Keywords
Quality; Daily management systems; Huddles; Communication
Background
One of the most successful tactics that has occurred during the recent quality revolution is also one of the simplest – the huddle. Having a defined process for a daily management system by which front line health care providers or leaders come together daily in a brief huddle has been shown to improve communication and coordination amongst teams [1]. Such systems have been shown to help identify abnormal states quickly, empower front-line staff to fix the problems that they can, and for problems that need higher level of attention, promote a more rapid execution of counter-measures [1].
Such management systems or huddle processes are growing more common in medicine and were copied from industrial companies such as Toyota [2-7]. Discussions about improvement in health care systems often focus on creating a change in culture [1-3]. Changing culture is often stressed to be essential for success. However, such a focus often leads to paralysis, as system leaders struggle to figure out how to change culture. Paradoxically, in order to create a culture conducive to improvement and execution, you should not focus on culture change itself but on your daily management process [1,2]. To change culture, you need to change your daily management system – change the expectations of how your leaders lead and how daily escalation and solving of problems occurs [2].
Through trial and error, we are continuously improving daily management processes and how to effectively huddle. In this article, we describe one approach to conducting a Daily Readiness Huddle (DRH) and its essential elements. Those elements include:
• Volume Assessment
• Readiness Assessment
• Problem Accountability System
• Metrics and Goals
Daily readiness huddle (DRH)
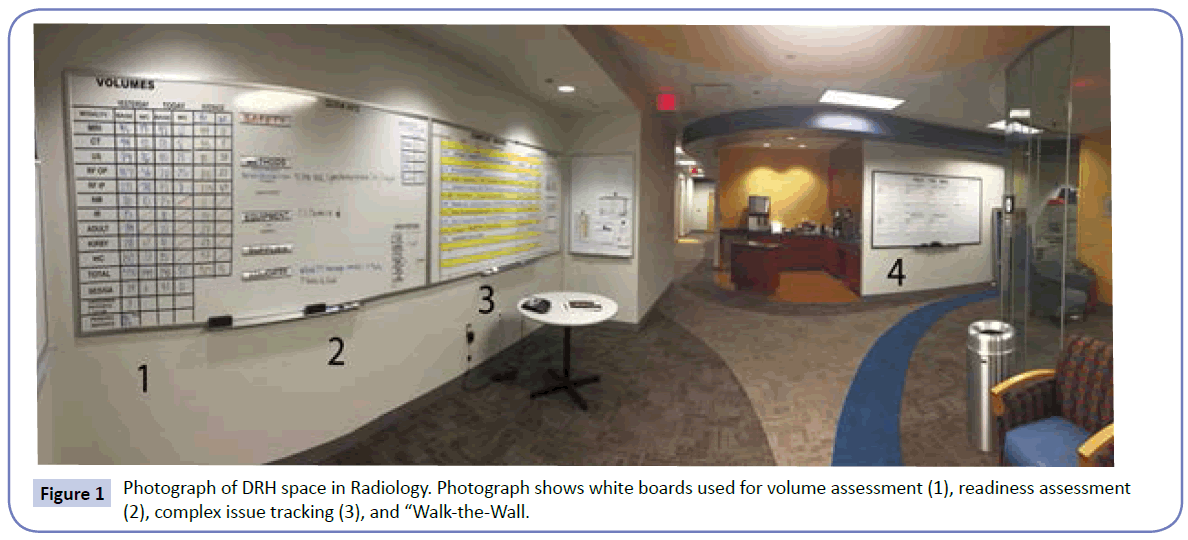
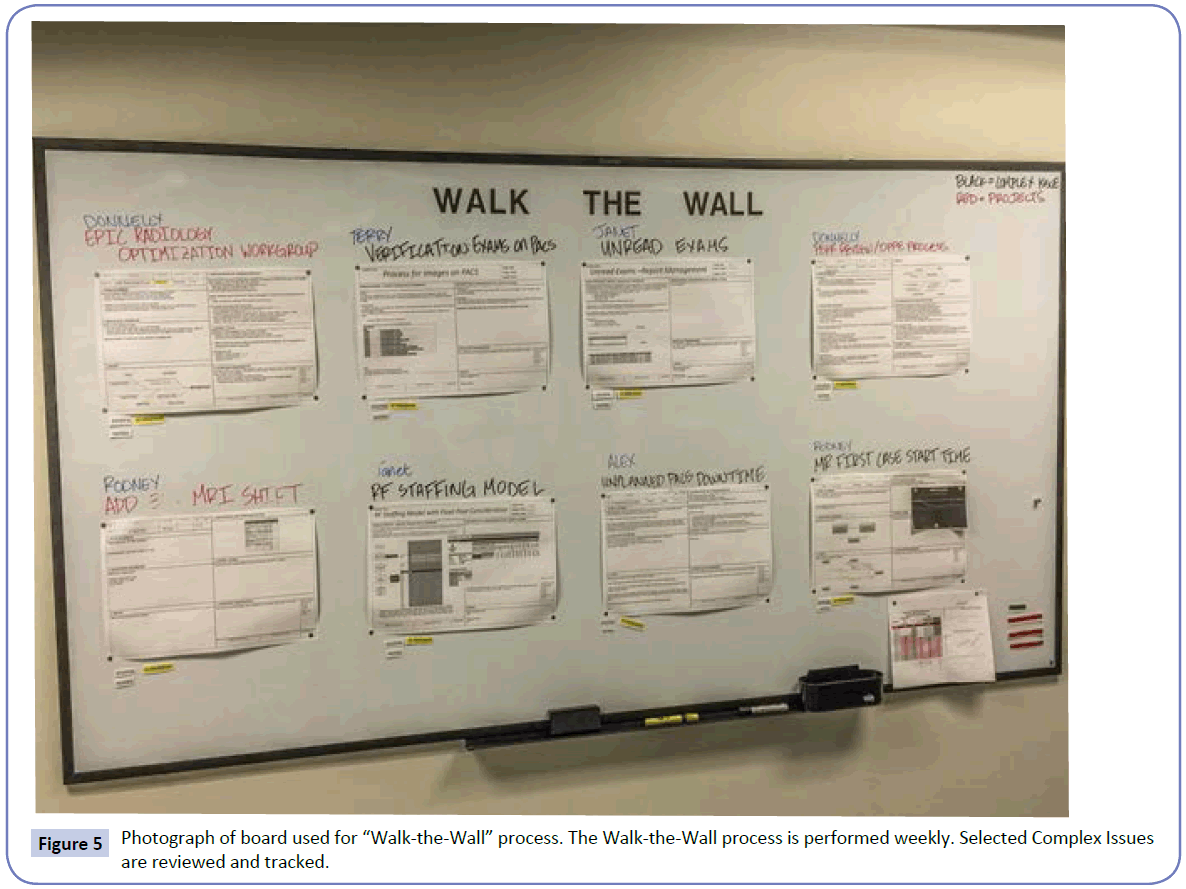
DRHs are a process by which a clinical area, department, or hospital leadership come together on a daily basis and assess their ability to care for the patients they will encounter that day combined with an assessment of any concerns about the delivery of care [1]. Such huddles are short by design and often held with attendees standing to keep the huddle short. They are typically held in an area at or near the care being rendered [1] and are conducted in front of a visual board. Low-tech white boards work exceptionally well for groups that are local and can meet in person (Figure 1). Not only are they inexpensive but the process can easily be adapted and improved when all it takes is an eraser and tape to modify the process. For groups that are meeting across multiple locations, projection of data on electronic documents accessible via a web sharing solution combined with a teleconference can also be effective. Although I would emphasize that when possible, in person processes are the most effective. Even for areas that perform DRH in front of a white board, we do keep electronic documents that track our problem solving performance. Also, an electronic summary of each DRH is sent daily in the form of an email to all associates and physicians in a particular area so that even those who are unable to attend the DRH are aware of the issues discussed. It is optimal to have two people to run a DRH. One acts as the verbal facilitator and one as the scribe or data recorder. It is very difficult for one person to play both roles and have the huddle run efficiently. Because the process has a defined structure, the facilitator role can rotate between leaders and staff attendees.
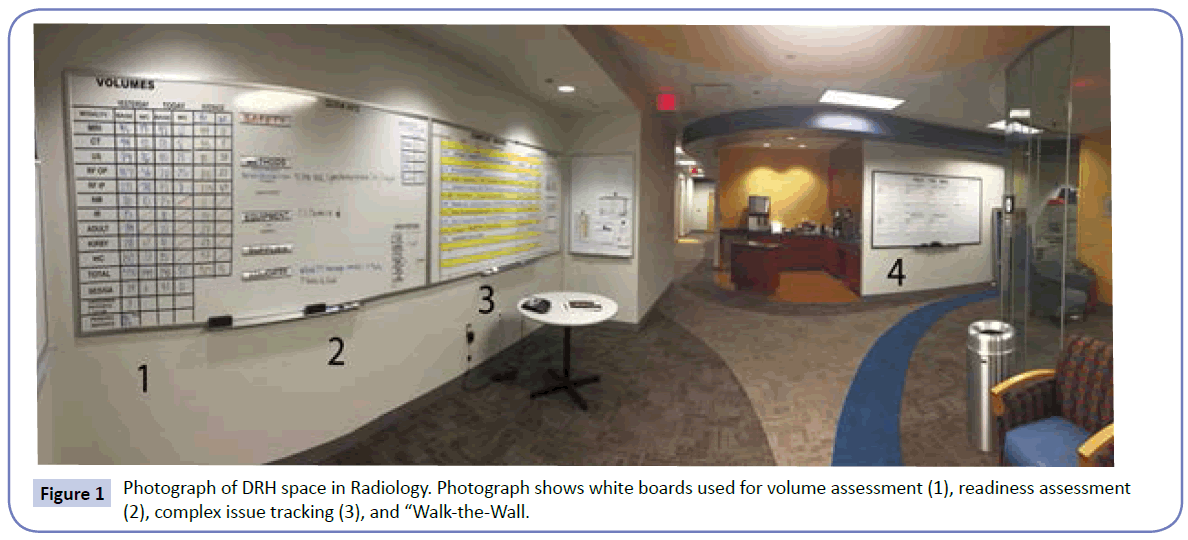
Figure 1: Photograph of DRH space in Radiology. Photograph shows white boards used for volume assessment (1), readiness assessment (2), complex issue tracking (3), and “Walk-the-Wall.
Volume assessment
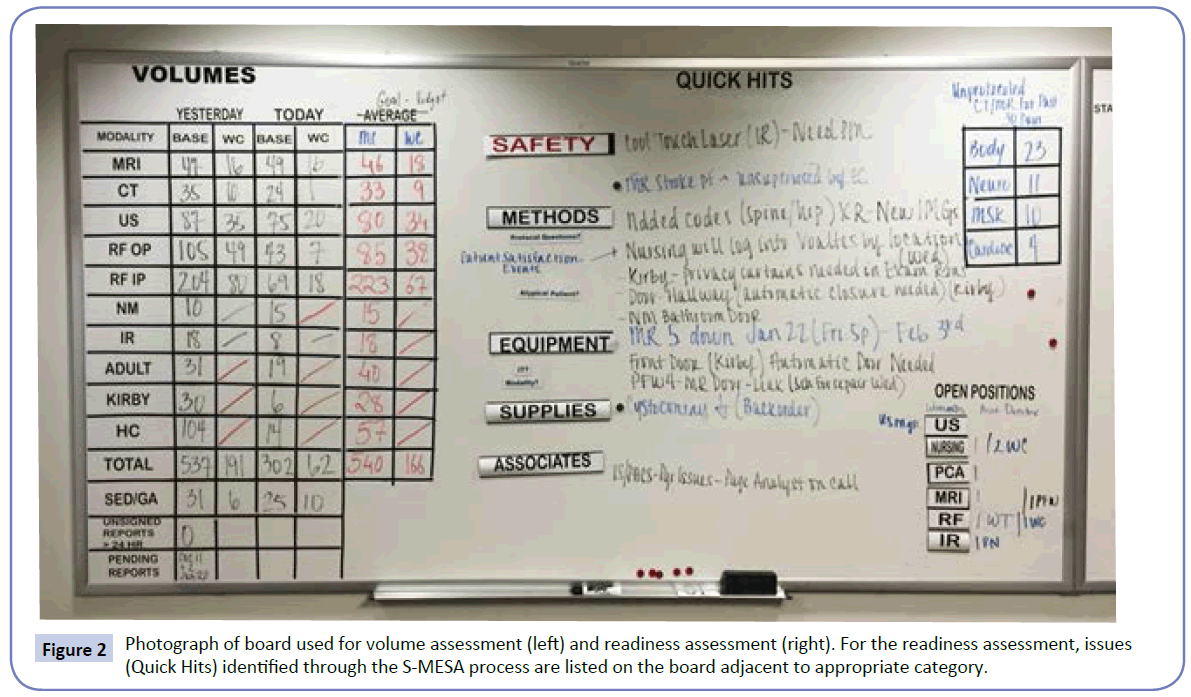
Typically, a DRH will start with an assessment of the volume of activity for the particular area. How this volume of activity is displayed will be very different depending upon the type and scope of work in the area performing the DRH (Figure 2). If the area is an outpatient clinic or department, the number of scheduled visits may be depicted. At a hospital level, the operational capacity, census, and operational variance may be depicted by unit. It is useful to have the operational capacity or average volume, noted adjacent to today’s volume to give context to the values. During this portion of the DRH, the volumes are reviewed and any concerns about those volumes discussed.
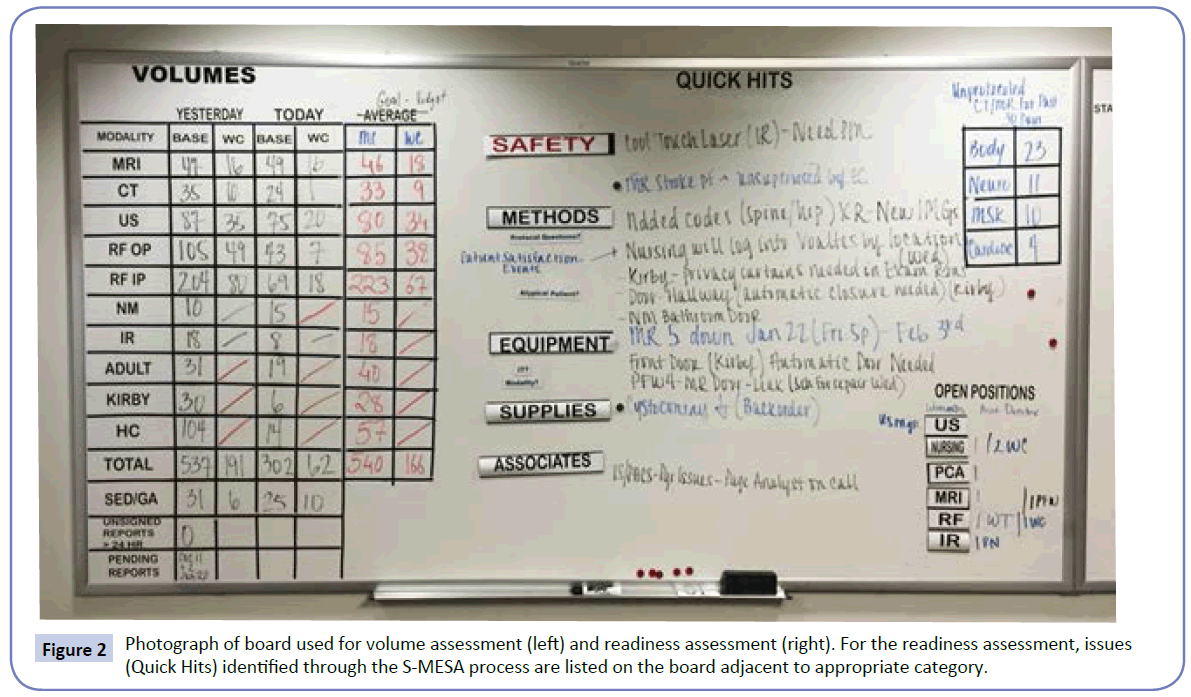
Figure 2: Photograph of board used for volume assessment (left) and readiness assessment (right). For the readiness assessment, issues (Quick Hits) identified through the S-MESA process are listed on the board adjacent to appropriate category.
Readiness assessment
The volume discussion is followed by a readiness assessment. This is typically conduced as a series of prompts designed to encourage attendees to bring up their concerns. It is helpful to have a defined set of prompts that is used daily. One acronym often used is “S-MESA”: Safety, Methods, Equipment, Supplies, Associates [1] (Figure 2). The DRH facilitator moves through the different prompts in a standardized fashion. Methods are an assessment as to whether we have the right protocols and standard work in place to meet the anticipated patient needs. Examples include - Are there any patients with atypical needs or diagnosis that will challenge our standard work and processes? Does anyone have any questions about their assignments and are they clear on the protocols that they are to use for that day? Equipment applies to the assessment as to whether we have the right equipment for that day. Examples include - Are there any atypical equipment needs based on unique patients? Is the equipment operational and working? Does everyone have the appropriate training to operate the equipment that will be needed for that day? Supplies apply to the assessment as to whether we have the right supplies for that day. Examples include - Are there any atypical supply needs based on the scheduled patients? Are there patient needs that may use more than the typical amounts of a standard supply? Do we have any issues with recalls, stock outs, or expired supplies? Associates apply to an assessment as to whether we have the right number and type of associates in place to meet the anticipated patient needs. Examples include - Has anyone called in sick? Based on volumes in particular areas, are we going to have staffing shortages anywhere [1]?
The use of S-MESA works for most clinical or non-clinical support areas. However, other sets of prompts can be uses as well, depending upon the activities and scope of the area. For our institutional DRH which assesses our readiness over a multi-hospital system, we have gravitated to using “SESSFIM”: Safety, Equipment, Supplies, Satisfaction, Facilities, Information Services, and Methods. In a large system, we feel this brings more granularity to the process. We cover staffing during the volume assessment. There are defined prompts under each category. For Safety, enquiries are made as to whether anybody has any patient safety concerns, were there any incident reports of institutional significance, was there any codes or rapid responses conducted and did they go well, were there any employee safety trends or events, were there any new hospital acquired conditions, and are there any other safety concerns? For Equipment, we enquire as to whether anyone has any equipment needs to report or whether biomedical engineering has anything to report. For Supplies, we enquire as to whether anyone has any supply needs to report or whether Supply Chain has anything to report (expired products, delays, dysfunctional products, backorders). For Satisfaction, we enquire as to whether there has been any patient or family satisfaction events or any transfer denials. For Facilities, we enquire as to whether anyone has any facility needs (blocked rooms, out of service elevators, etc) or does Facilities have anything to report. For Information Services, we ask if anyone has any information services needs or whether Information Services has anything to report (downtimes, upgrades, roll outs, etc). Finally, Methods is an additional opportunity to bring up any other issues not yet discussed, issues related to policy or protocol, or issues related to support services: pharmacy, laboratory, respiratory, or imaging issues.
Problem accountability systems
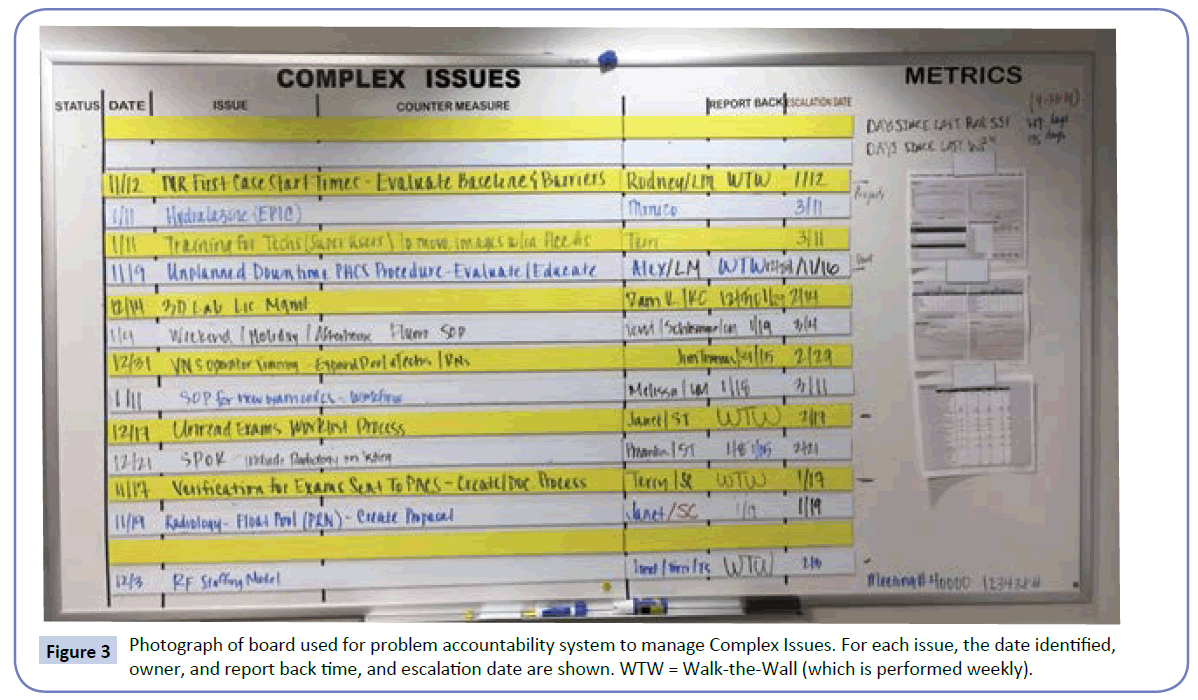
The Readiness Assessment process results in a list of identified issues and concerns. We have come to divide these issues into two groups: Quick Hits and Complex Issues (Figure 3). Quick Hits are defined as issues that are anticipated to be resolved within a short period of time and do not require large amounts of problem analysis or project management. Examples include issues such as a patient room is not available related to a facility issue, a particular supply is on back order, or an operating room sterilizer is not working. Complex Issues are defined as identified problems that often will take a longer period of time and would benefit from project management. Often these issues involve consensus building around a particular standard operating procedure or often changes in information technology systems or space (facility) alterations. Examples would include changes that need to be made to the admission or discharge processes or a change in use of space to expedite patient flow [1]. An identified issue may clearly be a Complex Issue when it is initially identified or may start as a perceived Quick Hit that lingers, does not resolve, and gets re-defined as a Complex Issue. What the appropriate amount of time permitted for resolution of a Quick Hit may vary by the nature of the area. Some of our front line areas use 24-48 hours as the cut off where as our institutional process uses 1-2 weeks.
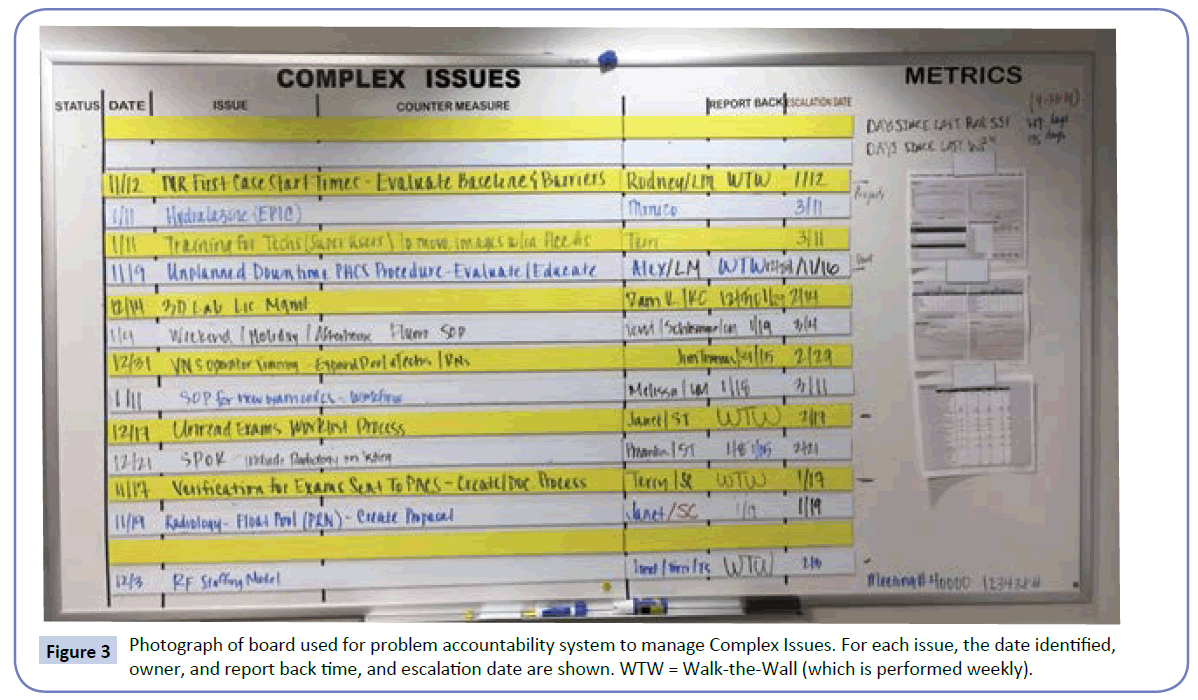
Figure 3: Photograph of board used for problem accountability system to manage Complex Issues. For each issue, the date identified, owner, and report back time, and escalation date are shown. WTW = Walk-the-Wall (which is performed weekly).
For each issue on the complex issues board, the following parameters are defined: the nature of the issue, a defined owner of the issue, a defined quality specialist assigned to the issues, the date the issues was first identified, and the date that the owner is to report back on the progress [1]. Clear communication and expectation setting around defining the problem, countermeasures, timeline, and ownership are key to the accountability cycle for problem solving [1,2,6].
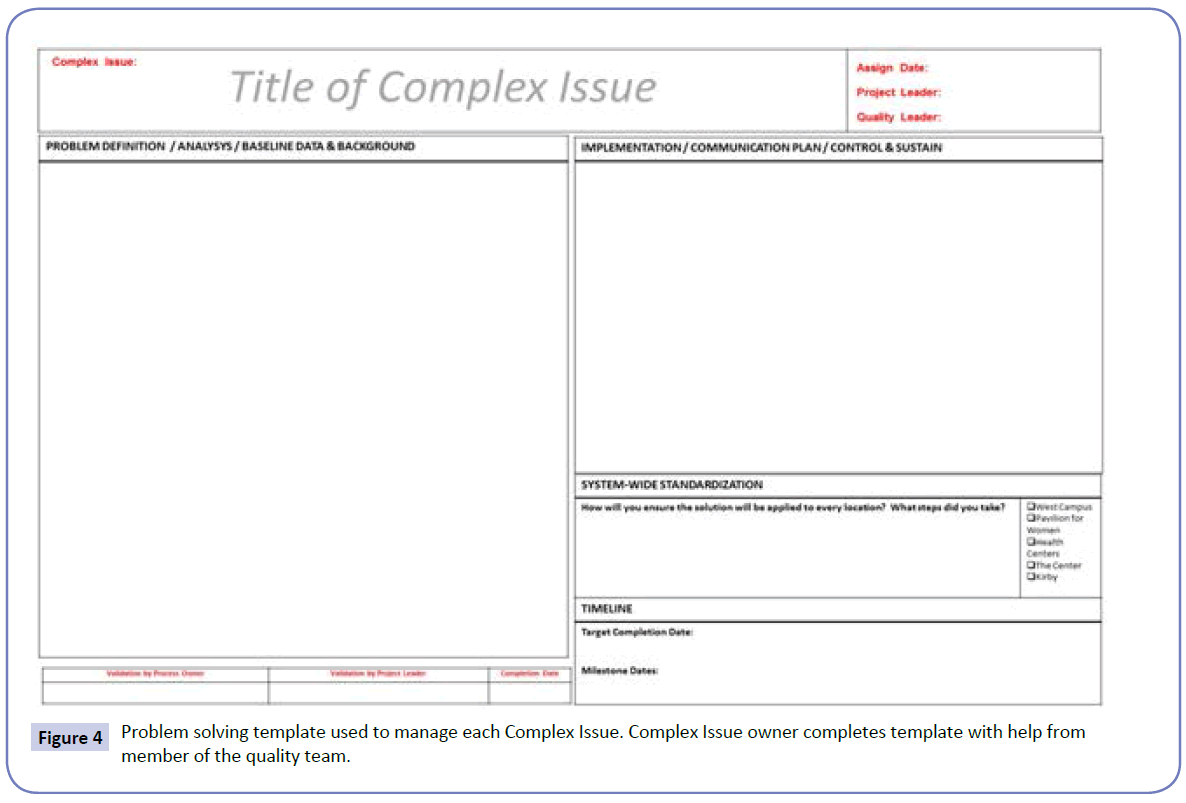
For each Complex Issue, we ask the owner to use a defined problem solving template (Figure 4). That template helps the team working on the issue with tasks such as defining the problem, analysis, baseline data or background, implementation, communication plan, sustainability, system-wide implications and standardization, and project timeline definition. We have found that use of a standardized template and approach to problem solving has helped our team both improve our problem solving abilities as well as helped with the presentation of plans back to our group. The project template has undergone a number of iterations based on both user feedback as well as analysis of our more common failures. Many of our failure points have been related to a lack of adequate communication around the agreed upon solution to the Complex Issue, such as a communication about a new or revised standard operating procedure. Many of our other failures result from fixing the issue at one location but failing to spread that success to other parts of the organization. This lead to sections of the template being dedicated to the communication plan as well as for system-wide standardization.
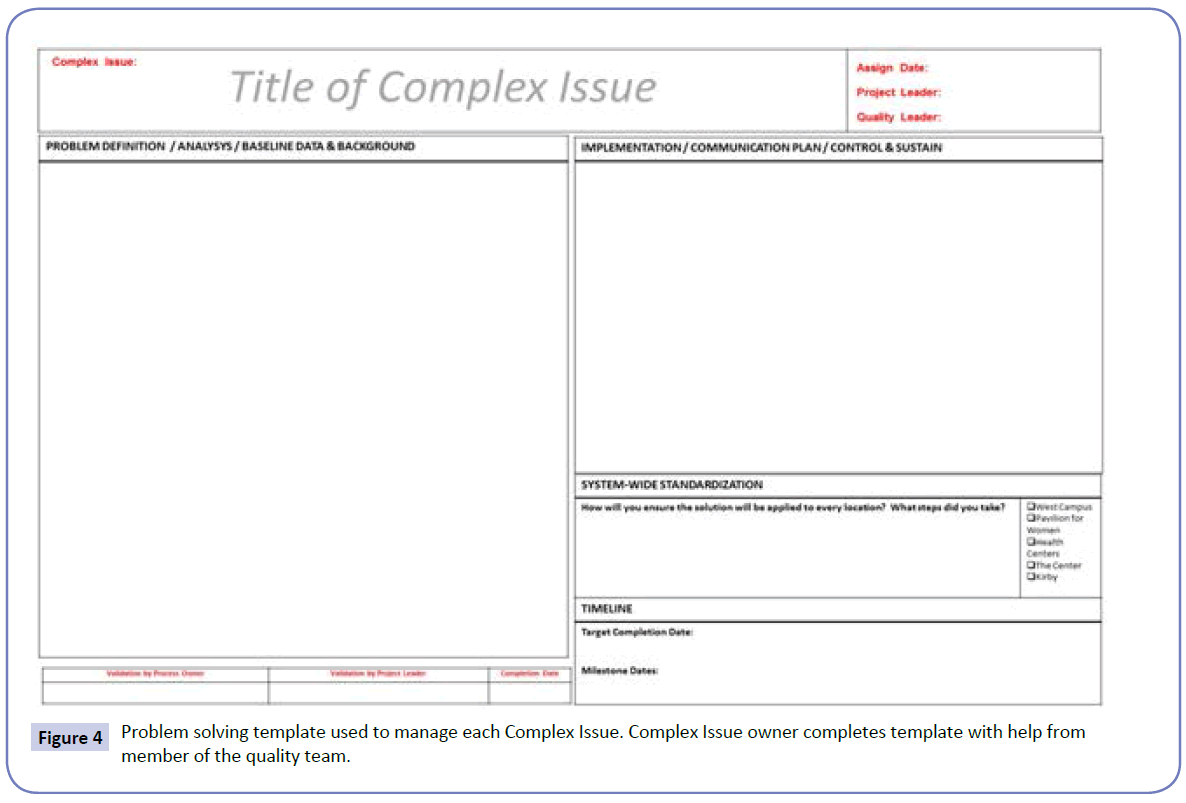
Figure 4: Problem solving template used to manage each Complex Issue. Complex Issue owner completes template with help from member of the quality team.
The owner of the Complex Issue choices the date for which they are to report back based on the nature of the problem. If the Complex Issue is not completed within a defined 60 day period, the Complex Issue is escalated and presented to a leadership group. The escalation date servers several purposes. First, it defines a process to bring in additional leaders to evaluate the issue, prioritize, and potentially bring further resources or support to help solve the problem. These issues are complex by definition and some do need additional resourcing. Second, none of the Complex Issue owners want to have their issue escalated and presented before a leadership group so the escalation date helps to drive projects to fruition.
One of the issues with which we have sometimes struggled is creating enough time to discuss some of these very Complex Issues in the detail needed at a DRH that is designed to last only 15- 20 minutes in total. Related to this we have created an additions process, adapted from a process which we saw presented from another institution, which we refer to as “Walk-the-Wall”. We have an additional board on which a defined number of Complex Issues are highlighted (Figure 5). On this board, the completed problem solving templates of the highlighted Complex Issues are displayed. One day per week, following the DRH, we spend an additional 30 minutes performing a “Walk-the-Wall” review of the featured Complex Issues. Typically, there are more Complex Issues than can be featured on the Walk-the-Wall board and we choice which ones to highlight based on the acuity of the problem as well as the need for attention and project management based on the nature of the issue and the experience of the team working on it.
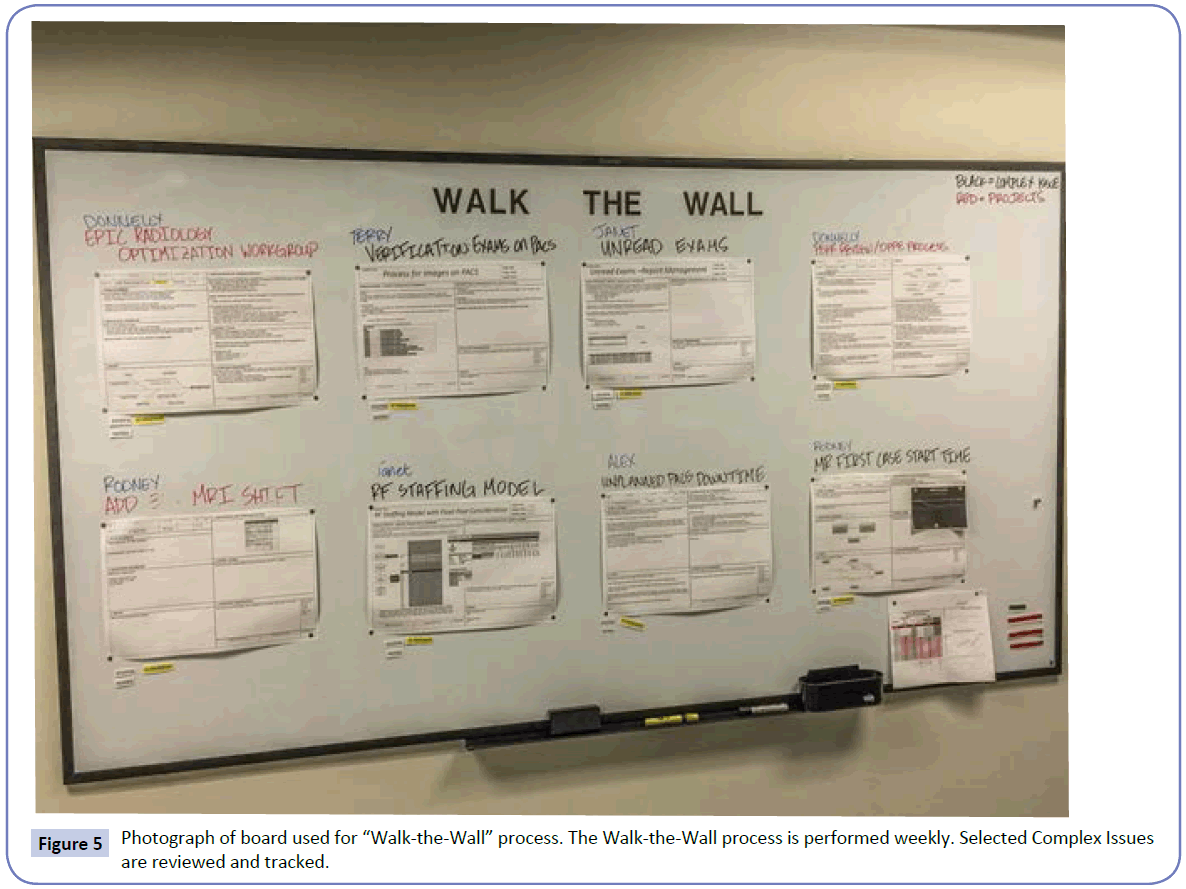
Figure 5: Photograph of board used for “Walk-the-Wallâ€Â process. The Walk-the-Wall process is performed weekly. Selected Complex Issues are reviewed and tracked.
Metrics and goals
Transparent display of data helps drive high performance [8-11]. Such data can be displayed in the format of a balanced scorecard [8-11]. The goal is to help align performance measures with strategy [8-11]. In healthcare, such scorecards reflect institutional strategic areas such as customer satisfaction, quality and safety, finance, research, education, and people [10]. It can service as a powerful tool. You tend to get what you measure [10]. We have incorporated aspects of a balanced scorecard into our huddle process.
Our areas display their score cards as part of their DRH visual boards. Many of these metrics are updated monthly and reviewed accordingly. Some metrics are updated daily (days since last serious safety event in the unit, days since last wrong patient/ wrong procedure event, etc).
Summary
In summary, we have found that having a defined DRH process has greatly increases our ability to rapidly identify and solve problems. It has also helped with team-building and improved coordination of our medical services. This is related to both the formal aspect of the DRH as well as the informal aspect. When you know that there is a defined portion of the day at which you are going to see all of the people that you might need to coordinate, it helps both with coordination as well as elimination of the rumor mill. We have also found that running an area via this process helps unite those with roles primarily in operations with those with roles primarily in quality and safety as one coherent team as opposed to two separate entities. This has been a critical aspect to optimizing our performance. We have found this process helpful at both the unit and institutional levels.
8446
References
- Donnelly LF (2014) Daily Management Systems in Medicine.Radiographics 44: 1209-1212.
- Mann D (2010) Creating a Lean Culture – Tools to Sustain Lean Conversions, 2nd Ed.Boca Raton, FL: CRC Press 3: 103.
- Liker JK, Convis GL (2012) The Toyota way to lean leadership – Achieving and sustaining excellence through leadership development. McGraw Hill 121-143.
- Koenigsaecker G (2009) Leading the lean enterprise transformation.Boca Raton, FL: CRC Press 9-77.
- Liker JK (2004) The Toyota way.14 Management principles form the world’s greatest manufacturer 1-159.
- Bussell J (2012) Anatomy of a lean leader as illustrated by 10 modern CEOs and Abraham Lincoln.Northbrook, IL; UL LLC 1-150.
- Toussaint J, Gerard RA (2010) On the mend.Revolutionizing healthcare to save lives and transform the industry.Cambridge, MA: Lean Enterprise Institute 1-138.
- Kaplan RS, Norton DP (1992) The balanced scorecard measures that drive performance.Harv Bus Rev 70: 71-79.
- Zelman WN, Pink GH, Matthias CB (2003) Use of a balanced scorecard in health care.J Health Care Finance 29:1-16.
- Donnelly LF, Gessner KE, Dickerson JM, Lehkamp TW, Moskovitz J, et al. (2010) Department Scorecard - A Tool to Help Drive Imaging Delivery Performance.RadioGraphics30:2029-2038.
- Johnson CD, Krecke KN, Miranda R, Roberts CC, Denham C (2009) Developing a Radiology Quality and Safety Program:A Primer. Radiograp hics29:951-959.