healthcare for many Americans. Lastly, there is contradictory data on public response to the economic shutdown. While the general consensus suggests a response favoring the shutdown of most socially interactive activities, the question to what extent should these measures be enacted remains open.
The public health’s common response [25] to pandemic control follows a fairly similar roadmap from both a geographic and historical standpoint:
1. Government Public Health Systems will limit social contact in an effort to lessen transmission from infected to those who lack immunity
2. Vaccines are developed to match the said virus
3. Public Vaccination Occurs
4. Drugs are developed to create viral antibodies
The challenge here is clearly timing, regardless of public access or cost to the vaccination. Both the literature as well as consensus opinion point to the fact that in reality, societies will only ever be able to physically respond to pandemics in a systematic way. “A well-planned, effectively communicated and coordinated emergency response that draws on medical mobilization is the key to a successful strategy for pandemic preparedness and response and will minimize the health threat of future pandemic influenzas [16].
To lockdown or not to lockdown? With the economic impact on a micro and macro level as significant as it’s proven to be, how can leaders make well-informed decisions in preparation of potential disasters? Analysis has been done to determine the optimal equilibrium in terms of economic and public health repercussions. Interestingly, a study that was conducted to analyze the effects of closing & no-closing scenarios for the 1918 Flu Pandemic for a population the size of New Zealand suggests interesting socioeconomic results.
Comparing the statistical validity of both closing and no-closing tactics, the general economic costs were looked at in terms of both import and export impacts as well as the implied cost of healthcare, both of which effect the net bottom-line impact of the pandemic. The data suggests that a 12-week closure with a 26 week ‘return to normal’ timeframe netted a savings of NZ$11 Billion as opposed to no closure with a base case scenario assuming modern medicine could handle the demands of the pandemic. Further, and even more clearly, the second case scenario showed an even more substantial cost savings in closure of NZ$120 Billion where the pandemic was assumed to hold a 10x mortality rate [4].
From an import/export standpoint, the data suggests a closure of the border to not be strong an economic decision for the mild scenario ie ~12,400 deaths but does hold a significant positive impact (even when assuming 100% losses) when the pandemic reached the 10x mortality rate ie ~124,000 deaths [4]. To put these numbers in perspective, New Zealand typically sees ~500 seasonal flu deaths per year [13] suggesting that the mild flu scenario described earlier would be 25x worse than the average flu season and in the severe scenario, 248x worse. Comparing it to today’s response, the US has seen its worst flu mortality rate in the winter of 2017 with ~80,000 deaths and more conservatively, averages roughly ~12,000 – 61,000 deaths annually (CDC Statistics). While the two economic structures are not similar, we can reach to make a comparison in saying the US has not yet come close to what the literature has described as the ‘mild’ scenario, in which case the infected population would have reached a threshold of 625,000 deaths (assuming an annual death rate of 25,000).
As a benchmark to actionable items, Taiwan has made a significant effort to track performance for pandemic preparation measures through both H1N1 and the SARS pandemics in 2003 and 2009. The general tactical strategies for hospital administration and communication were built on six-sigma principals. Additionally, a tactic known as “control bundling” was developed through both pandemic responses and refined as a means to directing and dispersing patients on local levels through the testing and treatment phases. Class suspensions for children and government mandated social distancing additionally played a significant role in the improvements from a disease control standpoint [16].
The data and literature suggests a combination of short term social distancing, perhaps a brief border closing for non-trade-related travel, and a clearly prepared local infrastructure for both disease management and communication. The analysis has a collective mixture of local response that is implicated by the global interaction. Therefore, the argument can be made at both a global and local scale considering we generally understand that predicting pandemics is challenging. Global collaborative response efforts in terms of travel restrictions and border controls could be a mutually beneficial way to create a global synergy response, and on the local level where these outbreaks may first occur, a structures infrastructure at the hospital level should be prioritized.
How can modern societies look to use our connective leverage in our favor? While the expansion of the globalized economy may prove to open doors for potential issues regarding the fundamental transfer of disease, our advancements in digital connectivity actually offer a unique benefit in times of crisis. Some organizations are utilizing the sheer volume of user-generated content as a means to predict and forecast potential behaviors if it can be materialized in an efficient way. One study was done specifically looking at the social media platform Twitter, where data was streamed and collected to track the public sentiment during both the H1N1 Swine Flu outbreaks as a means to measure the disease activity [28-30].
The data on social media platforms is free and in real time and can easily be tracked on a large scale by imply searching for and understanding topic trends. Furthermore, this information can focus on cities or entire continents simultaneously. Because the information is tracked ‘live,’ health experts are able to react in real time and prepare on a near-term basis. The data shows that at a local level, the real time data produced is fairly effective in understanding current data trends that are typically determined by healthcare professions 1-2 weeks after the fact. While this method certainly has its flaws, it is an example of how the connected world offers new opportunities to inherently build firewalls for potential issues in a much quicker and more efficient manner.
As a global society, the growing data in conjunction with demands for stronger local response mechanisms, provide the opportunity to take both past and present information to make a strong argument for recommended steps. Reviewing the literature points to the blind spot in the challenge of determining pandemic threat levels, which would be timing. The challenge in understanding which threats pose true dangers are a tough call. While the data suggests the advantages of shutting down borders, doing so at a bad time holds significant cost. The big picture should be to hold collective and standardized global accountability in terms of closure and travel policy, while at the local level, creating specific hospital infrastructure and management systems to control the flow of infection. Social distancing and short-term shutdowns have also proven effective and should continue to remain a cornerstone in the response strategy. Finally, utilizing new forms of social data to better understand patterns and better predict disease status in real time has shown an upside in terms of response timing where applicable.
36937
References
- Adebowale N (2018) 69 million Nigerians lack access to safe water- UNICEF. Premium times.
- Berg N (2016) As cities grow more crammed and connected, how will we discourage the spread of disease? Ensia.
- Bermingham F (2014) Edward Glaeser: Successful Cities Depend on Density of Smart People. International Business Times.
- Boyd M, Baker MG, Mansoor OD, Kvizhinadze G, Wilson N (2017) Protecting an island nation from extreme pandemic threats: Proof-of-concept around border closure as an intervention. Plos One 12.
- Dubner SJ, Hickey M, Chen D, Douglas RL (2020) What Does Covid-19 Mean for Cities (and Marriages)? Freakonomics.
- Dziedzic S (2020) Taiwan rejoining World Health Organization still backed by Australia in diplomatically risky move. ABC News.
- Florida R (2020) Pandemics have destroyed cities before. Could they do it again? Fastcompany.
- Hendrix M, Manhattan Institute (2020) Density and Disease. Eye on the News.
- Hilsenrath J (2020) Global Viral Outbreaks Like Coronavirus, Once Rare, Will Become More Common.
- Hsu LY, Tan MH (2020) What Singapore can teach the U.S. about responding to Covid-19. Statnews.
- Keil R, Connolly C, Ali SH (2020) Outbreaks like coronavirus start in and spread from the edges of cities. The conversation.
- Kessaram T, Stanley J, Baker MG (2014) Estimating influenza-associated mortality in New Zealand from 1990 to 2008. Influenza and Other Respiratory Viruses 9: 14–19.
- Klaus I (2020) Pandemics Are Also an Urban Planning Problem. Bloomberg CityLab.
- Kraemer MUG, Perkins TA, Cummings DAT, Zakar R, Hay SI, et al. (2015) Big city, small world: density, contact rates, and transmission of dengue across Pakistan. The Royal Society Publishing.
- Associated Press (2018) CDC: 80,000 people died of flu last winter in the U.S. highest death toll in 40 years.
- Lee VJ, Ho M, Kai CW, Aguilera X, Heymann D, et al (2020) Epidemic preparedness in urban settings: new challenges and opportunities. The Lancet Infectious Diseases 20: 527-529.
- Leslie T, Gourlay C, Byrd J, Hanrahan C, Elvery S, et al. (2020). What we can learn from the countries winning the coronavirus fight. ABC News.
- Maizland L, Felter C (2020) Comparing Six Health-Care Systems in a Pandemic. Council on Foreign Relations.
- Nelson (2020) Nowhere to Hide' as Unemployment Permeates the Economy.
- Ovuorie T (2014) 90 percent Nigerians don’t wash hands properly, risk infection - Research.
- Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora ME, ( 2015) Mental, Neurological, and Substance Use Disorders. Disease Control Priorities (3rd edn) volume 4. Washington, DC: World Bank.
- Robbins A, Freeman P (2018) Completing the global strategy: a missing element in preparation for pandemic influenza. Journal of Public Health Policy 39: 265–267.
- Sciences N. A. of, Engineering, & Medicine (2018) Understanding Infectious Disease Transmission in Urban Built Environments.
- Scott D (2020) 4 lessons the US should learn from Italy’s coronavirus mistakes.
- Signorini A, Segre AM, Polgreen PM (2011) The Use of Twitter to Track Levels of Disease Activity and Public Concern in the U.S. during the Influenza A H1N1 Pandemic. PLoS ONE 6.
- Tarwater PM, Martin CF (2001) Effects of population density on the spread of disease. Complexity 6: 29–36.
- Wang CJ, Ng CY, Brook RH (2020) Response to COVID-19 in Taiwan. JAMA 323: 1341.