Apostolopoulou Eleni1*, Zikos Dimitrios2, Georgoudi Aikaterini3, Papadimitriou Eleni3, Tsaousi Theonitsa3, Maniati Maria3 and Poulopoulou Stavroula4
1Nursing Faculty, National and Kapodistrian University of Athens, Athens, Greece
2University of Texas at Arlington, United States
3Nursing department, General Hospital of “Evangelismos”
4Statistician, Biostatistics Laboratory of Nursing Faculty, National and Kapodistrian University of Athens, Greece
*Corresponding Author:
Eleni Apostolopoulou
Nursing Faculty, National and Kapodistrian
University of Athens, Papadiamantopoulou 123
Athens-11527, Greece
Tel: +30 210- 7461450
FaX: +30 210-7461495
E-mail: eapostol@nurs.uoa.gr
Background: The evidence for effectiveness of perioperative antibiotic prophylaxis is well established. However, despite evidence of effectiveness and the publication of guidelines for antimicrobial prophylaxis, use is often suboptimal.
Aim: The aim of the present study was to explore the impact of irrational perioperative antibiotic prophylaxis use on the nursing workload in a surgical ward.
Methods and Material: Α prospective observational study took place for a period of one month in a surgical ward of a general hospital in Athens, Greece. Patient data consisted of demographic characteristics, underlying diseases and data for antibiotic agent, the timing of administration and the duration of prophylaxis. In each shift, structured observational data for nursing workload were collected by the registered nurses of the surgical ward.
Results: A total of 51 patients undergoing surgery operations were prospectively evaluated. Patients received in total 1604 doses. Of these doses, 1106 (69%) were newer antibiotics under restriction. Antibiotic prophylaxis was inappropriately given to 3,9%. The timing indicator was 88,2 %. The use of antibiotic prophylaxis was misuse in 94% and overuse in 96%. The mean daily nursing workload due to
irrational antibiotic prophylaxis was 5,05 hours.
Conclusion: Irrational antibiotic prophylaxis use increase the daily nursing workload 5,05 hours. The adherence with perioperative antibiotic prophylaxis is poor. The education and discussion of our results with surgical team and infection control committee will contribute to reducing the nursing workload, increasing the adherence with prescribing and administering perioperative antimicrobial prophylaxis, and improving the safety and quality care in studied population.
Keywords
Chemoprophylaxis; Compliance; Nursing workload; Surgical site infections
Introduction
Surgical site infections (SSIs) are the second commonest nosocomial infection [1]. Patients who experience SSIs have twice the mortality, are 60% more likely to spend time in an intensive care unit, and are five times more likely to be readmitted to the hospital than patients without SSIs [2]. The efficacy of prophylactic antibiotics in reducing risk of SSI was first demonstrated in both animal and clinical studies in the 1960s [3,4] is estimated that 40 to 60% of SSIs are preventable with proper prophylactic antibiotics administration [5]. Therapeutic levels of antibiotics must be present at the time of the incision to achieve effective prophylaxis. Timing of prophylactic antibiotics administration is critical, with both early and late prophylactic antibiotics administration associated with increased SSI rates [6]. Consensus guidelines’ state that prophylactic antibiotics should be given at the time of induction of anaesthecsia [7].
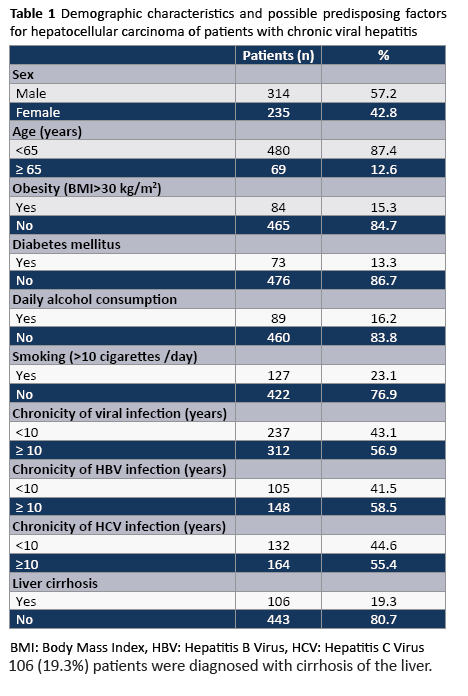
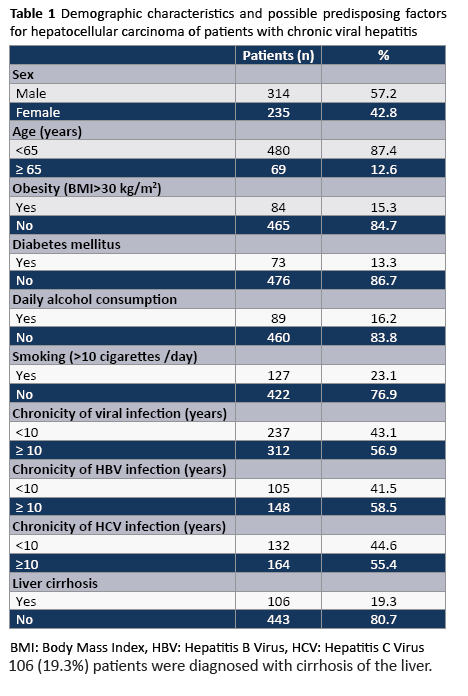
According to Greek national guidelines, a single dose of an antimicrobial agent is sufficient for most surgical operations (Table 1). The recommended antimicrobial agent is second generation cephalosporin. The antibiotics must discontinue within 24 hours for all surgical operations except cardiac surgery operations within 48 hours of surgery end time [7].
Previous studies have evaluated the compliance and cost of antibiotic prophylaxis [8-10]. Nevertheless, to the best of our knowledge, this study is the first published evaluation of impact of inappropriate antibiotic prophylaxis use on the nursing workload in a general surgical ward.
Method and Material
This prospective observational study was carried out for one month (April 2008) in a surgical ward of a general hospital, in Athens, Greece.
During the surveillance period, all patients admitted to the surgical ward were included in the study. Data were collected by using an anonymous standardized survey record form. Patient data consisted of demographic characteristics, underlying diseases and data for antibiotic agent, the timing of administration and the duration of prophylaxis. In each shift, structured observational data were collected by the registered nurses of the surgical ward. The nursing workload was measured in terms of hours including the ordering, preparation, administration and documentation of irrational perioperative antibiotic prophylaxis. Study patients were prospectively followed for the occurrence of a healthcare associated infection until either discharge from surgical ward or death. The appropriateness of antibiotic prophylaxis was determined by Guidelines for Antimicrobial Prophylaxis that was composed by the Central Committee of Nosocomial Infections of the Greek Ministry of Health and Solidarity. There was no standard protocol in the ward or in the operating room, specifying antimicrobial agents for certain procedures, based in the interpretation of the guidelines.
The research protocol has been approved from the Ethics Committee of the Hospital in which the survey has been conducted.
Calculation of Nursing Workload due to Irrational Antibiotic Prophylaxis
The nursing workload due to irrational perioperative antibiotic prophylaxis is the difference between the total hours (for the ordering, preparation, administration and documentation of antibiotic prophylaxis) spent the nurses for administration all antibiotics and the hours for administration the antibiotic prophylaxis recommended by the Greek National Guidelines.
tb = tt - tg
tb: nursing workload due to irrational perioperative antibiotic prophylaxis (for ordering, preparation, administration and documentation).
tt: total hours spent the nurses for the ordering, preparation, administration and documentation all antibiotics.
tg: hours spent the nurses for the ordering, preparation, administration and documentation of perioperative antibiotic prophylaxis recommended by the Greek National Guidelines.
Statistical Analysis
Continuous variables are expressed as mean ± standard deviation (SD) and categorical variables are expressed as a percentage of the total number of Patients analyzed.
Descriptive statistic methods have been utilized in the case of the patient demographic characteristics as well as to describe the level of utilization of antibiotics in surgical operations. The analysis was performed using SPSS software, version 20.
Results
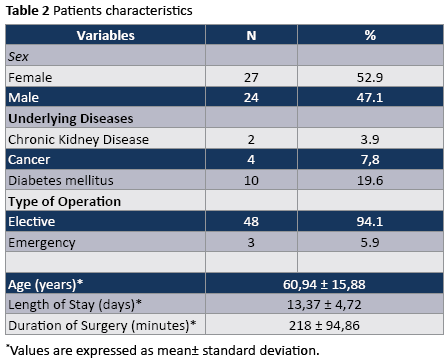
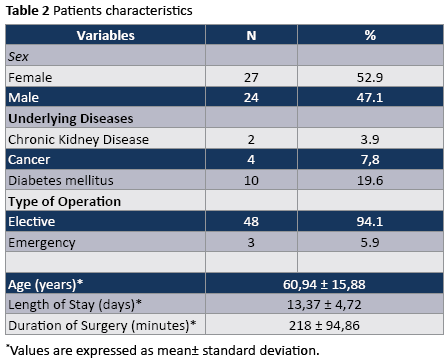
A total of 51 patients undergoing surgery operations were prospectively evaluated. Among the participants, 27 (52%) were females and 24 (47%) males. Of these patients, 3 (5,9%) underwent a clean surgical operation, 41 (80,4%) clean with risk factors and 7 (13,7% ) underwent a clean-contaminated operation. The most common type of surgery operations was cardio surgery (74 .5%) followed by general surgery (21.5%), and orthopedic surgery (3.92%).
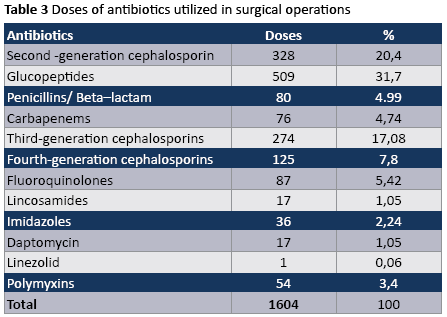
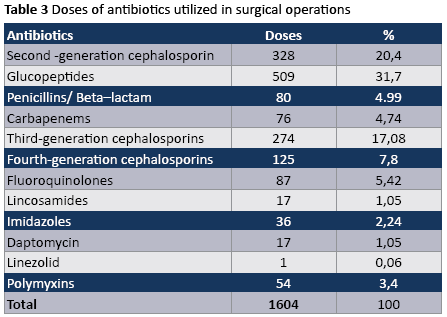
The majority of operations were elective (Table 2) antibiotic prophylaxis was indicated in 49 operations, but in our survey, it was administered to 100% of patients so it was inappropriately given to 3,9%. The timing indicator was 88,2% (antibiotic administration at the time of induction of anaesthesia). The use of antibiotic prophylaxis was misuse in 94% (less effective antibiotics were used) and overuse in 96% (too many doses of antibiotic prophylaxis were used). The most frequently prescribed categories of antibiotics were glycopeptides and second generation cephalosporins. Patients received in total 1604 doses (Table 3). Of these doses, 1106 (69%) were newer antibiotics under restriction (glycopeptides, carbapenems, third and fourth generation cephlosporins, quinolone, lincosamides, daptomycin , linezolid).
During the study period we performed 90 observations, 30 observations for each shift (in the morning, afternoon and night). The mean number of registered nurses was two in the morning shift while in the afternoon and night shift there was only one registered nurse. The mean daily number of hospitalized patients in the studied surgical ward was 42.8 patients. The mean daily time nurses spend due to irrational antibiotic prophylaxis use for all processes was found to be 5.05 hours (ordering, preparation, administration and documentation). In specific, the mean time nurses spend for irrational antibiotic prophylaxis use in the morning shift was 2.11 hours, in the afternoon shift 1.56 hours and in night shift 1.38 hours.
Discussion
The evidence for effectiveness of perioperative antibiotic prophylaxis is well established. However, despite evidence of effectiveness and the publication of guidelines for antimicrobial prophylaxis, use is often suboptimal [8].
Overuse and misuse of antibiotics is common in Greece [9,10]. Prophylaxis with second generation cephalosporin is recommended as a single agent for most procedures [7]. The use of antibiotic prophylaxis was misuse in 94% (less effective antibiotics were used) and overuse in 96% (too many doses of antibiotic prophylaxis were used). The majority of patients received newer antibiotics under restriction. Our observations highlight the need for education of surgeons and anesthesiologist and the communication of data for the increasing of compliance with guidelines for antibiotic prophylaxis in general surgery.
Postoperatively, the administration of antibiotics most often involves nursing care. A national medication error reporting study from the Journal of Infusion Nursing found over a 5-year period that commonly reported Iv-related medication errors in the United States included omissions (28,5%), improper dosing (22,9%) and prescription errors (16,2%). The most common reported reasons for errors involved a clinical performance deficit. These deficits included failing to perform the task (48%) not following procedure or protocol (28%) and in accurate or omitted transcription (14%) [11].
In a recent study in Canada, [12] dose omissions were not as much of an issue as improper dosing, especially with timing of postoperative doses. Nursing guidelines gave an acceptable timeframe for dose administration as ± 1 hour of the scheduled time. In all, 79% of patients received postoperative antibiotics. However, only 34% received those doses correctly, 61% of patients had no documented reactions for receiving an incorrect antibiotic prophylaxis regimen. This presents an opportunity to improve the tracking and documenting of patient care [12]. Previous studies have demonstrated that appropriate timing of antimicrobial administration, inappropriate selection of the antimicrobial agent and excessive duration of prophylaxis, leading to drug reactions, the development and dissemination of bacterial resistance including strains resistant to newer agents, and the burdening of the health systems with unnecessary costs [5,13]. Nevertheless, to the best of our knowledge, this study is the first published evaluation of impact of irrational perioperative antibiotic prophylaxis use on the nursing workload in a general surgical ward.
The principal finding of our study was that the mean daily nursing workload due to irrational perioperative antibiotic prophylaxis was 5.05 hours. In specific, the mean time nurses spend for irrational antibiotic prophylaxis use in the morning shift was 2.11 hours, in the afternoon shift 1.56 hours and in night shift 1.38 hours. Our results are important in clinical practice. Investigating factors influencing nursing staff performance may help bring about strategies for improving adherence to medication administration. For antibiotic prophylaxis, each additional postoperative dose creates additional work and thus an opportunity for error. Singledose preoperative prophylactic regiments would eliminate the problems with postoperative prophylactic antibiotic administration entirely. This could help reduce the workload of the nursing staff, simplifying the postoperative management of patients and potentially decrease the overall incidence of medical errors [12].
Importantly, other investigators have demonstrated the effect of nursing workload on the occurrence of infection. It could be attributed to the fact that under the pressure of increased workload, healthcare workers do not comply with infection control measures, such
as hand hygiene, due to time constraints [14,15]. We suggest that emphasis must be given to the reducing of nursing workload. It will contribute to reducing many other factors such as job dissatisfaction, burnout, absenteeism and intention to leave the current position which have been linked to negative hospital outcomes, including healthcare-associated infections [16-19].
Additionally, it should be noted that according to International Nurses Association an ideal nurse to patient ratio for surgical ward is 1 nurse to 5 patients. In our study the ratio was 2 nurses for 42.8 patients in morning shift and 1 nurse for 42.8 patients in afternoon and night shift. There is growing evidence to suggest that the staffing is a key determinant of healthcare associated infection in critically ill patients [20-22]. Assuming causality, a substantial proportion of all infections could be avoided if nurse staffing were to be maintained at a higher level [23].
Interestingly, reducing the duration of antibiotic prophylaxis has many potential benefits. The decision to prescribe antimicrobials has to be carefully balanced between immediate benefits and possible adverse effects as well as unfavorable medium-term impact on patient or hospital ecology. Besides improving patient care and ecological benefits, a reduction in inappropriate drug administration can also lead to significant financial savings [24,25].
Study Limitations
These results should be interpreted in the context of several potential limitations. First, our study did not include a sufficiently large number of patients. Second, patients from one general clinic participated in the study so the results are representative only of one clinic. Our findings highlight the need for a multicentre study involving a greater number of patients.
Conclusions
Irrational antibiotic prophylaxis use increase the daily nursing workload 5,05 hours. The adherence of surgeon and anesthesiologists with guidelines for perioperative antibiotic prophylaxis is poor. The education and discussion of our results with surgical team and infection control committee will contribute to increasing the adherence with prescribing and administering perioperative antimicrobial prophylaxis, reducing the nursing workload and improving the safety and quality care in studied population.
3753
References
- Burke JP (2003) Infection control - a problem for patient safety. N Engl J Med 348: 651-656.
- Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ (1999) The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 20: 725-730.
- Burke JF (1961) The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery 50: 161-168.
- Polk HC Jr, Lopez-Mayor JF (1969) Postoperative wound infection: a prospective study of determinant factors and prevention. Surgery 66: 97-103.
- Bratzler DW, Houck PM, Richards C, Steele L, Dellinger EP, et al. (2005) Use of antimicrobial prophylaxis for major surgery: baseline results from the National Surgical Infection Prevention Project. Arch Surg 140: 174-182.
- Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, et al. (1992) The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med 326: 281-286.
- Voros D, Gerasimidis TH, Geroulanos S, Kampouridis A, Lelekis M (2007) Guidelines for diagnosis and empirical treatment of surgical infections: Central Committee of Nosokomial Infections of the Greek Ministry of Health. Athens, Greece.
- Dellinger EP, Hausmann SM, Bratzler DW, Johnson RM, Daniel DM, et al. (2005) Hospitals collaborate to decrease surgical site infections. Am J Surg 190: 9-15.
- Tourmousoglou CE, Yiannakopoulou ECh, Kalapothaki V, Bramis J, St Papadopoulos J (2008) Adherence to guidelines for antibiotic prophylaxis in general surgery: a critical appraisal. J Antimicrob Chemother 61: 214-218.
- Apostolopoulou E, Zahos N, Ceorgoudi AI, Tsakona M, Nikoloudi P (2010) Adherence to Guidelines of perioperative antibiotic prophylaxis and cost among women undergoing cesarean section. Review of Clinical Pharmacology and Pharmacokinetics 24:19-24
- Hicks RW, Becker SC (2006) An overview of intravenous-related medication administration errors as reported to MEDMARX, a national medication error-reporting program. J Infus Nurs 29: 20-27
- Lundine KM, Nelson S, Buckley R, Putnis S, Duffy PJ (2010) Adherence to perioperative antibiotic prophylaxis among orthopedic trauma patients. Can J Surg 53: 367-372.
- Gyssens IC (1999) Preventing postoperative infections: current treatment recommendations. Drugs 57: 175-185.
- Harbarth S, Sudre P, Dharan S, Cadenas M, Pittet D (1999) Outbreak of Enterobacter cloacae related to understaffing, overcrowding, and poor hygiene practices. Infect Control Hosp Epidemiol 20: 598-603.
- Hugonnet S, Perneger TV, Pittet D (2002) Alcohol-based handrub improves compliance with hand hygiene in intensive care units. Arch Intern Med 162: 1037-1043.
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH (2002) Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 288: 1987-1993.
- Aiken LH, Clarke SP, Sloane DM; International Hospital Outcomes Research Consortium (2002) Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care 14: 5-13.
- Jackson M, Chiarello LA, Gaynes RP, Gerberding JL (2002) Nurse staffing and health care-associated infections: Proceedings from a working group meeting. Am J Infect Control 30: 199-206.
- Zimmerman S, Gruber-Baldini AL, Hebel JR, Sloane PD, Magaziner J (2002) Nursing home facility risk factors for infection and hospitalization: importance of registered nurse turnover, administration, and social factors. J Am Geriatr Soc 50: 1987-1995.
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K (2002) Nurse-staffing levels and the quality of care in hospitals. N Engl J Med 346: 1715-1722.
- Fridkin SK, Pear SM, Williamson TH, Galgiani JN, Jarvis WR (1996) The role of understaffing in central venous catheter-associated bloodstream infections. Infect Control Hosp Epidemiol 17: 150-158.
- Pessoa-Silva CL, Toscano CM, Moreira BM, Santos AL, Frota AC, et al. (2002) Infection due to extended-spectrum beta-lactamase-producing Salmonella enterica subsp. enterica serotype infantis in a neonatal unit. J Pediatr 141: 381-387.
- Hugonnet S, Chevrolet JC, Pittet D (2007) The effect of workload on infection risk in critically ill patients. Crit Care Med 35: 76-81.
- Prado MA, Lima MP, Gomes Ida R, Bergsten-Mendes G (2002) The implementation of a surgical antibiotic prophylaxis program: the pivotal contribution of the hospital pharmacy. Am J Infect Control 30: 49-56.
- Queiroz R, Grinbaum RS, Galvão LL, Tavares FG, Bergsten-Mendes G (2005) Antibiotic prophylaxis in orthopedic surgeries: the results of an implemented protocol. Braz J Infect Dis 9: 283-287.