Keywords
Stroke; Physiotherapy; Aged; Psychomotor performance
Introduction
Stroke is caused by a dysfunction of the blood supply to the brain [1]. It represents a group of diseases with similar clinical manifestations, but has some subdivisions: hemorrhagic, which is conceptualized as rupture of a cerebral blood vessel; and ischemic that presents as occlusion of the blood circulation [2].
It is characterized by sensory, motor and cognitive-perceptive alterations that result in functional limitation or disability with consequent interference in the Activities of Daily Living (ADL) and restrictions in social participation, with loss of autonomy and independence [3]. Depending on the extent of the injury and the brain affected area, about ninety percent of people can present hemiparesis or hemiplegia on the contralateral side of the injury. Major impairments in patients include lack of balance, altered mobility, sensory, cognitive, perceptual, and language deficits [4].
However, dysfunctions resulting from stroke can be reduced by aquatic therapy. This intervention uses the physical properties of water to help adjust muscle spasticity, relieve joint overload, stretch soft tissues, improve venous return, and facilitate controlled movements [5]. In addition, it enables the experience of treatment in a differentiated environment and influences the individual's behavior, as it increases their confidence and self-esteem [6].
Furthermore, psychomotricity is a recent science, with the purpose of promoting the interaction of the individual with the space through body practice and its expressiveness. It is possible to observe fundamental psychomotor elements such as: body scheme, body image, tonus, balance, global motor coordination, fine motor skills, spatial-temporal organization, rhythm, laterality, and breathing [7]. Not only the body will be in movement, but also the brain and the soul, working the physical, social, biological and emotional resourcefulness [8].
Aquatic Psychomotricity promotes a comprehensive therapeutic approach, since it helps in the rehabilitation of various motor symptoms, taking advantage of the properties of water. The psychomotor activities used in this medium help in rehabilitation by facilitating or creating resistance in the execution of movements, without the need for specific equipment. Thus, the principles of psychomotricity in the aquatic environment broaden functional improvements and stimulate psycho-emotional reactions [9].
Therefore, considering the return of functionality in this individual with stroke sequels and the need for a deeper approach on the subject, this study proposed to verify the effects of aquatic psychomotricity on psychomotor and mental factors in elderly people with stroke sequels.
Materials and Methods
The longitudinal research, with a descriptive and quantitative approach, developed in the therapeutic swimming pool of the Teaching and Assistance Unit of Physical Therapy and Occupational Therapy began after approval by the Research Ethics Committee of the Center for Biological Sciences and Health of the Pará State University, with opinion number 4,359,488 and signing of the consent form by the participants or legal guardians.
The research sample was selected by convenience and composed of twenty-one elderly people, considering as inclusion criteria both genders, aged between 60 and 75 years, patient of UEAFTO, individuals with stroke sequels from the 3rd month after diagnosis, with hemiparesis, those who use wheelchairs for locomotion, but who were able to stand up and/or walk with help and who agreed to participate in the research by signing the Informed Consent Form.
Excluded were individuals with mental and cognitive impairment (Mini Mental State Examination less than 20) that interfered with the understanding of simple commands, as well as elderly individuals with uncontrolled hypertension, dermatological alterations, infected open wounds, acute illnesses, severe respiratory failure, otitis, infection and urinary incontinence.
After screening, a form was applied with personal identification and socioeconomic aspects, prepared by the researchers. Besides the evaluation by means of the Gerontopsychomotor Observation Scale, developed with the purpose of tracing the psychomotor profile of the individuals, by means of aspects related to psychomotricity, cognition, and language, the social-affective relationship, and autonomy in the activities of daily living, which is classified as: 0-Behavior not observed or not applicable (NA); 1-Does not do/does not present; 2-Does with great difficulty/ Rarely presents; 3-Does with some difficulty/Sometimes presents; 4-Does without difficulty/Presents frequently [10].
Another scale used was the Performance Scale, which more simply and effectively assesses the participants' performance in the sessions. Each task is given a score from 0 to 8, rating the type of help in the sessions, where 8=no help; 7=some help; 6=verbal help; 5=demonstrations; 4,3 and 2=physical help; 1=does not do; 0=not applicable [10].
For the psychomotor intervention in aquatic ambient, in a heated pool with an average temperature of 35º C, 12 dynamics containing individual tasks for self-knowledge (straight line, race on the board, statue of liberty, sea horse, target shooting, the tightrope walker) and in groups (follow the master swimmer, circuit, basketball, frog pond, bladder dance, water mirror) were developed for socialization. These dynamics contemplate the psychomotor elements of body scheme, tonus, balance, global motor coordination, fine motor skills, spatial and temporal organization, rhythm, laterality, and breathing, and for their applicability, materials such as balls, boards, bladders, hula hoops, aquatube, and dumbbells were used.
Each session was composed of 10 minutes of adaptation in the aquatic environment, with a water walk associated with breathing and concentration on the body itself, then 20 minutes for two psychomotor dynamics, and at the end between 10 and 15 minutes of relaxation with hydro-massage, in which floats were placed on the volunteers, making them comfortable and safe. The choice of tasks was made by the researchers and consisted of 1st session: Straight Line and Target Shooting; 2nd session: Seahorse and Statue; 3rd session: Circuit and Water Mirror; 4th session: Bladder Dance and Balancer; 5th session: Basketball and Frog Pond; 6th session: Race on the Board and Follow the Swimmer; 7th session: Target Shooting and Seahorse; 8th session: Straight Line and Water Mirror.
The software Excel® 2010 was used for data entry and preparation of tables. Descriptive analysis and data distribution were performed using RStudio® software, and the Shapiro Wilk test was applied to analyze data normality. Then, the existence of a statistically significant difference between the beginning and end of the intervention was evaluated using the analysis of variance test at an alpha level of significance of 5% (p ≤ 0.05), using the BioEstat® 5.3 program for comparison. For further evaluation, the performance of each block was presented as a function of the mean variables through graphical analysis.
Results
Twenty-one volunteers were selected. 61.90% were male, 76.19% self-declared brown, 85.71% diagnosed with ischemic stroke, mean age 66.19 years, according to table 1. Regarding occupation, it was observed that most participants were retired people (61.90%) (Table 1).
| Variables |
N |
Percentage (%) |
| Age group |
| 60-65 |
13 |
61.90 |
| 66-75 |
8 |
38.10 |
| Gender |
| Male |
13 |
61.90 |
| Female |
8 |
38.10 |
| Ethnicity |
| Black |
3 |
14.29 |
| Brown |
16 |
76.19 |
| White |
2 |
9.52 |
| Diagnostic |
| Ischemic stroke |
18 |
85.71 |
| Hemorrhagic stroke |
2 |
9.52 |
| Ichemic and hemorrhagic stroke |
1 |
4.76 |
Table 1 Distribution of absolute and relative frequency for the participants' profile.
The mean and standard deviation of the score obtained in each domain of the Psychomotor Observation Scale, in both evaluations, are shown in Table 2. Comparing the pre and post aquatic psychomotor intervention results, significant improvements were found in all variables, with p ≤ 0.05 (Table 2).
| Variables |
Initial |
Final |
p-value |
| Mean ± SD |
Mean ± SD |
| Attention |
3.24 ± 0.89 |
3.86 ± 0.36 |
< 0.0001* |
| Manual Coordination |
6.14 ± 1.80 |
7.57 ± 0.75 |
< 0.0001* |
| Podalic Coordination |
6.33 ± 1.28 |
7.67 ± 0.86 |
< 0.0001* |
| Spatial-temporal structure |
14.52 ± 3.20 |
15.67 ± 0.97 |
< 0.0001* |
| Temporal orientation |
6.43 ± 1.29 |
7.52 ± 0.75 |
< 0.0001* |
| Spatial Orientation |
13.10 ± 3.08 |
14.71 ± 2.26 |
< 0.0001* |
| Global Praxis |
8.14 ± 2.22 |
10.86 ± 1.35 |
< 0.0001* |
| Fine Praxis |
28.33 ± 7.19 |
32.24 ± 4.47 |
< 0.0001* |
| Body notions |
14.43 ± 2.93 |
15.43 ± 2.04 |
0.0002* |
| Laterality |
7.24 ± 1.26 |
7.76 ± 0.54 |
< 0.0001* |
| Tonicity |
33.43 ± 9.62 |
35.67 ± 9.16 |
< 0.0001* |
| Balance |
15.90 ± 3.52 |
18.38 ± 2.56 |
< 0.0001* |
*Significant difference (p ≤ 0.05)
Table 2 Analysis of the mean ± standard deviation (SD) referring to the psychomotor elements.
In table 3, the comparison between pre- and post-intervention in relation to language and cognition showed that the group obtained significant improvements in all variables except short-term memory (Table 3).
| |
Initial |
Final |
|
| Variables |
Mean ± SD |
Mean ± SD |
p-value |
| Activity of Daily Living |
20.05 ± 3.85 |
22.33 ± 2.99 |
< 0.0001* |
| Non-Verbal Language |
13.81 ± 2.34 |
15.05 ± 1.32 |
< 0.0001* |
| Verbal Language |
26.43 ± 5.90 |
28.95 ± 4.27 |
< 0.0001* |
| Short-term memory |
10.19 ± 2.96 |
10.29 ± 3.02 |
0.0797 |
| Long-Term Memory |
9.81 ± 3.22 |
10.76 ± 3.05 |
< 0.0001* |
| Social Affectivity |
30.38 ± 6.08 |
33.24 ± 3.71 |
< 0.0001* |
| Other |
20.00 ± 5.24 |
21.10 ± 4.00 |
< 0.0001* |
*Significant difference (p ≤ 0.05)
Table 3 Mean value ± standard deviation referring to the cognition and language domains.
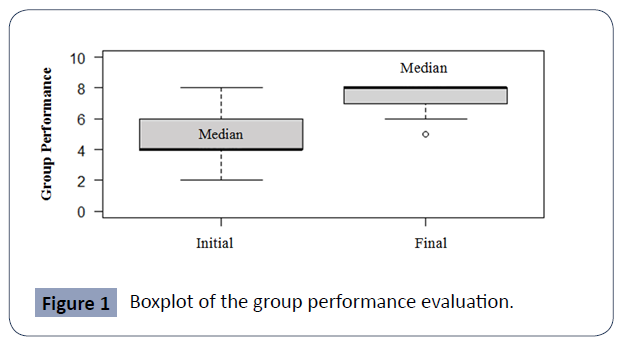
This research used the Psychomotricity Session Performance Evaluation Scale to quantify the evolution of patients during the treatment. Graphic 1 illustrates, by means of boxplot, the comparison of the group's performance at the beginning and after of the psychomotor treatment. It shows that at the end, the median score predominated between 7 and 8, indicating that in the last session the volunteers were able to perform the activities independently, without any help (Figure 1).
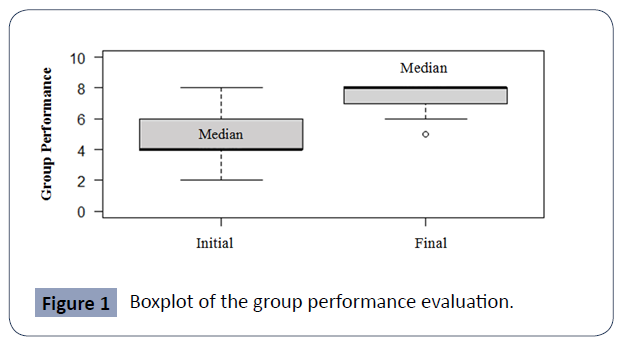
Figure 1 Boxplot of the group performance evaluation.
Discussion
In this study, it was possible to observe agreement with the literature on the epidemiological profile of individuals affected by stroke. Guziki and Bushnell [11] conducted an epidemiological survey in the United States, showing a higher incidence in blacks than in whites and that men are more affected when compared to women, both young and middle-aged. Medeiros et al [12], when performing the self-reported evaluation of ethnicity, concluded that brown was the most commonly reported, and also demonstrated the high prevalence of ischemic stroke.
Individuals with this pathology can present cognitive sequels and consequently losses in executive function, such as the ability to planning and attention. Pereira et al [13] conducted a pilot study of a multimodal exercise program and obtained improvements in relation to selective and sustained attention, with greater concentration of the volunteers. In the present analysis, cognitive training had not been performed to cover the participants' attention-related limitations; however, psychomotor tasks maintained the function, avoiding progressive losses.
Regarding muscle tone, Matsumoto [14] emphasizes that exercises performed in immersion in hot water for 10-15 minutes can relief spasticity in post-stroke patients, especially in the lower extremities, without triggering adverse effects. The therapy enabled the relief of muscle hypertonia in both the upper and lower limbs, since the psychomotor tasks, which aim to preserve tonus, were associated with the benefits of thermotherapy, when the exercises were performed with the limbs submerged.
In the meta-analysis formulated by Naiak et al [15], it was found that aquatic therapy improves the balance of these individuals when administered alone, and also promotes benefits when worked in a complementary manner with conventional therapy. Furthermore, he emphasized that the study parameters in most therapies are 0-60 minutes of intervention, 3-5 sessions per week for 8 weeks. However, it is possible to realize the viability of the psychomotricity protocol in the aquatic environment in relation to balance, in only 2 sessions per week during 4 weeks, maintaining the time of 60 minutes.
The notion of body results from its interaction with the environment, therefore, the sudden changes that occur after the stroke can be an influencing factor in the body scheme and body image. For Sadanandan et al [16] and Timothy et al [17], in fact, those affected by this pathology experience disturbances in the perception of body image and this results in dissatisfaction with life, anxiety, and negative emotions. Data analysis and the participants' reports showed that the psychomotor intervention promoted the redefinition of self-identity and acceptance, which facilitated the way of dealing with the disease and rehabilitation.
The individual has the ability to situate himself in relation to the succession and in function of the diverse events, the variation of periods in an inconvertible form of time [18]. According to the classic by Le Boulch [19], this structure can be dictated by the dynamic and rhythmic way that the human being experiences his existence, at this point, even the use of music is an important factor for development and rehabilitation [20]. At the time of treatment, such a resource was used to stimulate the creativity, imagination, and learning of the elderly and consequently obtain the results for temporal structuring.
Spatial orientation declines during the aging process of all individuals and the impoverishment of this domain leads to difficulties in displacement, especially in different spaces of everyday life [21]. It was observed in this research that among the psychomotor aspects, spatial orientation was one of those that obtained a difference between the initial and final evaluation, although it is a variable that needs more time to obtain better results; however, it achieved the goal of preserving existing functions and preventing psychomotor retrogenesis processes.
Motor incoordination after stroke produces significant disabilities that affect the activities of daily living and consequently the quality of life. At the beginning of the treatment, the execution and automation of movements, of most volunteers, was performed in a non-integrated manner. In the elaborate program of psychomotor activities, it was essential to perform bilateral exercises of both the upper and lower limbs, because according to Kantak et al [22] and Menezes et al [23] for rehabilitation practice it is essential to incorporate coordination in a globalized manner, and thus obtain a full functional recovery.
In addition, there are also fine motor deficiencies, mainly in grip strength, motor coordination, and movement speed, since they also have altered tactile sensitivity, making it difficult to apply adequate force for manual skills tasks [24]. The psychomotor intervention allowed for a statistically significant improvement in the participants' fine praxis, especially in the palmar grip strength of the paretic hand, when using aquatubes, balls, and bladders of different sizes in most activities, in addition to motor coordination when manipulating objects.
The ability to communicate for those who have been affected by the pathology is crucial, because when done effectively it facilitates the daily life of the individual and their caregivers. It is important to go beyond verbal language factors, since non-verbal skills play an indispensable role in the transmission of a given message [25]. In the interventions of this protocol, more than one measure was used to capture the skills of a functional communication, aiming as therapeutic focus the spoken participation activities and those performed with gestures, facial expressions, and with the gaze.
In the studies by Osorio-Valencia et al [26] conducted with preschool children at age 3 and later at age 5, it was realized that psychomotricity is important for the development of motor and cognitive skills, including memory. With this, stimulation helps to create neuronal networks that facilitate the acquisition of these skills from childhood. In the elderly with stroke, the induction of a plastic state can occur through neurorehabilitation and the behavioral activity of the recovering circuits, but it was observed significantly in the present study in relation to long-term memory, but not short-term [27].
The psychomotor protocol in the aquatic environment, especially the exercises performed in groups, can contribute to the improvement of the social-affective relationship of the elderly, given that at the end of the treatment there was greater interaction among participants, influencing a better acceptance of the therapy, which resulted in a statistically significant difference in this aspect. Mosor et al [28] conducted an intergenerational intervention program based on psychomotor activity and did not obtain satisfactory statistics, however, the qualitative evaluation of the process showed the satisfaction of the elderly, through positive reports of the experience and it was also possible to observe engaged and happy facial expressions, which promotes greater well-being.
The altered movement patterns in hemiparetic patients caused by spasticity, the onset of tonic reflex activity, cognitive decline, and sensory disorders can influence the mobility, quality of life, and performance of daily life activities of these individuals [29]. Thus, by using psychomotricity associated with the physical properties of water, it allowed the execution of movements that were difficult to perform on land, as observed in this research, considering that the participants, by integrating psychomotor aspects in the aquatic environment, obtained greater independence in activities of daily living.
When analyzing the data, it was concluded that during the sessions there was a relevant improvement in relation to the participants' performance since the first evaluation. According to Stinear et al [30], several large intervention studies aimed at motor recovery reported that the motor performance of participants improved after treatment, but to a similar degree for intervention and control groups in most studies. Although the research did not have a control group for a better comparison, only psychomotor rehabilitation allowed that in the final evaluation the individuals were more independent in their activities, needing little or no help from another person.
Conflict of Interest
There is no conflict of interest regarding the manuscript or the materials of this study.
Conclusion
Aquatic psychomotricity, as a therapy involving body and mind, allowed an improvement in psychomotor aspects. In this context, the practice proved to be effective both for proposing movement and its facilitation, as well as for cognitive skills and social interaction. The research in question contributed as an enriching source of knowledge and techniques for professional learning. Thus, incentives in the literature on the theme are still necessary to enrich the content and promote experiences that contribute to the physical and social well-being during stroke rehabilitation.
40204
References
- Lopes J, Sanchis GJB, de Medeiros JLA, Dantas FG (2016) Hospitalization for ischemic stroke in Brazil: an ecological study on the possible impact of Hiperdia. Rev bras Epidemiol 19.
- Dutra MOM, Coura AS, França ISX, Enders BC, Rocha MA, et al. (2017) Sociodemographic factors and functional capacity of elderly people with stroke. Rev Bras Epidemio 20: 124-135.
- Silva SM, Corrêa JCF, Pereira GS, Corrêa FI (2019) Social participation following a stroke: an assessment in accordance with the international classification of functioning, disability and health. Disabil Rehabil 49: 879-886.
- Darekar A, Mcfadyen B, Lamontagne A, Fung J (2015) Efficacy of virtual reality-based intervention on balance and mobility disorders post-stroke: a scoping review. J Neuroeng Rehabil 12: 46.
- da Costa MRDV, de Lima RC, Lopes CP, Shirahige L, Albuquerque PL (2017) Effect of hydrotherapy on cardiovascular conditioning and quality of life in patients after stroke. Conscientiae saúde 16.
- Assis F, Raimundo R, Lima K (2019) The importance of aquatic physiotherapy for the elderly. E-Revista pp: 1981-3511.
- de Oliveira RV, Foresti BB, de Carvalho PK, Alves FRR (2017) Psychomotricity as an intervention method for the elderly. Revista UIIPS 5: 135-140.
- Fernandes JMGA, Filho PJBG, de Rezende ALG (2018) Psychomotricity, game and body-in-relation: contributions to intervention. Cad Bras Ter Ocup 23: 702-709.
- dos Santos SL, Soares MJGO, Ravagni E, Costa MML, Fernandes MGM (2014) Walking performance of elderly practitioners of psychomotricity. Rev Br Enf 67: 617-622.
- Freitas MM (2017) Psychomotricity in the Senior Neurological Campus - implementation of a psychomotor program in neurodegenerative diseases. ULisboa.
- Guzik A, Bushnell C (2017) Stroke epidemiology and risk factor management. Continuum (Minneap Minn) 23: 15-39.
- de Medeiros CSP, da Silva OAP, de Araújo UB, de Souza DE, Cacho EWA, et al. (2017) Social and Functional Profile of Userswith Stroke Assisted by the Family Health Strategy. Rev Bras Cienc Saud 21: 211-220.
- Pereira C, Rosado H, Cruz-Ferreira A, Marmeleira J (2018) Effects of a 10-week multimodal exercise program on physical and cognitive function of nursing home residents: a psychomotor intervention pilot study. Aging Clin Exp Res 30: 471-479.
- Matsumoto S, Uema T, Ikeda K, Miyara K, Nishi T, et al. (2016) Effect of Underwater Exercise on Lower-Extremity Function and Quality of Life in Post-Stroke Patients: A Pilot Controlled Clinical Trial. J Altern Complement Med 22: 635-41.
- Nayak P, Mahmood A, Natarajan M, Hombali A, Prashanth CG, et al. (2020) Effect of aquatic therapy on balance and gait in stroke survivors: A systematic review and meta-analysis. Complement Ther Clin Pract 39: 101110.
- Sadanandan S, D'Silva F, Renjith V (2021) Body Cathexis among Stroke Survivors: A Cross-Sectional Study. J Neurosci Rural Pract 12: 33-38.
- Timothy EK, Graham FP, Levack WMM (2016) Transitions in the Embodied Experience After Stroke: Grounded Theory Study. Phys Ther 96: 1565-1575.
- Soares JLF, Santos AT (2020) Spatial and Temporal Structuring of Children at a State School in the City of Montes Claros - MG. National Electronic Journal of Physical Education 6: 65-66.
- Le Boulch J (1982) Psychomotor development: from birth to 6 years: educational consequences, psychokinetics in pre - school age. Porto Alegre: Artmed.
- Grau-Sánchez J, Münte TF, Altenmüller E, Duarte E, Rodríguez-Fornells A (2020) Potential benefits of music playing in stroke upper limb motor rehabilitation. Neurosci Biobehav Rev 112: 585-599.
- Juhel JC (2010) Psychomotricity at the service of the elderly. Think, act and live better. Laval University Press, Canada.
- Kantak S, Jax S, Wittenberg G (2017) Bimanual coordination: A missing piece of arm rehabilitation after stroke. Restor Neurol Neurosci 35: 347-364.
- Menezes KK, Nascimento LR, Pinheiro MB, Scianni AA, Faria CD, et al. (2017) Lower-limb motor coordination is significantly impaired in ambulatory people with chronic stroke: A cross-sectional study. J Rehabil Med 49: 322-326.
- Allgöwer K, Hermsdörfer J (2017) Fine motor skills predict performance in the Jebsen Taylor Hand Function Test after stroke. Clin Neurophysiol 128: 1858-1871.
- Schumacher R, Bruehl S, Halai AD, Ralph MAL (2020) The verbal, non-verbal and structural bases of functional communication abilities in aphasia. Brain Commun 2: fcaa118.
- Osorio-Valencia E, Torres-Sánchez L, López-Carrillo L, Rothenberg SJ, Schnaas L (2018) Early motor development and cognitive abilities among Mexican preschoolers. Child Neuropsychol 24: 1015-1025.
- Joy MT, Carmichael ST (2021) Encouraging an excitable brain state: mechanisms of brain repair in stroke. Nat Rev Neurosci 22: 38-53.
- Mosor E, Waldherr K, Kjeken I, Omara M, Ritschl V, et al. (2019) An intergenerational program based on psycho-motor activity promotes well-being and interaction between preschool children and older adults: results of a process and outcome evaluation study in Austria. BMC Public Health 19: 1-13.
- Shen C, Liu F, Yao L, Li Z, Qiu L, et al. (2018) Effects of MOTOmed movement therapy on the mobility and activities of daily living of stroke patients with hemiplegia: a systematic review and meta-analysis. Clin Rehabil 32: 1569-1580.
- Stinear C, Lang C, Zeiler S, Byblow WD (2020) Advances and challenges in stroke rehabilitation. Lancet Neurol 19: 348-360.