Key words
ICU acquired weakness, muscle strength, functional ability
Introduction
Intensive care unit acquired weakness (ICUAW) is one of the most frequent complications of ICU stay. The incidence of ICUAW is estimated to be 30%-90% depending on the method and time of diagnosis. [1,2] It is characterized by profound muscle weakness and diminished or absent deep tendon reflexes [3,4] and is associated with delayed weaning from mechanical ventilation, [5] suggesting a possible relationship between limb and respiratory neuromuscular involvement. In addition, the syndrome is associated with prolonged hospitalization and increased mortality. [6]
There are a number of ways for assessing objectively muscle strength, which can be categorized as techniques that quantify maximum voluntary contraction force and those that assess evoked (stimulated) muscle force. Important factors that limit the repetitive evaluation of maximum voluntary contraction force in intensive care unit patients are learning effects, pain during muscular contraction, and alteration of consciousness.
Diagnostic strategies include specialized neurophysiologic testing and the bedside Medical Research Council physical strength exam. Neurophysiologic testing, such as electromyography, can be performed on ICU patients; however, interpretation requires special expertise, is not universally available in all ICUs and can be compromised by confounding factors such as generalized tissue edema. In contrast, the bedside strength exam can be performed by most clinicians. However, to be performed properly the strength exam requires an awake and attentive patient with the mobility and stamina to participate in the evaluation by MRC of all twelve major limb muscle groups. A simpler assessment may result in improved recognition of ICUAW. One such measure is handgrip dynamometry, which has been used as a surrogate for global strength in other neuromuscular diseases.[7-9]
One out of three patients dismissed from the ICU appear to face serious functional disorders and one out of four decreased mobility. [10,11] The functional ability and muscle strength of patients in relation to the presence of ICUAW after their discharge from the Intensive Care Unit (ICU) has not been extensively studied. Despite this, little is known about patient functional outcome. [12] Medical research in the ICU has traditionally focused on outcomes such as length of stay (LOS), length of ventilation and mortality.
The Functional Independence Measure (FIM) was used to assess the functional ability of ICU survivors and after 8 months. The FIM scale assesses physical and cognitive disability and focuses on the burden of care.
We hypothesized that patients discharged from the ICU will be inflicted by diminished muscle strength and that would affect their functional ability and that these impairments will be more pronounced in patients with ICUAW. The aim of this study was the assessment of muscle strength and functional ability of ICU survivors after ICU discharge.
Methods
Patients
The study was approved by the Scientific Council and the Ethics Committee of our Hospital. Written informed consent was given by family members of all the patients included in the study. All patients consecutively assessed at discharge from the multidisciplinary 28-bed university ICU during a 19 months study period. As in previous studies, [13,14] all patients over the age of 18, with an APACHE II admission score ≥ 13, with ICU stay > 48 hours and able to follow simple commands were considered for inclusion in the study.
Exclusion criteria were: age under 18, pregnancy, obesity (BMI>35 kg/m2), preexisting neuromuscular disease (e.g. myasthenia Gravis, Guillain-Barré), diseases with systemic vascular involvement such as lupus erythematosus etc.
The sequential organ failure assessment (SOFA)15 and Acute Physiology and Chronic Health Evaluation (APACHE II)16 severity scores were calculated for all patients on the day of admission in ICU.
Diagnosis of ICUAW and muscle strength assessment
The Medical Research Council (MRC) score for clinical assessment of muscle Strength was used for the diagnosis of ICUAW. [5] After interruption of sedation patients were screened daily for awakening and comprehension until ICU discharge. MRC was assessed on the day the patients had a level of consciousness adequate to respond to at least three of the following orders (“open/close your eyes”, “look at me”, “put out your tongue”, “nod your head”, “raise your eyebrows”). [2] Three muscle groups in all four limbs were assessed with the MRC scale with values ranging from 0 (quadriplegia) to 60 (normal muscle strength). The following functions were assessed: wrist flexion, forearm flexion, shoulder abduction, ankle dorsiflexion, knee extension, hip flexion. [17] Patients with an MRC score <48/60 were diagnosed with ICUAW. The cut off limit of 48 for the MRC score was selected because it indicates clinically significant weakness and has been used previously for the clinical identification of ICUAW. [5] The MRC score was performed by two independent investigators that were familiar with this technique and no more than 24 hours elapsed between the two measurements. The two investigators were unaware of each other assessment and they provided written MRC scoring for each muscle group that was assessed. The mean value of the MRC score of the two investigators was used for the diagnosis of ICUAW.
After the ICU discharge patients were evaluated by MRC score every 10 days.
Handgrip Dynamometry
Reliable and valid evaluation of hand strength can provide an objective index of general upper body strength. The power grip is the result of forceful flexion of all finger joints with the maximum voluntary force that the subject is able to exert under normal biokinetic conditions. The synergistic action of flexor and extensor muscles and the interplay of muscle groups is an important factor in the strength of the resulting grip. [18]
Patients were sited with their lumbar spine flexed in 140o , their shoulder and forearm in neutral position and elbow flexed 900 degrees. From each hand 5 successive measurements were taken, and the highest score was the one to be evaluated.
After the ICU discharge, patients were evaluated by Hand Grip dynamometry every 10 days. Immediately after the MRC exam, the same examiner asked subjects to perform hand dynamometry (Jamar handgrip dynamometer; Lafayette 78010, Lafayette Instrument Company, Indiana, USA.IL).
Functional Independence Measure
The FIM scale assesses physical and cognitive disability. [19] Items are scored on the level of assistance required for an individual to perform activities of daily living. The FIM scale is used to measure the patient’s progress and assess rehabilitation outcomes. This scale is useful in clinical settings of rehabilitation. The scale includes 18 items, of which 13 items are physical domains based on the Barthel Index and 5 items are cognition items. Each item is scored from 1 to 7 based on level of independence, where 1 represents total dependence and 7 indicates complete independence. The scale can be assessed by a physician, nurse, therapist. [19] Possible scores range from 18 to 126, with higher scores indicating more independence.
The FIM score is applied to the following areas of functional ability as: eating, grooming, bathing, dressing (upper body), dressing (lower body), toileting, bladder management, bowel management, transferring (to go from one place to another) in a bed, chair, and/or wheelchair, transferring on and off a toilet, transferring into and out of a shower, locomotion (moving) for walking or in a wheelchair, and locomotion going up and down stairs. The FIM score is also used for cognitive areas such as comprehension, expression, social interaction, problem solving, and memory.
Alternatively, 13 physical items could be scored separately from 5 cognitive items. Patients were assessed with FIM score at hospital discharge by observation and interview with the patient or the caregiver and at 8 months after ICU discharge by telephone interview with the patient or the caregiver. [20]
Other variables collected from the medical record included ICU LOS, hospital LOS.
Statistical analysis
Normality of distribution was checked by employing Kolmogorof - Smirnof test. Baseline characteristics of continuous variables of the ICUAW group and no ICUAW group for the whole cohort, those finally evaluated were compared by unpaired Student’s t-test or Mann-Whitney U test, in case of not normal distribution. Paired data were analyzed with Wilcoxon’s test and Repeated Measures Analysis of Covariance (ANCOVA).
The Kaplan-Meier method was used to compare the duration of ICU stay and Hospital stay, between patients with and without ICUAW. The two groups were compared using the long-rank test. All continuous variables are presented by mean ± SD or median and interquantile range in case of not normal distribution. In all cases, statistical significance level was set at p<0.05.
Results
Study population
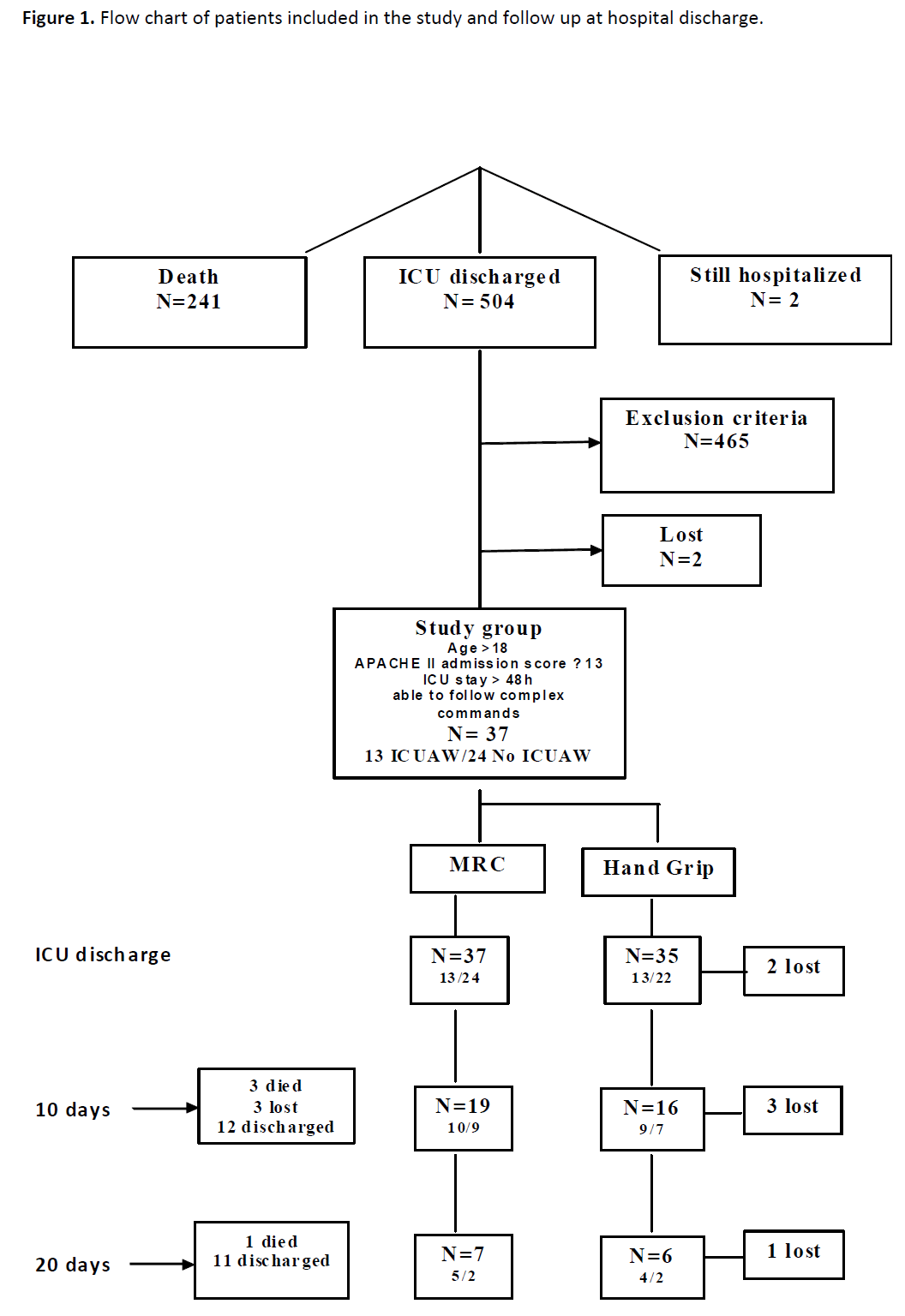
Seven hundred and fifty seven patients were admitted to our multidisciplinary ICU during the 19-month study period. During this period 504 patients had been discharged from the ICU, 241 died. Of the 504 patients, 465 patients fulfilled the exclusion criteria or had an ICU stay of less than 48 hours. Of the remaining 39 patients, 2 were lost at the follow up (Figure 1). Finally 37 patients were included in the study. Patients’ baseline characteristics are presented in Table 1.
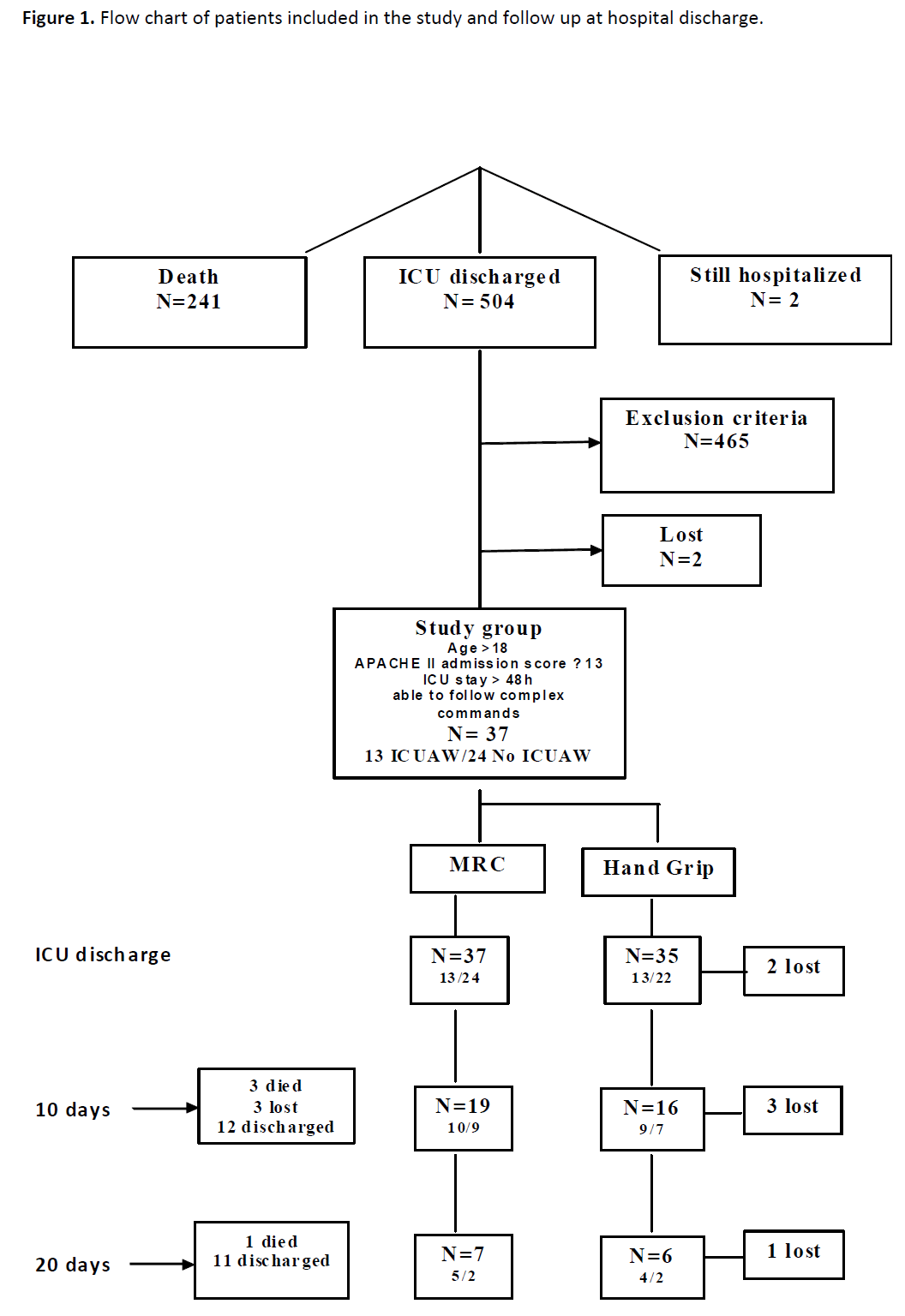
Figure 1: Flow chart of patients included in the study and follow up at hospital discharge.
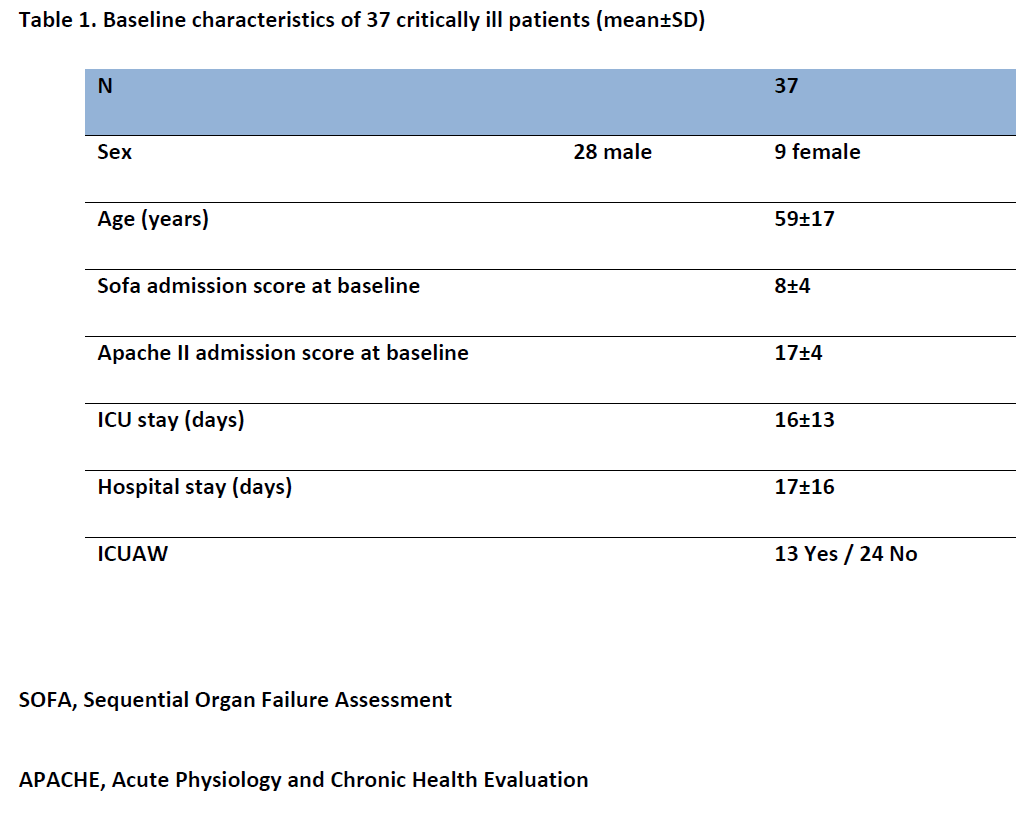
Of the 37 patients that dismissed from the ICU, ICUAW was diagnosed in 13 patients.
Νo significant difference was found between the ICUAW group and the no ICUAW group in, SOFA sore [8 (4-12) vs 8 (6-11), p=0.65] and APACHE II [19 (15-20) vs 18 (13-19), p=0.71]. Age was higher at the ICUAW group [67±15 vs 54±16, years, p=0.016].
At the 10-day follow up 12 patients had been discharged from the hospital and 4 patients had died. Of the 22 remaining patients 19 patients were evaluated with the MRC score and 3 were lost to the follow up.
At the 20-day follow up 11 patients had been discharged from the hospital and 1 patient had died. The 7 remaining patients were evaluated with the MRC score.
Thirty five patients were initially evaluated with the handgrip dynamometry and 2 patients were lost due to technical reasons. At the 10-day follow up after ICU discharge 16 patients, were evaluated with the handgrip dynamometry and 6 were lost to follow up. At the 20-day follow up after ICU discharge 6 patients, were evaluated with the handgrip dynamometry and 1 were lost to follow up. (Figure 1).
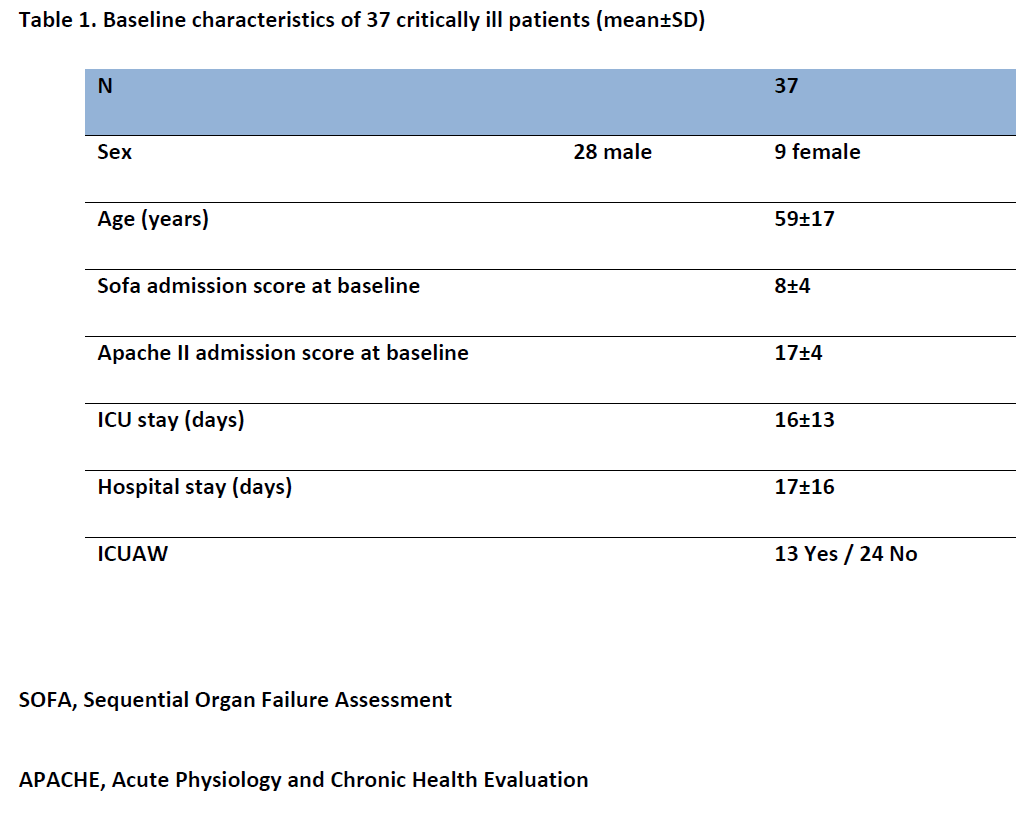
ICU length of stay
Patients that developed ICUAW had a longer ICU stay as compared to patients that did not develop ICUAW [26 (12-42) vs 11 (5-14), days, log-rank test, p=0.002] (Figure 2).
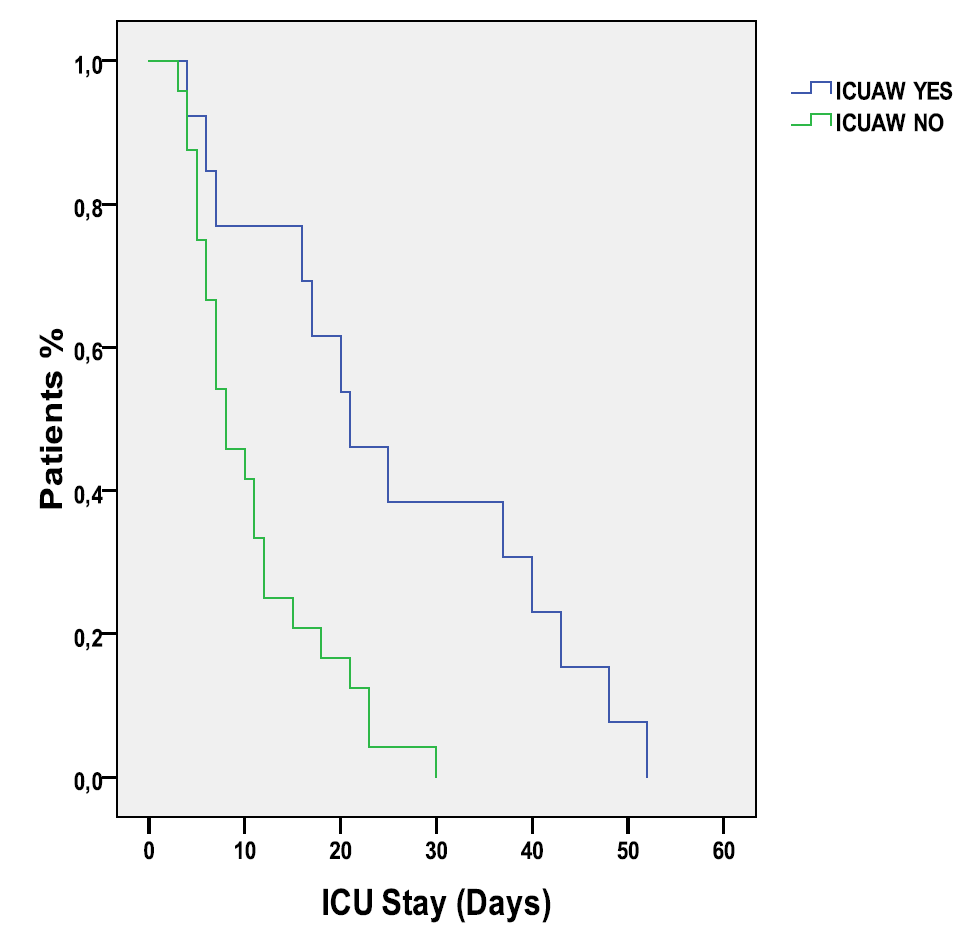
Figure 2
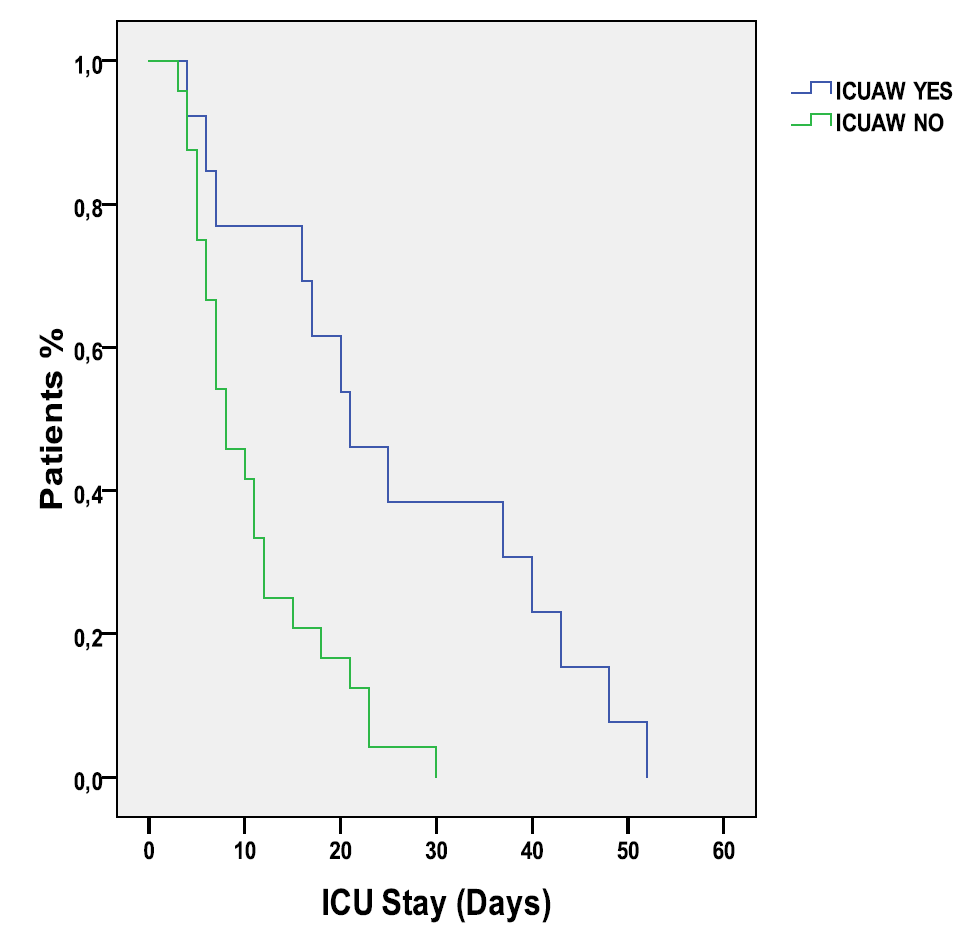
Hospital length of stay
Of the 37 patients that dismissed from the ICU, 4 died. Patients that developed ICUAW had a longer ICU stay as compared to patients that did not develop ICUAW [28 (10-43) vs 13 (5-22), days, respectively, log-rank test, p=0.025] (Figure 3).
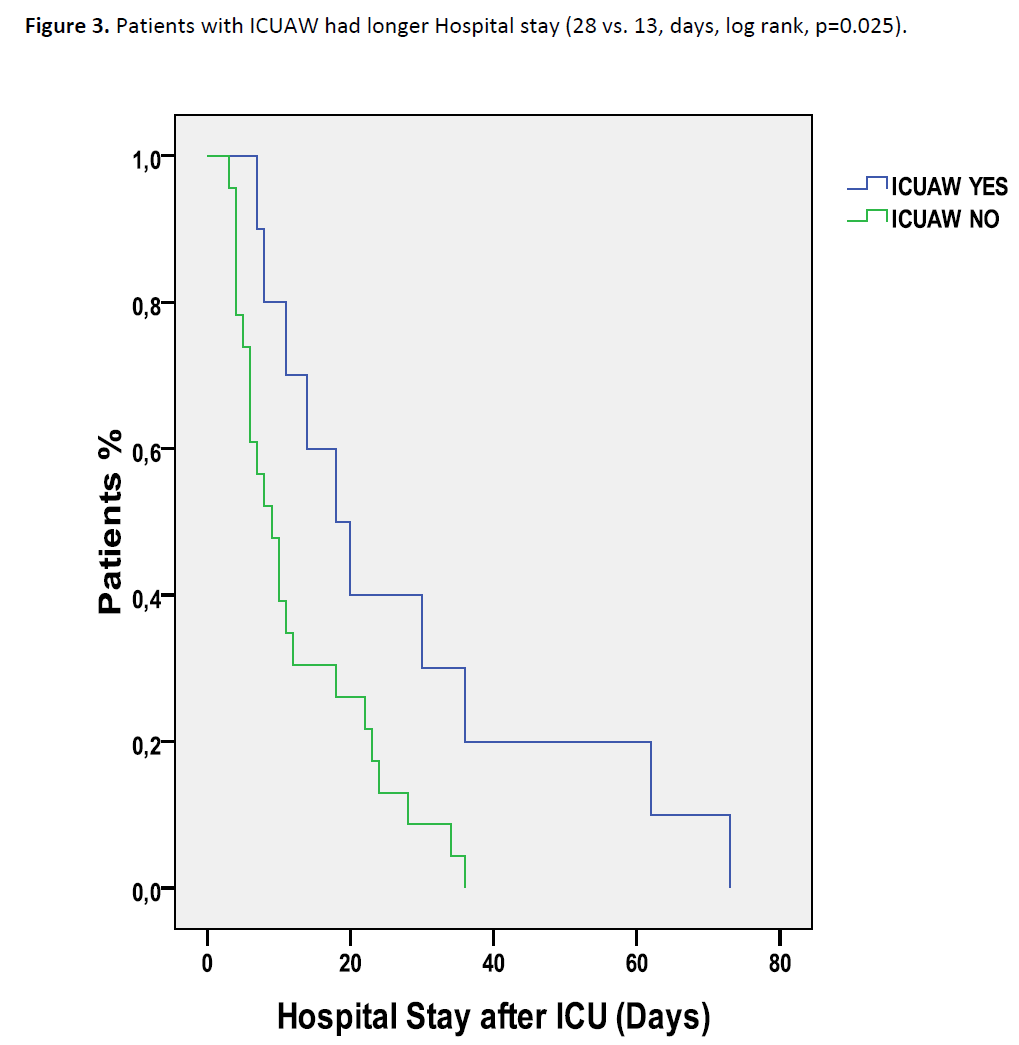
Figure 3: Patients with ICUAW had longer Hospital stay (28 vs. 13, days, log rank, p=0.025).
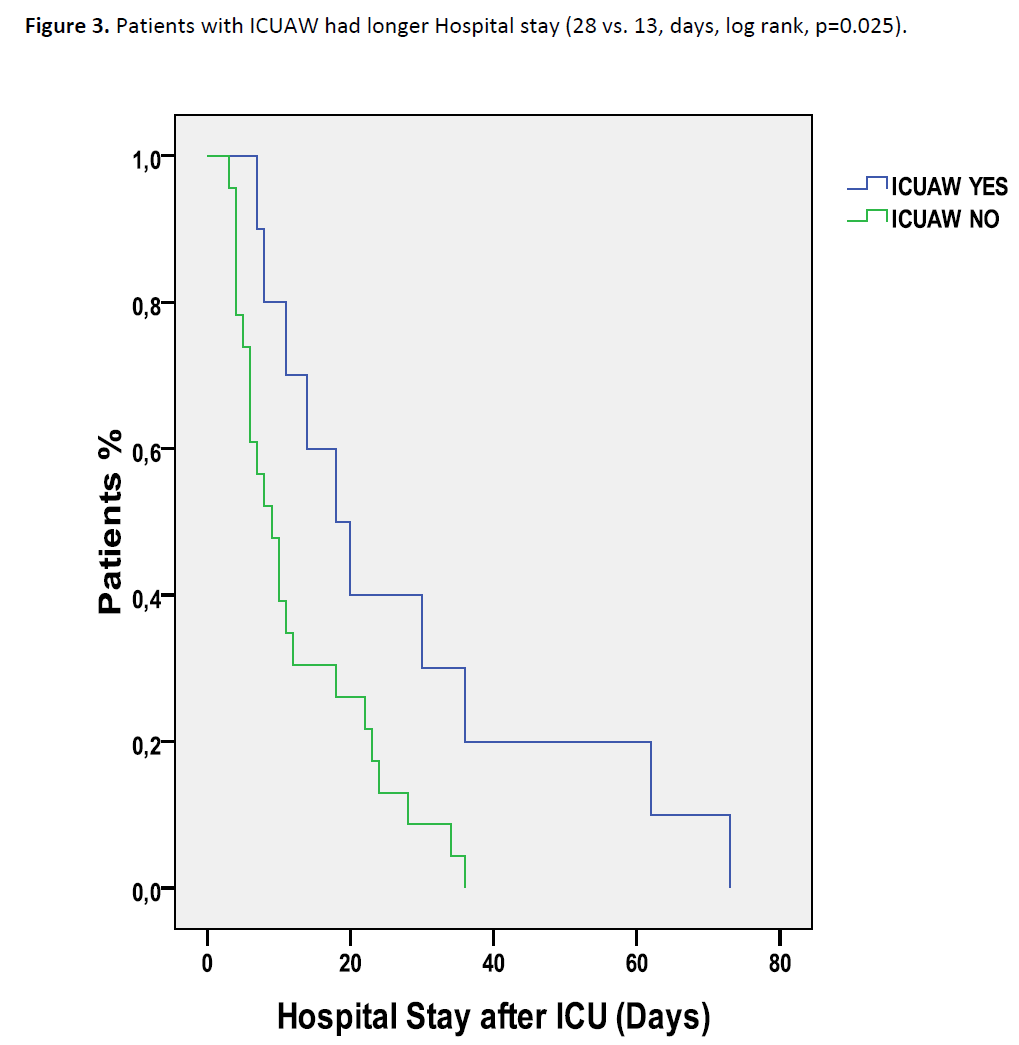
Muscle strength
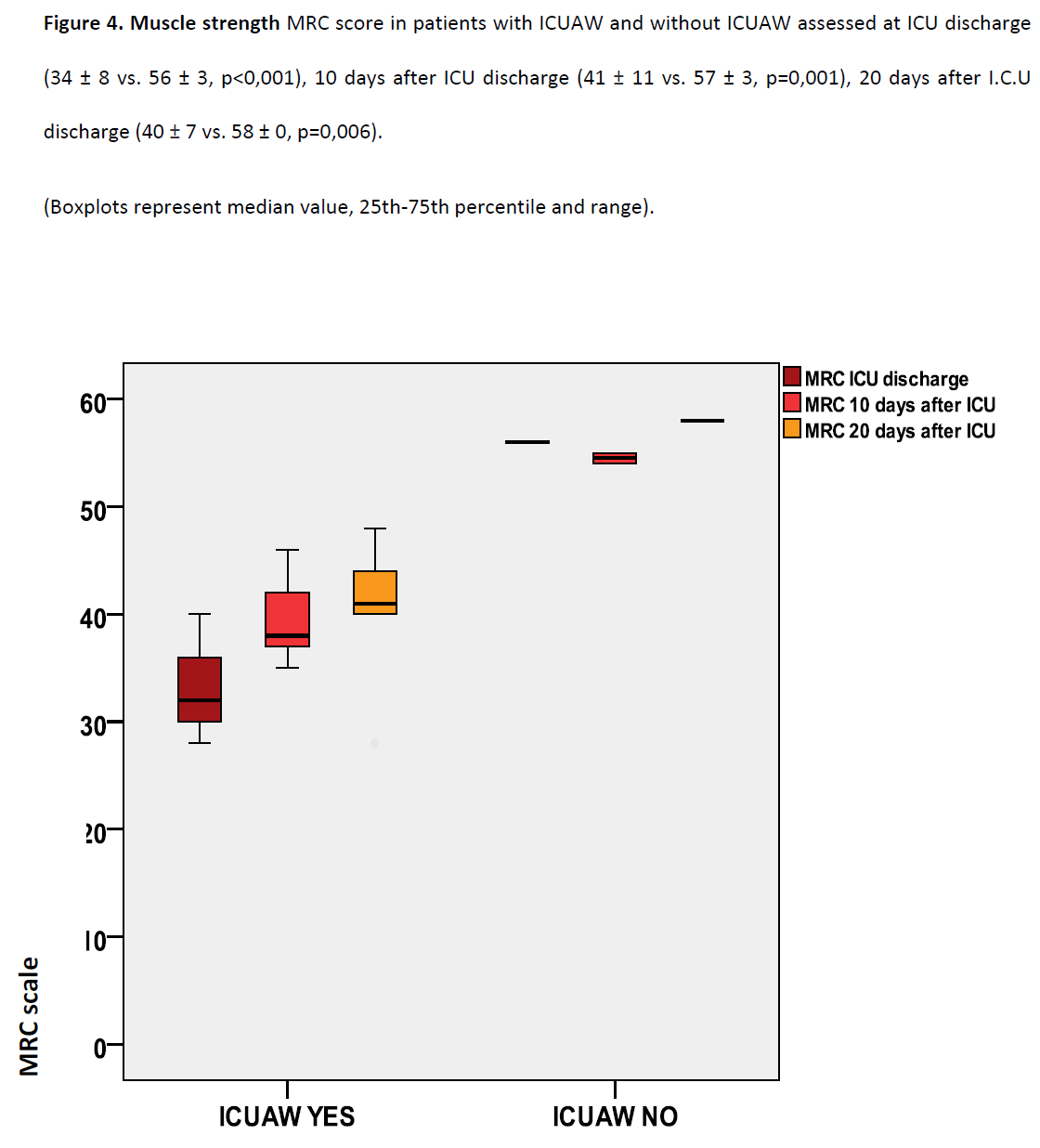
The MRC score was significantly lower in patients with ICUAW as compared to the no ICUAW group at ICU discharge (34±8 vs 56±3, p<0 .001) (Figure 4).
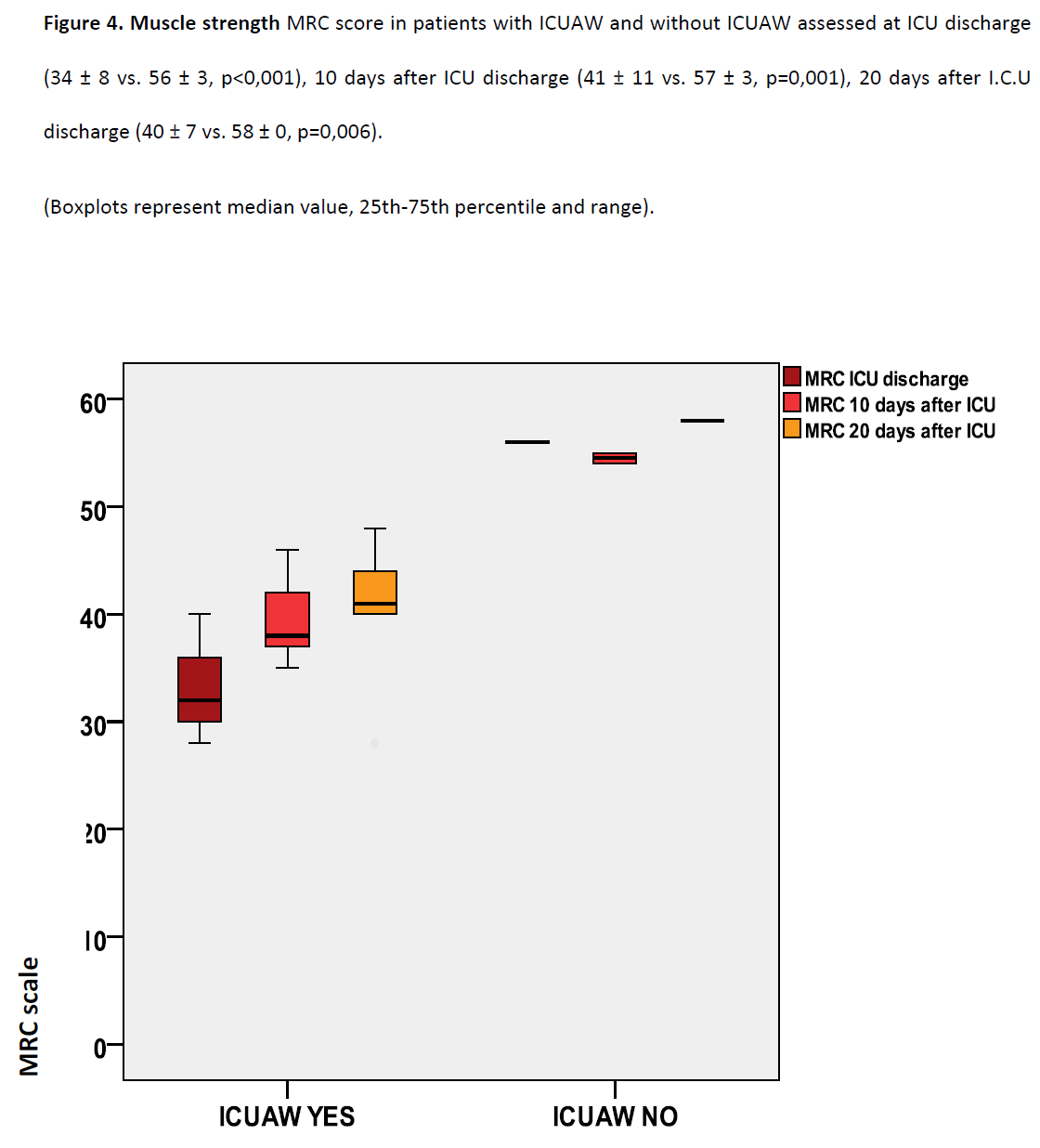
Figure 4: Muscle strength MRC score in patients with ICUAW and without ICUAW assessed at ICU discharge (34 ± 8 vs. 56 ± 3, p<0,001), 10 days after ICU discharge (41 ± 11 vs. 57 ± 3, p=0,001), 20 days after I.C.U discharge (40 ± 7 vs. 58 ± 0, p=0,006).
Ten days after ICU discharge ICUAW patients had significantly lower MRC score (41±11 vs 57±3, p=0.001, n=19) (Figure 4). Twenty days after ICU discharge ICUAW patients had significantly lower MRC score (40±7 vs 58±0, p=0.006, n=6) (Figure 4).
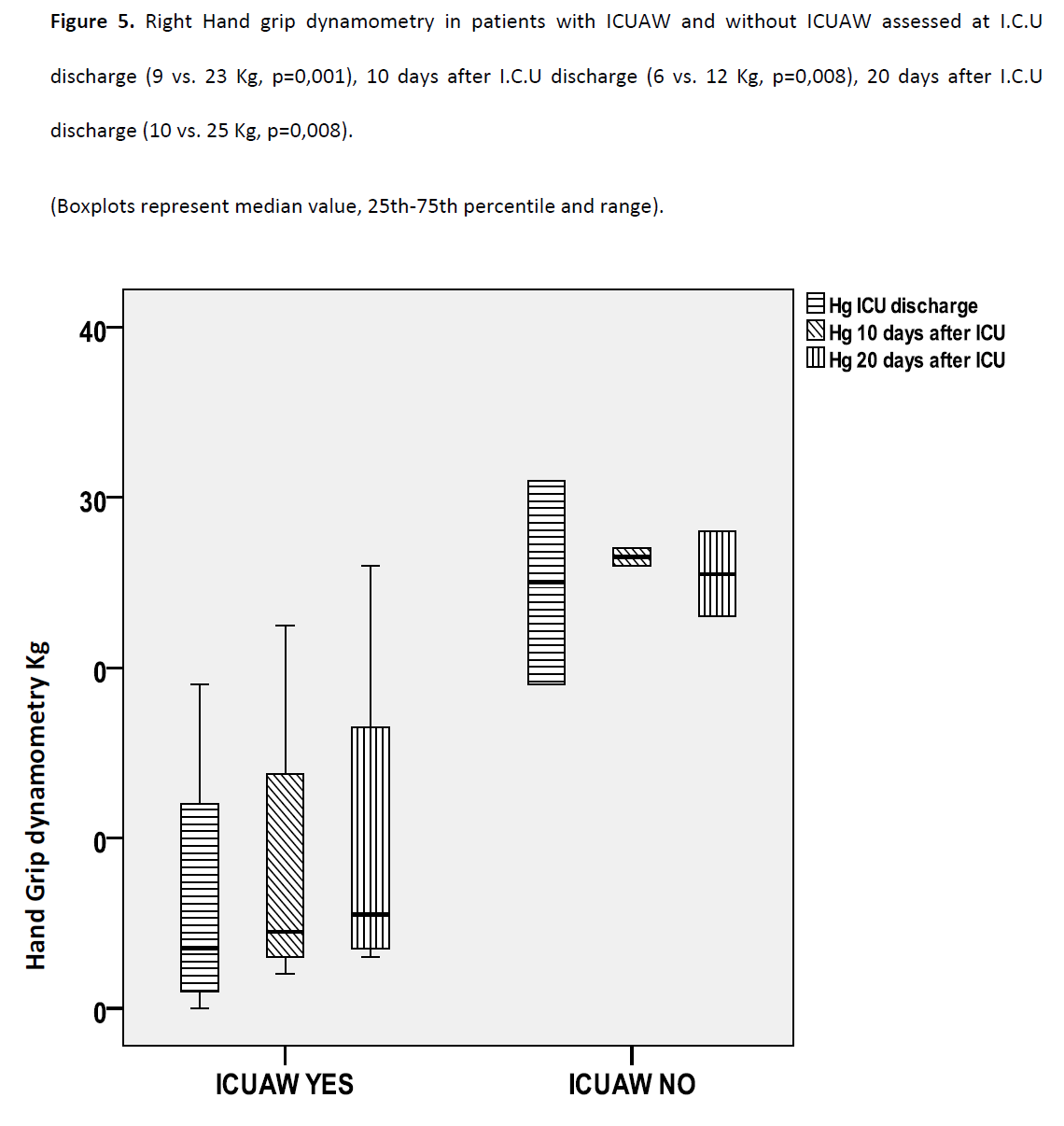
Patients with ICUAW had significantly lower muscle strength at ICU discharge, at the right-hand as assessed with hand grip dynamometry [9 kg (2-13) vs 23 kg (14-29), p=0.001] (Figure 5).
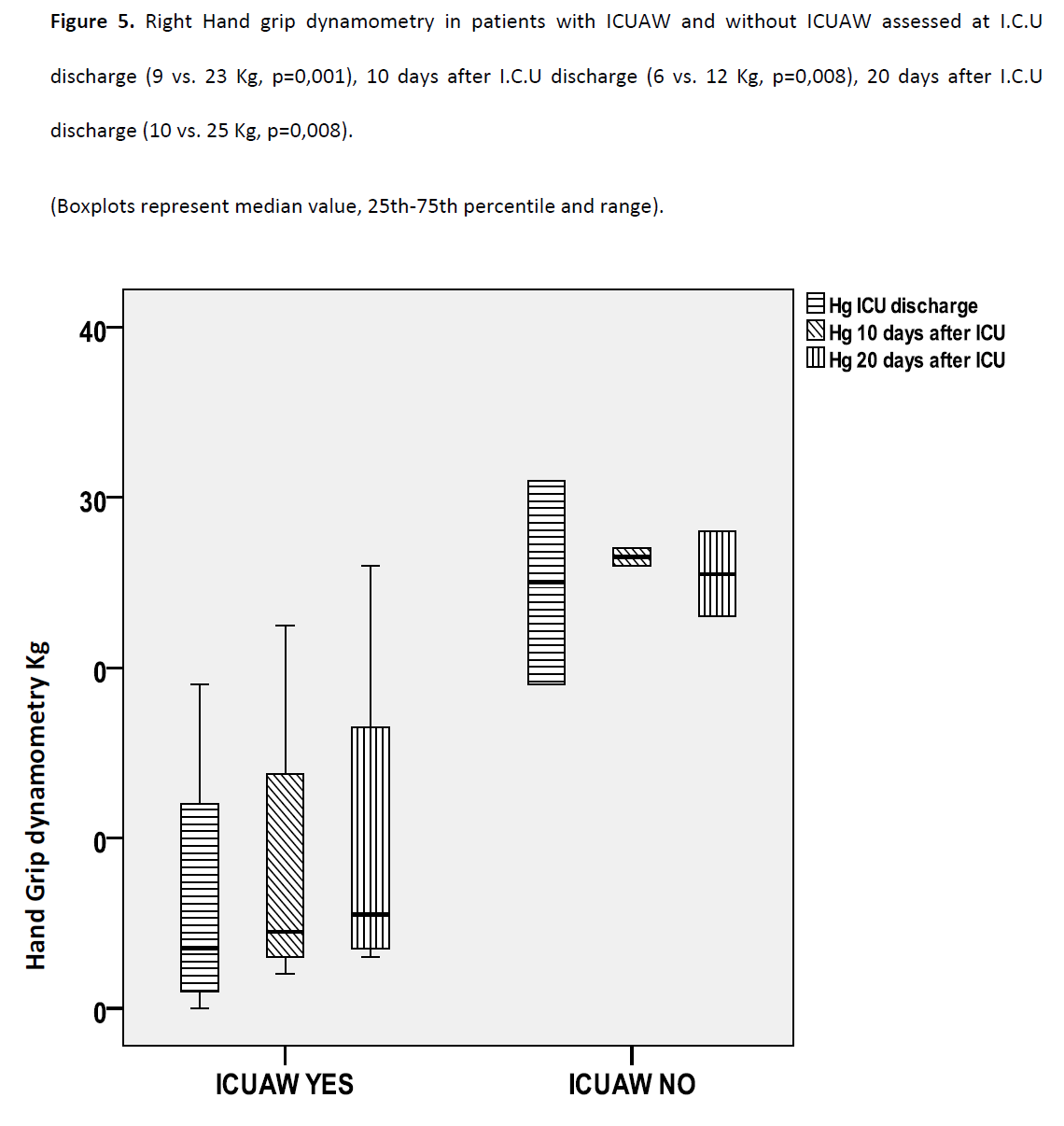
Figure 5: Right Hand grip dynamometry in patients with ICUAW and without ICUAW assessed at I.C.U discharge (9 vs. 23 Kg, p=0,001), 10 days after I.C.U discharge (6 vs. 12 Kg, p=0,008), 20 days after I.C.U discharge (10 vs. 25 Kg, p=0,008).
Ten days after ICU discharge ICUAW patients had lower muscle strength after the evaluation by the hand grip dynamometry [6 kg (3-14) vs 12 kg (12-27), p=0.008]. (Figure 5).
Twenty days after ICU discharge ICUAW patients had lower muscle strength after the evaluation by the hand grip dynamometry [10 kg (3-21) vs 25 kg (23-28), p=0.008]. (Figure 5).
Functional ability
The functional ability was assessed with the FIM score at ICU discharge and after 8 months in a subgroup of patients.
23 patients were evaluated with the FIM score at hospital discharge and 12 patients were evaluated after 8 months with the FIM score (3 died and 8 lost at the follow up). The FIM score improved significantly 8 months after hospital discharge (68±27 vs 104±27, p=0.004). Patients with ICUAW tended to have a lower FIM score at hospital discharge and 8 months after hospital discharge however it did not reach statistical significance (n= 23 64±22 vs 71±30, p=0.5 and n=12 90±27 vs 110±26, p=0.2).
Discussion
ICUAW has significant effects on patients recovery during their stay in ICU and even when they are transferred to the ward. Patients with ICUAW develop neuromuscular abnormalities that include muscle atrophy, paresis, impaired deep tendon flexes and affects rehabilitation in 100% of ICU survivors that stayed in ICU for at least 4 weeks. [21]
First finding of the study is that patients with ICUAW suffer from profound muscle weakness that is consistent even 2 weeks after ICU discharge. Severe muscle weakness is well documented in other studies as well, [10,22,23] and the diagnoses was made either with electromyography, or clinical examination, or biopsy, or a combination of the above. In accordance with other studies, we have shown that in mild cases there is a certain improvement in a few weeks, whilst in more severe case it may take months. This improvement is characterized by a progressive recovery of muscle strength along with sensation. However it seems that approximately half of these patients were fully rehabilitated [22,23] but still, in most cases physical impairment remain and in a few there is no restoration at all. [10]
Hand-grip strength is a subset of Hand grip dynamometry and enables measurement of force using a calibrated device for patients who are conscious and cooperative. Hand grip dynamometry is a reliable, rapid and simple alternative to comprehensive manual muscle test assessment [9] and may be a surrogate for global strength. [24] For the first time in our study, hand grip dynamometer is being used as an assessment tool for muscle strength of patients with ICUAW. Hand-grip dynamometry is significant reduced in patients with ICUAW even 20 days after ICU discharged something that is shown with MRC as well.
A second finding is the reduced functional ability as assessed with FIM. Muscle weakness has detrimental effects on physical function as this is measured by FIM. This impairment in functional ability is evident during hospital discharge and persists even 8 months after that. This impairment in functional ability reflects a compromise in quality of life that is present even 8 months after ICU discharge. These data are consistent with other reports [10,22] but FIM instrument was never used for the evaluation of these patients. Severe disability with tetraparesis, tetraplegia, or paraplegia was reported in a review by 28% of patients with ICUAW.23 In ARDS survivors impairments in functioning due to muscle atrophy and weakness still occur even 1 year from hospital discharge. Clinical and electrophysiological findings may be evident even 5 years after hospital discharge. [25]
Using the modified FIM, Livingston and colleagues, found that ICU survivors had significant impairment more than 3 years after severe injury, including inability to return to work. [26]
So far association of patients age on the development of ICUAW has given differential results. In one study [27] older age was associated with ICUAW while in one other [28] was even found to have a protective role, something that the authors were unable to explain. The results of our study showed that the mean value of patients age with ICUAW was larger than those.
Finally, as previously reported it was found a prolonged ICU and Hospital stay in patients with ICUAW.
Limitations
A limitation of the study is the small number of patients evaluated so far. Additional study of a larger number of patients is essential to verify these results and assess functional outcome and quality of life in these patients.
Finally, Post hospital physiotherapy at home, was not recorded at the present study.
Conclusions
Patients with ICUAW had a significantly longer ICU and hospital stay. They also had significantly lower muscle strength at their discharge from the ICU which remained compromised during hospital stay. The functional ability as assessed with the FIM score improved after 8 months, however it tended to remain lower in patients with ICU acquired weakness. It seems that the development of ICU acquired weakness affects the mobility of the patients, even after their discharge from the ICU, with negative impact to their functionality and the duration of their hospitalization. Further studies are warranted to assess the long term effect of ICU acquired weakness on the mobility, functional ability and quality of life in these patients.
3025
References
- Nanas S, Kritikos K, Angelopoulos E, Siafaka A, Tsikriki S, Poriazi M, et al. Predisposing factors for critical illness polyneuromyopathy in a multidisciplinary intensive care unit. Acta NeurolScand 2008, 118(3):175-181.
- De Jonghe B, Bastuji-Garin S, Durand MC, Malissin I, Rodrigues P, Cerf C, et al. Groupe de Réflexion et d'Etude des Neuromyopathies en Réanimation. Respiratory weakness is associated with limb weakness and delayed weaning in critical illness. Crit Care Med. 2007;35(9):2007-15.
- C F Bolton, D A Laverty, J D Brown, N J Witt, A F Hahn, W J Sibbald. Critically ill polyneuropathy: electrophysiological studies and differentiation from Guillain-Barre syndrome.JNeurolNeurosurg Psychiatry 1986; 49(5):563–573.
- Bolton CF. Neuromuscular manifestations of critical illness. Muscle Nerve 2005;32(2):140-163.
- De Jonghe B, Bastuji-Garin S, Sharshar T, Outin H, Brochard L. Does ICU-acquired paresis lengthen weaning from mechanical ventilation- Intensive Care Med 2004;30(6):1117–1121.
- Garnacho-Montero J, Madrazo-Osuna J, García-Garmendia JL, Ortiz-Leyba C, Jiménez-Jiménez FJ, Barrero-Almodóvar A, et al. Critical illness polyneuropathy: risk factors and clinical consequences. A cohort study in septic patients. Intensive Care Med 2001; 27(8):1288—1296.
- Visser J, Mans E, de Visser M, Van den Berg-Vos RM, Franssen H, de Jong JM, et al. Comparison of maximal voluntary isometric contraction and hand-held dynamometry in measuring muscle strength of patients with progressive lower motor neuron syndrome. NeuromusculDisord 2003;13(9):744–750.
- Merlini L, Mazzone ES, Solari A, Morandi L. Reliability of hand-held dynamometry in spinal muscular atrophy. Muscle Nerve 2002;26(26):64–70.
- Ali NA, O’Brien JM Jr, Hoffmann SP, Phillips G, Garland A, Finley JCW, et al. Acquired weakness, handgrip strength and mortality in critically ill patients. Am J RespirCrit Care Med 2008;178(3):261-8.
- Fletcher SN, Kennedy DD, Ghosh IR, Misra VP, Kiff K, Coakley JH et al. Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med 2003; 31(4):1012—1016.
- Van Der Schaaf M, Beelen A, De Vos R. Functional outcome in patients with critical illness polyneuropathy. DisabilRehabil 2004; 26(20):1189—1197.
- Welton JM, Meyer AA, Mandelkehr L, Fakhry SM, Jarr S. Outcomes of and resource consumption by high-cost patients in the intensive care unit. Am J Crit Care 2002;11(5):467-73.
- Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al.Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009 ;373(9678):1874-82.
- Routsi C, Gerovasili V, Vasileiadis I, Karatzanos E, Pitsolis T, Tripodaki E, et al.Electrical muscle stimulation prevents critical illness polyneuromyopathy: a randomized parallel intervention trial. Crit Care 2010;14(2):R74.
- Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Crit Care Med 1998;26(11):1793-800.
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE: APACHE II: a severity of disease classification system. Crit Care Med 1985, 13(10):818 829.
- Kleyweg RP, van der Meché FG, Schmitz PI. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain- Barré syndrome. Muscle Nerve 1991; 14(11):1103-1109.
- Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S (Feb 1985). "Grip and pinch strength: normative data for adults". Arch Phys Med Rehabil 66 (2): 69–74.
- Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home support, long-term and acute care settings. Age Ageing 2007; 36(2): 130–39.
- Masedo AI, Hanley M, Jensen MP, Ehde D, Cardenas DD. Reliability and validity of a self-report FIM (FIM-SR) in persons with amputation or spinal cord injury and chronic pain. Am J Phys Med Rehabil 2005;84(3):167-176.
- Suter P, Armaganidis A, Beaufilis F. Consensus conference organized by the ESICM and the SRLF: predicting outcome in ICU patients. Intensive Care Med 1994;10(5):390-397.
- De Sèze M, Petit H, Wiart L, Cardinaud JP, Gaujard E, Joseph PA, et al. Critical illness polyneuropathy:a 2-year follow-up in 19 severe cases. EurNeurol 2000;43(2):61–69.
- Nicola Latronico, IndritShehu, Elisa Seghelini. Neuromuscular sequelae of critical illness. CurrOpinCrit Care 2005; 11(4):381—390.
- Stevens RD, Marshall SA, Cornblath DR, HokeA, Needham DM, de Jonghe B, et al. A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med 2009;27(10 Suppl.):S299—308.
- Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 2011;364(14):1293-304.
- Livingston D, Tripp T, Biggs C, Lavery L, A fate worse than death- Long-term outcome of trauma patients admitted to the surgical intensive care unit. J Trauma 2009; 67(2):341-8.
- De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, et al. Paresis acquired in the intensive care unit: a prospective multicenter study.JAMA 2002;288(22):2859-67.
- Hermans G, Wilmer A, Meersseman W, Milants I, Wouters PJ, Bobbaers H, et al. Impact of intensive insulin therapy on neuromuscular complications and ventilator dependency in the medical intensive care unit. Am J RespirCrit Care Med 2007;175(5):480-9.