Olajide Olushola1, Onabolu Oluwatoni2, Jagun Omodele1*, Betiku Anthony1, Alao Gboyega3, Aham-Onyebuchi Ugochi1 and Leshi Mojisola1
1Ophthalmology Unit, Babcock University Teaching Hospital, Ilishan-Remo, Ogun State, Nigeria
2Ophthalmology Unit, Olabisi Onabanjo University Teaching Hospital, Sagamu, Ogun State, Nigeria
3Department of Family Medicine, University College Hospital, Ibadan, Oyo State, Nigeria
*Corresponding Author:
Dr. Jagun Omodele
Ophthalmology Unit, Babcock University Teaching Hospital
Ilishan-Remo, Ogun State, Nigeria
Tel: +234-8023184198
E-mail: Omodelly@yahoo.com
Received Date: 21.11.2016; Accepted Date: 13.12.2016; Published Date: 23.12.2016
Keywords
Glaucoma; Deteriorating vision; Blindness; Cup-disc ratio
Introduction
Glaucoma refers not to a single disease, but to a group of disorders, characterized by optic neuropathy (cupping and atrophy of the optic nerve head) and a characteristic visual field loss [1]. It is the second most common cause of blindness and the leading cause of irreversible blindness worldwide [1]. Glaucoma affects up to 2% of those over the age of 40 years globally, and up to 10% over the age of 80 while 50% may be undiagnosed [2]. The estimated prevalence of glaucoma varies widely across population based samples. The Rotterdam Study [3] shows a prevalence of 0.8% for open angle glaucoma while the Barbados Eye Study reported a prevalence of 7% for open angle glaucoma in blacks, 3.3% in mixed race and 0.8% in whites [4]. Tham et al. found the global prevalence of glaucoma for population aged 40-80 years to be 3.5% [5].
There are several classifications of glaucoma which includes anatomic, gonioscopic, biochemical, molecular, and genetic views and each has its own merit. Appropriate management of glaucoma depends on the clinician's ability to diagnose the specific form of glaucoma in a given patient, determine the severity of the condition, and detect progression in that patient’s disease status. It is often useful to question the patient specifically about symptoms and conditions associated with glaucoma, such as pain, redness, colored halos around lights, alteration or loss of vision, bumping into objects and family history of blinding eye disease. Many cases of glaucoma go unidentified and untreated, even in developed countries [6] especially because there is currently no test or combination of tests that provides a reasonable balance of sensitivity and specificity that would support the development and conduct of population-based screening programs for glaucoma [7]. Despite being the most common cause of irreversible blindness worldwide, diagnosis of glaucoma is not included in the Vision 2020 strategic plan. The World Health Organization (WHO), using data from late 1980’s and early 1990’s estimated that 104.5 million people have intra ocular pressures (IOP) >21 mmHg [8] (normal:10-21 mmHg) and 2.4 million new cases of primary open angle glaucoma per annum are seen globally [8]. In 2013, the number of people (aged 40-80 years) with glaucoma worldwide was estimated to be 64.3 million, and this is expected to increase to 76 million by 2020 [5]. The prevalence of primary open angle glaucoma is highest in Africa (4.20%) [5] and the prevalence of primary angle closure glaucoma is documented to be highest in Asia (1.09%) [5].
In Nigeria, most studies on glaucoma have been hospital based due to the difficulties and technicalities required for community screening. Prevalence of glaucoma in these hospital based studies have been reported as 8.7% [9] 29.4%, [10] with primary open angle glaucoma being 51.2%, [10] 73.4%, [11] while elsewhere in Africa the prevalence of primary open angle glaucoma was as high as 76.9% [12], and 54.2% [13] but a lower value was noted in Brazil 37.7% [14]. The main rationale for this retrospective study is to determine the prevalence of glaucoma among patients presenting at the eye clinic of Babcock University Teaching Hospital, to report the clinical presentation, types of glaucoma and the disease severity in the patients at presentation as these would have serious public health consequences in the prevention of blindness strategies.
Methodology
Study area
Babcock University Teaching Hospital, Ilishan, Ogun State is 45 km equidistance between Lagos and Oyo states in Nigeria. The hospital subserves Babcock University, Ilishan town, neighboring communities and cities such as Lagos, Ibadan and Abeokuta.
Methodology
A retrospective study of patients diagnosed with glaucoma on presentation to the eye clinic for the first time, between July 2012 and June 2015. All data were obtained from the patient’s hospital record files. Information obtained include demographic data (age, sex, occupation), presenting complaint, ophthalmic history and ophthalmic evaluation carried out (visual acuity (VA) classified according to the WHO definition of visual impairment) [15], intraocular pressure (IOP), gonioscopic findings using the Schaffer’s grading system, biomicroscopic optic disc assessment using a +78 diopter lens after eye has been dilated, central visual field (CVF) findings done with an automated perimeter (Opto AP100, China).
Glaucoma diagnosis
Diagnosis of glaucoma was made based on glaucomatous optic neuropathy (vertical cupping of the optic nerve head VCDR ≥ 0.5/0.6 ‘and not obeying the ISNT rule’ or difference of >0.2 between the 2 eyes) or a characteristic glaucomatous CVF defect [9,10]. Glaucoma was classified as Primary open angle base on open angle on gonioscopy and age ≥ 40 years, Juvenile open angle base on open angle on gonioscopy and age 40 at diagnosis [10], Primary angle closure base on angle closure on gonioscopy in more than 2 quadrants and age ≥ 40 years, juvenile angle closure base on angle closure on gonioscopy in more than 2 quadrants and age below 40, Secondary glaucoma base on the presence of an ocular or systemic abnormality predisposing to glaucoma e.g. trauma to the eye [10].
Data analysis
Done using SPSS 21 version.
Results
A total of 3,814 new cases were seen during the study period, 144 (3.78%) were newly diagnosed glaucoma cases. The mean age of these patients were 61.9 ± 19.5 years (range 13-88 years), 85 (59%) were age 60 years and above, 85 (59%) were males, showing a male preponderance and 93 (64.6%) of them attained a minimum of secondary school education (Table 1).
Table 1 Socio – demographic characteristics of patients.
| Age (years) |
N |
% |
| ≤ 20 |
10 |
6.9 |
| 21-30 |
5 |
3.5 |
| 31-40 |
6 |
4.2 |
| 41-50 |
9 |
6.3 |
| 51-60 |
29 |
20.1 |
| >60 |
85 |
59 |
| Sex |
N |
% |
| Male |
85 |
59 |
| Female |
59 |
41 |
| Level of Education |
N |
% |
| No formal education – primary school |
51 |
35.4 |
| Secondary school and above |
93 |
64.6 |
Presenting complain
Majority of the patients, 76.4% (110) complained of poor vision in one or both eyes at presentation. Eighteen (12.5%) presented on account of pain in one or both eyes while the remaining 11.1% (16) had no complain at presentation (Table 2).
Table 2 Presenting complaints and ocular history.
| Presenting Complaint |
N |
% |
| Deteriorating vision |
110 |
76.4 |
| Ocular pain |
18 |
12.5 |
| No complaints |
16 |
11.1 |
| Prior diagnosis |
N |
% |
| No prior diagnosis |
71 |
49.3 |
| < 1 year |
12 |
8.3 |
| 1-5 years |
40 |
27.8 |
| > 5 years |
21 |
14.6 |
| Prior treatment with drugs |
N |
% |
| Yes |
69 |
94.5 |
| No |
4 |
5.5 |
| Family history of glaucoma |
N |
% |
| Father/mother |
14 |
9.7 |
| Siblings |
2 |
1.4 |
| Children |
1 |
0.7 |
| No family history |
127 |
88.2 |
Glaucoma diagnosis and treatment
At presentation, 71 (49.3%) patients were newly diagnosed, 52 (36.1%) patients had been diagnosed for less than 5 years while 14.6% (21) had been diagnosed for over 5 years. Sixtynine patients (94.5%) of those previously diagnosed with glaucoma were already on medications. Eight (11.6%) out of the 69 patients who were on medications had also undergone glaucoma surgery prior to presentation (Table 2). Only 17 (11.8%) patients had a family history of glaucoma in their first degree relative (Table 2).
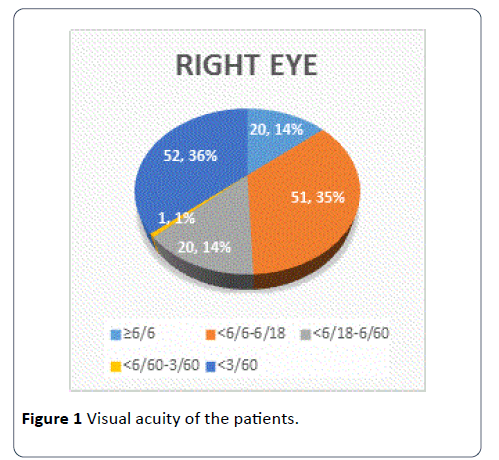
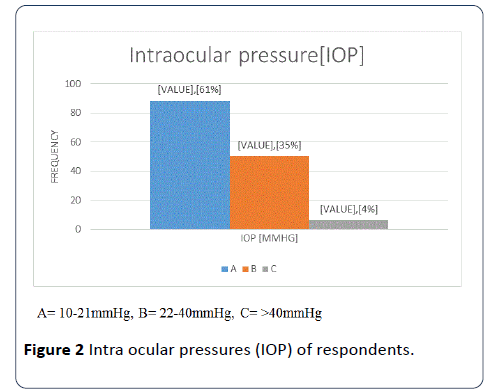
The cup to disc ratio (CDR) of the optic nerve head were similar in both eyes with 72% of the patients having a CDR ≥ 0.7 indicating advance disease while only 28% (41) ≤ 0.6 (Table 3). Intraocular pressure (IOP) was normal (IOP=10-21 mmHg) in 61% (88) of the patients’ right eyes (Figures 1 and 2).
Table 3 Vertical cup to disc ratio (VCDR) of the optic nerve heads of the patients.
| CDR |
Right eye |
Left eye |
| < 0.5-0.6 |
41 (28%) |
40 (28%) |
| 0.7-1.0 |
103 (72%) |
104 (72%) |
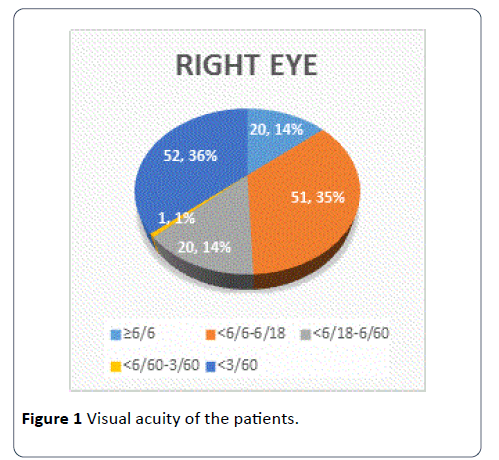
Figure 1: Visual acuity of the patients.
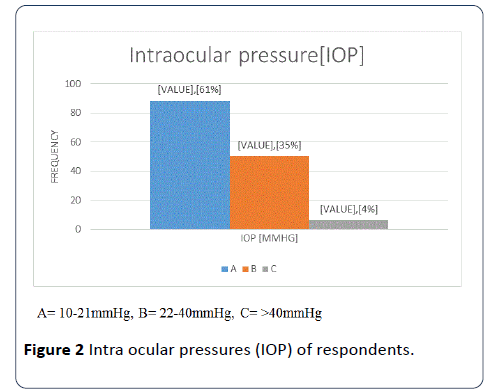
Figure 2:Intra ocular pressures (IOP) of respondents.
Base on gonioscopic findings, 75.7% (109) had primary open angle glaucoma, 8.3% (12) had primary angle closure glaucoma, 13.2% (19) were adjudged to have juvenile open angle glaucoma, 1.4% (2) had juvenile angle closure glaucoma, and 1.4% (2) had secondary glaucoma.
Only 34% (49) out of the 144 patients reviewed had a central visual field test (CVF) done (constrains ranged from financial issues to inability to fixate on target). The CVF defects seen were mainly arcuate scotoma 51% (25) and tunnel vision 10% (5) while 39% (19) had essentially normal visual fields.
Discussion
During the 3 years considered in this study, a total of 3,814 new cases were seen and 144 were diagnosed with glaucoma giving a prevalence of 3.8%. The results for each eye where found to be statistically similar, thus our discussion is based on the right eye findings where mono-ocular findings are indicated.
Twenty-one (14.6%) of the patients were noted to be ≤ 40 years. The early occurrence of glaucoma in blacks have also been demonstrated in different studies [10,16,17] with Olawoye et al. further postulating that this could be the reason for the higher rate of blindness from the disease experienced in blacks especially in developing countries since these individuals would tend to have the disease for a longer period [10].
The main (76.4%) presenting complain observed in these patients were deterioration of vision in one or both eyes and was similar to the findings by Adekoya et al. [18] in 75% of patients. This usually implies that there is a significant optic nerve neuropathy as it is a documented fact that by the time a glaucoma patient complains of loss of vision especially in Open angle glaucoma, there would have been up to 40-50% optic nerve damage, thus glaucoma is known as the ‘silent thief ‘of sight [2,4,8]. Only 8% had no complain at presentation and the diagnosis of glaucoma was made after routine eye examination for pre-admission/employment eye checks, these patients had no significant eye complains while some had a family member with a positive history of glaucoma. Adekoya et al. also documented a similar rate of 7.2% new cases diagnosed as part of routine eye examination [18]. Hence the need to include routine screening for glaucoma in the global or National prevention of blindness programs so that the world can then ‘Beat Invisible Glaucoma’ and reduce avoidable blindness as being advocated during the world glaucoma weeks over the last 2 years [19].
Thirty (20.8%) of the patients were bilaterally blind, while 37% (52) had monocular blindness. Those with bilateral blindness were noted to be slightly higher than previously documented 15.5% [18], 16.8% [10] and 17.7% [11] in Nigeria. The prevalence of blindness from glaucoma have been shown to be higher in developing countries as opposed to developed countries [14,20,21] and this can also be due to the late presentation noted amongst patients in developing countries [16,18].
Primary open angle glaucoma (POAG) was the most common type [75.7%] of glaucoma as also seen globally [1] and in Nigeria [9-11]. Juvenile open angle glaucoma was the second most common type accounting for 13.2% (19) cases out of which 38% had a positive family history of glaucoma, thus the need for routine eye screenings. The high prevalence of Juvenile glaucoma could also be due to the range of clientele seen at the eye clinic which includes the secondary and university students domicile in Babcock.
The need to have a governmental policy on regular or yearly eye examination cannot be over emphasised as 11.8% (17) of the total patients had a positive family history of glaucoma in a first degree family member (parents or siblings) and this value is likely to be higher as many of the patients had family members who had never been screened for glaucoma nor visited an eye care centre.
PACG was the third commonest type of glaucoma (8.3%) seen in this study. This is however higher than previous values from Ibadan (2.7%) [10].
Limitation of this study is that it is hospital based with limited number of patients seen within the period of the study.
Conclusion
The prevalence of glaucoma was significant with most patients presenting with advance disease. There is an urgent need to incorporate routine eye screenings in the general healthcare policies so as to detect invisible and early stages of glaucoma so as to prevent avoidable blindness.
17886
References
- Thylefors B, Negrel AD (1994) The global impact of glaucoma. Bull World Health Organ 72: 323-326.
- Kanski JJ, Brad B (2011) Clinical ophthalmology: A systematic approach. Elsevier Saunders, London.
- Wolfs RC, Borger PH, Ramrattan RS, Klaver CC, Hulsman CA, et al. (2000) Changing views on open-angle glaucoma: definitions and prevalences--The Rotterdam Study. Invest Ophthalmol Vis Sci 41:3309-3321.
- Leske MC, Connell AM, Schachat AP, Hyman LA (1994) The Barbados Eye Study: Prevalence of open angle glaucoma. Ophthalmol 112:821-829.
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, et al. (2014) Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology 121:11.
- Holló G, Kóthy P, Géczy A, Vargha, P (2010) Health anxiety in a non-population-based, pre-published glaucoma screening exercise. Eye.
- Tielsch JM, Katz J, Singh K, Quigley HA, Gottsch JD, et al. (1991) A population-based evaluation of glaucoma screening: The baltimore eye survey. Am J Epidemiol 1991: 1102-1110.
- American Academy of Ophthalmology (2016)GLAUCOMA: lifelong education for the ophthalmologist, (13thedn.).
- Omoti AE (2005) Glaucoma in Benin-city, Nigeria. Nig Postgrad Med J 12:189-192.
- Olawoye O, Tarella S (2014) Spectrum of glaucoma presentation in a Nigerian tertiary hospital. Niger J Ophthalmol 22:11-15.
- EpoEnock M (2010) Glaucoma in a suburban tertiary care hospital in Nigeria. J Ophthalmic Vis Res 5:87-91.
- Giorgis AT, Mulugeta A, Aga A, Deyassa N (2012) The spectrum of glaucoma presentation at Menelik II Hospital, Addis Ababa. Ethiop Med J 50:259-264
- Ntim-Amponsah CT, Amoaku WM, Ofosu-Amaah S, Ewusi RK, Idirisuriya-Khair R, et al. (2004) Prevalence of glaucoma in an African population. Eye 18: 491-497.
- Osaki TH, Kasahara N, Paolera MD, Cohen R, Nishiwaki-Dantas MC (2010) Presentation of glaucoma in an urban tertiary care hospital in South America: legal blindness and prevalence. IntOphthalmol 30:361-366.
- World Health Organization (1992) International classification of diseases, 10th revision (ICD-10). World Health Organization, Geneva, Switzerland.
- Nosiri C, Chawat S,Abba G (2009) Prevalence of glaucoma in Nigeria. Int J Epidemiol9: 1.
- Adekoya BJ, Shah PS, Onakoya AO, Ayanniyi AA (2014) Glaucoma in SouthwestNigeria : clinical presentation, family history and perception. Int Ophthalmology 34: 1027-1036.
- Giaconi JA, Salim S,Lim AK (2015) Primary versus secondary open angle glaucoma.