Keywords
Giant uterine leiomyoma; Muscular dystrophy; Post-operative nursing care
Introduction
Progressive muscular dystrophy is a group of genetic diseases with clinical and genetic features characterized by progressive skeletal muscle atrophy and weakness [1]. Mainly manifesting as progressive dystrophy of skeletal muscle and a gradual decrease in muscle strength, some patients may develop damage to the myocardium and liver and eventually lose the ability to exercise. It is a disease with high disability and mortality rates [2]. The main types of progressive muscular dystrophy include Duchenne (DMD), Myotonic (MMD), Limb-Girdle (LGMD), Facioscapulohumeral (FSH/FSHD), Becker (DMD), and Cogenital muscular dystrophy [1]. The underlying mechanisms of the clinical features of progressive muscular dystrophy include the disruption of cytoskeleton-ECM connections caused by mutations in the DMD gene, genetic mutation-induced aberrant glycosylation of α-dystroglycan, loss of integrin-mediated linkage between the ECM and cytoskeleton related to mutations in ITGA7, impaired cell signaling at the sarcolemma, defective sarcolemma repair, disintegration of muscle sarcomeres, toxic effects of RNA repetition during transcription with expansion of CTG triplets, and overexpression of toxic transcription factors [3,4].
Uterine leiomyomas are one of the most common types of benign tumors of the female reproductive tract, with an incidence of about 25%-45%, and are more common in women aged 30 to 50 [5-7]. Giant uterine leiomyomas, which weigh more than 11.4 kg, are very rare and exhibit atypical clinical presentations and a risk of malignancy, thereby representing an enormous challenge in diagnosis and therapy [8,9]. Giant uterine leiomyomas are a potentially fatal condition due to the pressure they cause on other organs [10]. Studies have shown that patients with muscular dystrophy are at increased risk of various types of tumors including melanoma, sarcomas, lymphomas, and malignant neoplasms in the brain, ovary, and thyroid [11,12].To date, there is only one case of a giant uterine tumor in a woman with muscular dystrophy reported by Kataoka et al, and they suggested the association of muscular dystrophy with a giant uterine tumor may be due to dysfunction of muscular dystrophy protein kinase, a tumor suppressor [13]. However, there is no literature on the strategies of nursing care delivery for patients with muscular dystrophy complicated with a concurrent giant uterine leiomyoma.
Herein, we present a rare case of a giant uterine leiomyoma in a 31-year old Chinese woman with muscular dystrophy. The post-operative nursing care delivery to this patient is reported.
Patient Information and Therapeutic Intervention
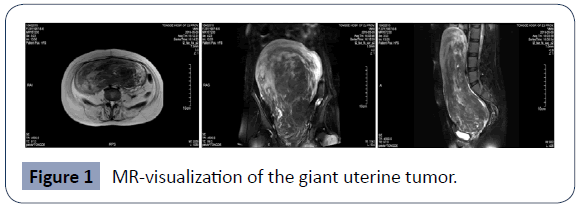
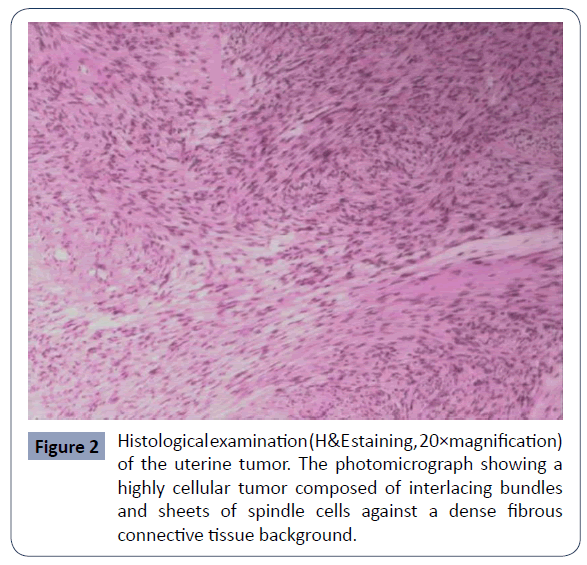
Written informed consent for this work was obtained from the patient. A 31-year-old woman presented to our hospital with compliant of increasing abdominal size, a 1-year history of a pelvic mass, a more than 10-year history of progressive muscular dystrophy, and moderate anemia. The muscle strength of both her upper and lower limbs was graded as level 2. Obvious muscle atrophy of the limbs was observed, and no tendon reflex was elicited in all 4 extremities.A giant uterine tumor measuring 250 mm x 102 mm x 60 mm was detected in MR (Figure 1). A total hysterectomy, bilateral resection of the fallopian tubes, removal of the broad ligament myoma, and separation of pelvic adhesions were performed 6 days after the patient was hospitalized. 2U of red blood cells were given during the operation and Clindamycin was administrated as symptomatic treatment after surgery and to prevent infection. Subserosal uterine leiomyoma was confirmed by histopathological diagnosis (Figure 2). The specimen was positive for SMA, Desmin, CD34, and Ki67, and negative for CD10, S-100, and P53.
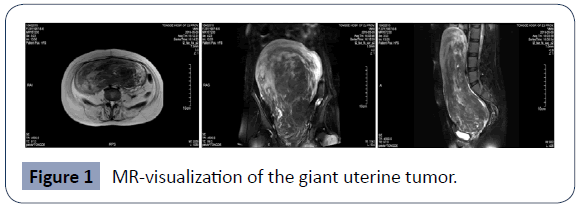
Figure 1 MR-visualization of the giant uterine tumor.
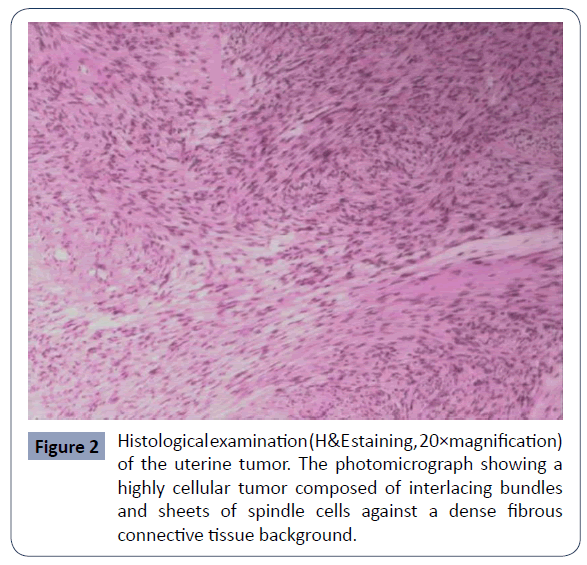
Figure 2 Histological examination (H&E staining, 20×magnification) of the uterine tumor. The photomicrograph showing a highly cellular tumor composed of interlacing bundles and sheets of spindle cells against a dense fibrous connective tissue background.
As the patient suffered from long-term muscular dystrophy, anesthesia and stress during surgery could increase the burdens on the respiratory muscles and even result in paralysis of respiratory muscles and an increased risk of lung infection and heart failure after surgery. Moreover, the patient was at a high risk of poor surgical wound healing, bleeding, and infection, and there was potential for intrapelvic hemorrhage. The patient also was more likely to develop aspiration pneumonia and lower extremity venous thromboembolism than patients with uterine leiomyoma without muscular dystrophy and moderate anemia. Therefore, a tailored nursing care strategy was essential to prevent occurrence of complications and enhance the patient’s ability to engage in self-care.
Post-operative care
General postoperative nursing care such as electrocardiogram monitoring and oxygen administration by nasal cannula were performed. To strengthen the patient’s respiratory capacity, the indoor air, temperature, and humidity of the hospital ward were set at ideal conditions. The patient experienced slight pharyngeal discomfort with coughing with phlegm 3 days after surgery and was treated with budesonide atomization to relieve the symptoms. In order to avoid increasing abdominal pressure after surgery, the abdominal incision was compressed with a sandbag for 6 hours to prevent bleeding and fluidization. The surgical incision healed well without occurrence of infection.
Complementary medical care
A Chinese medicine warm compress and Qihuang pain-relief plaster were used for symptomatic treatment after surgery to boost blood circulation, reduce inflammation, and relieve pain. Jinhuang Ruyi ointment or a Chinese medicine warm compress was applied to the surface of the skin close to the veins during the delivery of intravenousfluid drips of drugs that might cause skin irritation to prevent venous stasis, improve local blood circulation, and relieve muscle spasms. The topical herbal medicine Jiangxia was administrated for preventing vomiting along with acupuncture and abdominal massage, both of which are beneficial for promoting intestinal peristalsis. To prevent deep vein thrombosis of the lower extremities, air pressure therapy for both lower extremities and hot foot baths with Chinese herbal medicines were performed. Traditional Chinese medicine, Houttuyniacordata and Scrophulariaceae, were sprayed to relieve the patient’s throat discomfort after surgery.
Pelvic floor muscle training exercise
Hysterectomy has a significant impact on the patient’s pelvic floor function. The patient received post-operative training in exercises that strengthen the pelvic floor muscles in order to reduce the symptoms of pelvic floor dysfunction caused by surgery.
Psychosocial care
The removal of the whole uterus and the stress caused by the resulting difficulties in post-operative recovery could induce psychological trauma that causes acute stress reactions. Thus, psychosocial care was delivered to the patient along with the cooperation of family members of the patient.
Nursing care provided in response to postoperative complications
Nursing care to prevent aspiration pneumonia: After returning to the ward following surgery, the patient was placed in the supine position with her head tilted to one side to avoid suffocation due to vomiting. The patient was encouraged to practice deep breathing and effective coughing. The patient was assisted to turn over and received gentle pats on the back. The patient’s family members were instructed to gently press the surgical site while the patient was coughing [14].
Nursing care to prevent infection: The patient was at high risk of infection due to the large incision and muscular dystrophy. Antibiotics were given to prevent infection and aseptic procedures were strictly followed by the doctors and nurses.
Nursing care to prevent lower extremity venous thromboembolism: Due to the impact of muscular dystrophy and the limited activities of the lower limb, the patient was at a high risk to develop lower extremity venous thromboembolism. The patient was encouraged to perform appropriate activities with assistance from the family members. Moreover, the patient received lower extremity compressed air massage, traditional Chinese medicine foot bath treatments, and subcutaneous injections of anticoagulants.
Nursing care for urinary retention: Being a long-term bedridden patient, the weak contractions of the patient’s bladder smooth muscle resulted in urinary retention. In addition, removal of the catheter during the application of an analgesic pump could cause hematuria and urinary retention. Therefore, we removed the catheter after using the analgesic pump. The patient did not experience urinary retention during hospitalization.
Outpatient care
Diet: A light, digestible, nutritious diet and a diet for anemia such as astragalus, hen, longan, red dates and red bean soup were suggested for the patient. The patient was told to avoid tobacco, alcohol and a diet containing sea food and other irritating ingredients.
Follow-up examination: A follow-up examination two weeks after discharge from the hospital was performed. Immediate follow-up examination was suggested if the patient experienced high fever, massive vaginal hemorrhage, shock, abnormal discharge or wound swelling, pain, and purulent discharge.
Exercise: The patient was told to take regular exercise and avoid long periods of sedentary behavior.
Sexuality: Sexual life and heavy physical labor cannot be carried out within 3 months after surgery.
Personal hygiene practices: It was suggested to the patient to keep the abdominal incision clean and dry, pay attention to signs and symptoms of infection such as swelling, heat and pain, replace sanitary pads frequently, and change underwear daily to prevent infection.
Clinical outcome
The patient’s condition was significantly improved 16 days after initial hospitalization, and the patient was discharged from the hospital with a high degree of satisfaction.
Discussion
At present, surgical treatment is usually the first choice for patients with symptomatic uterine fibroids. The surgical procedures include laparoscopic myomectomy, transabdominal myomectomy, total laparoscopic hysterectomy, transabdominal hysterectomy, and vaginal hysterectomy. However, those surgical procedures present advantages and disadvantages to patients. For patients with giant uterine fibroids, it is difficult to perform the surgery without a significant risk of relapse. The combined surgical procedures performed on the patient were transabdominal hysterectomy, bilateral salpingectomy, and broad ligament myomectomy. Giant uterine leiomyoma, progressive muscular dystrophy, moderate anemia, and a severe restrictive ventilatory defect in this patient posed a serious challenge for adequate nursing care. To prevent respiratory depression, use of muscle relaxants were minimized in the selection of types of anesthesia during the operation.
Particular attention should be paid to the patients after surgery with regard to infection, aspiration pneumonia, lower extremity venous thromboembolism, pressure ulcers, etc. The patient’s posterior airway was unobstructed during and after the surgery, and there were no complications such as bleeding, venous thrombosis of the lower extremities, and pressure sores during post-operative nursing care. In the past 5 years, the patient relied on care from her family and had to stay in bed for a long periods of time due to the inability to walk normally caused by more than 10-year history of muscular dystrophy. Thus, in addition to the management of disease, it is necessary to take into account the psychological state of the patient and their family over an extended rehabilitation. Indeed, psychosocial care and home care also play an important role in patient recovery. Timely intervention to restore both the patient’s physical and psychological state to an optimal level should be provided during rehabilitation.
In conclusion, tailored post-operative nursing care may have a great impact on reduction of post-operative complications and improvement of clinical outcome.
Funding
This work is supported by the Department of Gynecology, Tonde Hospital of Zhejiang Province, Hangzhou, China.
Conflict of interest
The authors declare no conflict of interest.
34950
References
- Zhang Y, Chen Y, Chen JW, Zhu DH (2005) Altered expression of myostatin gene in the progressive muscular dystrophy patients. J Genet Genomics 32: 779-783.
- Guo X, Wei ZX, Ma Y (2014) Treatment of progressive muscular dystrophy by hyperbaric oxygen adjuvant. Chin J Gerontol 34: 4204-4205.
- Rahimov F, Kunkel LM (2013) Cellular and molecular mechanisms underlying muscular dystrophy. J Cell Biol 201:499-510.
- Turner C, Hilton-Jones D (2014) Myotonic dystrophy: diagnosis, management and new therapies. Curr Opin Neurol 27:599-606.
- He Y, Liu XJ, Lu JC(2014)The effect of open myomectomy and laparoscopic myomectomy on DDI score and prognosis in elderly patients. Chin J Gerontol 10:5.
- Sun J, Bai TM, Yang SF(2016) Comparison of the therapeutic effect of transabdominal or transvaginal extirpation in the treatment of uterine fibroids. Chin J General Practice 14: 615-617.
- Zhang H, Wu YY (2013) Comparison of laparoscopic and open myomectomy. Chin J Minimal Invasive Surg 13:1077-1079.
- Moris D, Vernadakis S (2014) Giant uterine leiomyoma mimicking pregnancy. Mayo Clin Proc 89: e53-54.
- Bartoš V, Korec P, Ficek R (2018) Giant Uterine Leiomyoma in a Young Woman as an Incidental Finding After a Car Accident: a Case Report. ActaMedica61:29-32.
- Lim PT, Tan CH, Chia HL, Phoon J (2018) Management of a giant uterine leiomyoma. BMJ Case Rep 2018: bcr2017224052
- Jones L, Naidoo M, Machado LR, Anthony K (2020) The Duchenne muscular dystrophy gene and cancer. Cell Oncol 11.
- Justice RW, Zilian O, Woods DF, Noll M, Bryant PJ (1999) The Drosophila tumor suppressor gene warts encodes a homolog of human myotonic dystrophy kinase and is required for the control of cell shape and proliferation. Genes Dev 9:534–546.
- Kataoka H, Ueno S (2017) A giant uterine tumor in a woman with myotonic dystrophy. Clinical Case Reports 5: 539-540.
- Ma ZM, Su LY (2014) Nursing care delivery to a patient with breast cancer and progressive progressive muscular dystrophy. Chin J Modern Nursing 20: 1869-1871.