Keywords
Healthcare systems; Kuwait; Population
Introduction
Healthcare systems (HCS) all over the world are facing escalating challenges as a consequence of increasing life expectancy and the growth of the ageing population [1]. Additionally, findings demonstrate that the HCS experience many preventable medical errors leading to both financial and human cost [2]. Even more, the financial constraints facing most countries are adding to the current crisis. Growing healthcare costs are directing the attention of many governments for investing to improve the efficiency of their HCS in providing high-quality services and to prevent medical errors.
Kuwait is not in a dissimilar position. Although Kuwait has made significant improvements in its HCS, there is a requirement to have more major development and improvement. Specifically, Kuwait is expected to face several challenges, such as financial deficits along with both political and public concerns about the level of the care services provided by the Kuwait Ministry of Health (MOH) in terms of its quality, safety, efficiency and staff engagement. Moreover, the increase in demand, changing demographics and the nature of diseases means that the future of the HCS in Kuwait is uncertain. These problems are not confined to the Kuwaiti HCS, it is a global problem. Many developed countries have had massive investment in order to improve their service efficiency, but this is not the case in Kuwait. To address some of these challenges, several institutes and organisations have adopted manufacturing improvement methods and techniques [3]. One noticeable improvement approach that promises to improve quality, efficiency and safety while reducing costs is lean management [4]. It began a long time ago in the industrial sectors and could be applied successfully in the healthcare industry [5]. As lean is implemented in the industrial area where the value is to create profit, the situation in HCS is for maximum value for the customers.
As part of a three-year PhD research project, this article is looking through the literature to explore the feasibility and motivation factors of studying lean thinking in the Kuwaiti healthcare system. The aim is to identify the gaps and direct any future research to the right path, to understand the potential for applying lean thinking in Kuwait and rationing the selected area where a pilot project is intended to be conducted.
Methodology
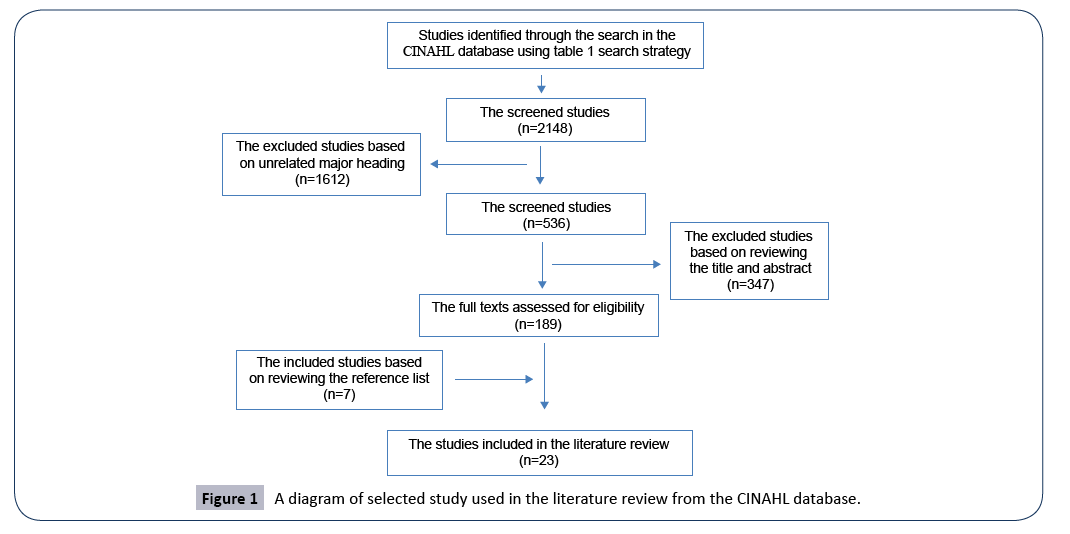
The method used in this research involved critically reviewing the retrieved literature. This research followed a structural review approach to make sure that the full range of literature is exposed and analysed. While the literature review is not systematic in the purest sense, it followed similar principles attempting to minimise bias. The researcher had conducted an extensive search of the literature to ensure capturing the most important concepts relating to the research aim and objectives. Using advanced techniques such as search criteria, combining keywords together, leads to a more focused strand of research. The used keywords included: “Health”, “healthcare”, “Health care”, “health system”, “hospital”, “Outpatient Clinic”, “Health Centre”, “Health Centre”, “Health Service”, “acute care”, “primary care”, “secondary care”, “tertiary care”, “rehabilitation”, “home care”, and “community care” accompanied of one of the key terms: “Lean”, “Lean approach”, “Lean process”, “Lean methodology”, “Lean method”, “Lean transformation”, “Lean philosophy”, “Lean principles”, “Lean practices”, “Lean process improvement”, “Lean management”, “Lean healthcare”, “Lean thinking”, “Lean production”, “Toyota production system”, “Just in Time”, “Value stream mapping”, “Process map” “Kaizen” and “Rapid improvement event”. Several databases were explored comprehensively considering two aspects lean and healthcare. Several databases were searched. These databases were Medline, CINAHL, Google Scholar, Embase and Cochrane Library. A strategy was followed to ensure directing the search to reach the aim of the study. Only in Google scholar searches which has tens of thousands of results, the author reviewed the results of the first ten pages. The CINAHL search, as an example, is shown in Table 1 and Figure 1.
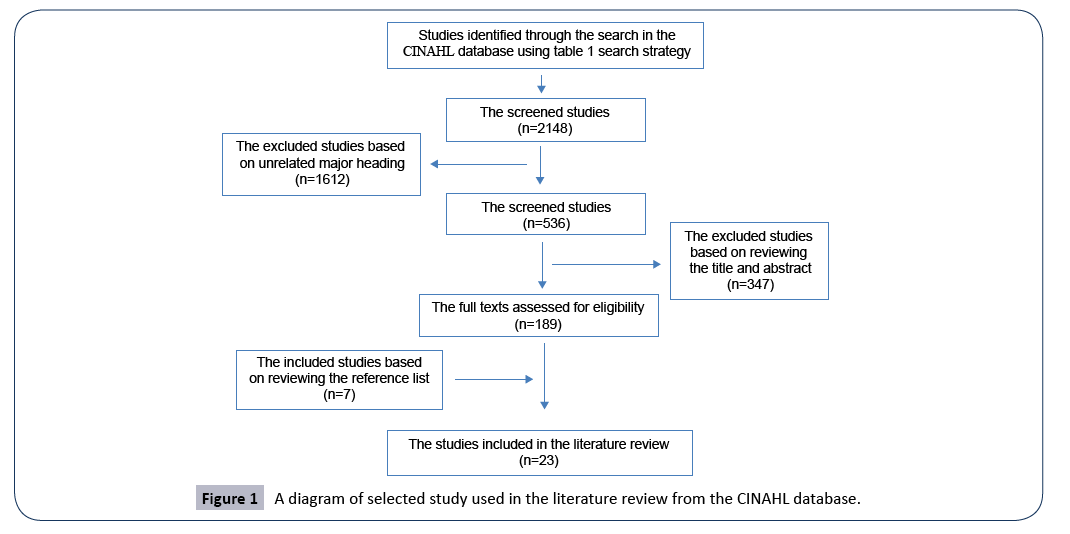
Figure 1: A diagram of selected study used in the literature review from the CINAHL database.
Table 1 An example of the search strategy used to search the CINAHL database.
| Search one |
Lean” OR “Lean approach” OR “Lean process” OR “Lean methodology” OR “Lean method” OR “Lean transformation” OR “Lean philosophy” OR “Lean principles” OR “Lean practices” OR “Lean process improvement” OR “Lean management” OR “Lean healthcare” OR “Lean thinking”, “Lean production” OR “Toyota production system” OR “Just in Time” OR “Value stream mapping” OR “Process map” “Kaizen” OR “Rapid improvement event”. |
| Search two |
“Health” OR “healthcare” OR “Health care” OR “health system” OR “hospital” OR “Outpatient Clinic” OR “Health Centre” OR “Health Centre” OR “Health Service” OR “acute care” OR “primary care” OR “secondary care” OR “tertiary care” OR “rehabilitation” OR “home care” OR “community care” |
| Search three |
Search one AND two |
The search included the articles published in peer review journals, in the English language and after the year 2000 until May 2019. Only the studies that used lean as a sole approach were considered, while the studies that utilised a hybrid approach (where lean was used with other methods such as six sigma) were excluded. The retrieved publications were reviewed by looking at the abstract to identify the articles that were of relevance. Following the snowball method, all the reference lists of the articles found were reviewed. This gives a wider finding and narrows the chance of missing essential textbooks and articles especially the lean topics that could be published in many other subjects. Beside the electronic database searches, the review will look at national publications where relevant, the grey literature and the official websites of different organisations. The grey literature was explored using Google using the same previous terms. Also, the search concentrated on specific organisation’s websites (where lean started to be implemented, havening higher attention and interest mostly in the USA, UK and developed countries in general) including:
• Institute for Healthcare Improvement
• Virginia Mason Institute
• NHS quality improvement
• Lean enterprise institute
• Lean Enterprise Academy
• The Kings Fund
• The Health foundation
• Department of Health (UK)
Results and Discussion
Based on the literature review, the researchers select to explore the case for lean in Kuwait’s healthcare system by applying lean to enhance the flow of patients with diabetes in Primary Healthcare Centres (PHC). The following findings justify the above topic selection where it answers the following six whys questions: why lean, why patient flow, why Kuwait, why diabetes and why primary healthcare.
Why lean
Lean has only been introduced to healthcare during the last 15 years (infant stage) in comparison with the manufacturing industry wher it has been used for more than 50 years ago [6,7]. More investing in effort and time is required to appreciate the full potential of lean. A significant gap in the literature regarding lean implementation is the lack of rigorous methodology of lean application [1,8-10] and the missing of the control group of most of the research methodology design [8,11]. The practice of lean thinking has the potential for great application in the healthcare arena [12]. Further research is required [13-15]. Another finding is that superficial patient involvement in the lean initiative [16,17] where lean has failed to improve patient satisfaction [11]. Poksinska, Fialkowska-Filipek [18] state, “That Lean healthcare implementations primarily target efficiency and little attention is paid to the patient’s perspective”. Therefore, any new research should pay more attention to bring the patients voice before, during and after the lean project implementation. Most of the initiatives were implemented on a specific service and in a specific period and as lean philosophy is not an on and off concept and it required a continuous improvement culture in order to achieve a sustainable improvement [19-21]. Lean must be implemented as an holistic way to gain its full potential and results [22-24]. A national framework is required for lean to be adapted across the entire system [25,26].
Why patient flow
Even with abundant researches in the literature, lean interventions had weak evidence on improving staff satisfaction, service quality, patient satisfaction and an effect on cost reduction [11]. On the other hand, a systematic review concluded that lean interventions have a potential yet inconsistent, benefit on process outcomes like patient flow and called for more research [11].
Why Kuwait
Healthcare organizations, mainly in developed countries, explored whether a lean as a management system is able to support the services quality improvement and enhance patient satisfaction. Despite lean having the potential for providing benefits to the developing countries HCS [8,27], there is a shortage of extensive research in that context. Most of the research has been conducted in developed countries [28,29] where the context and the level of system development is different than that in developing countries [14,30-32]. The impact of the context where lean is pretending to be implemented is considered a strong influential factor on the results that could be achieved [33]. This point encourages the developing countries to invest more for exploring the feasibility of lean management to tackle the different existing challenges. Kuwait is an example of developing countries that has massive expenditure on expanding the MOH infrastructure by building clinics and hospitals. As a consequence, the MOH is undergoing to double their total bed capacity within four years. These changes will drive the necessity of adoption of an efficient approach to run the healthcare services and utilize the present recourses effectively [34].
Why primary healthcare
Within the literature, numerous articles discussed the lean management approach in healthcare and mentioned different tools used to improve the services mostly in hospitals [14,35]. On the other hand, few studies explore the lean implementation within the PHC [30,36-38]. The greater part of researches has focused on the areas with high cost and pressures such as emergency departments and operating theatres [39-43]. There is a present requirement to look beyond the hospitals for improving patient flow [44].
Why diabetes
Diabetic patient flow in PHC can be selected to be studied in the future. In Kuwait, the majority of diabetic patients are followed in the PHC. In 2015, there were almost one million diabetic patient visits to the PHC, while 100 thousand visits were in the government hospitals [45]. More than 80% of diabetic patient OPD visits were in the PHC. The justification for highlighting the diabetic aspect is the high prevalence. The Kuwait adult population has the sixth highest prevalence, affecting approximately 24% of the population [46]. The economic burden resulting from diabetic patients is huge. More than 60% of hospital bed days in the UK were occupied by patients suffering from chronic illness or related complications [47]. In Kuwait, diabetes is the principal or secondary diagnosis in 40.6% of hospitalizations [48]. Moreover, the follow-up of diabetic diseases is a long-life journey where a medical doctor, along with other healthcare providers will see the patient on a regular basis. Therefore, looking at improving the diabetic patient flow is worthwhile.
Notwithstanding the wide interest in lean methodologies within HCS [49-51], It has been concluded that there is weak evidence about the effectiveness of lean for improving the quality of services [11,52-54]. Despite the weak evidence noted in systematic reviews, there are calls for further research in the application of lean to HCS. The researcher argues that there is a necessity to explore the potential of lean application in more depth within the HCS. The explanations of the high percentage of lean implementation failures are due to the absence of senior management support, misunderstanding of the concept of lean management [55] and lack of the correct culture required for successful lean implementation [56]. Even in the business sector, unsuccessful lean implementation is very common. According to a review done in 2007, the companies that succeeded with full lean program implementation represented only 2 per cent [56]. Other additional explanations of the reasons that lean in healthcare does not gain the same results that Toyota did are shown in Table 2.
Table 2 The reasons that lean in healthcare does not gain the same results that Toyota achived (Develop by researcher).
| No. |
Reasons that lean in healthcare does not gain the same results that Toyota did |
| 1 |
Lean has only been introduced to healthcare during the last 15 years (infant stage) in comparison to the manufacturing industry more than 50 years ago |
| 2 |
Contextual differences between healthcare and manufacturing leads to more preparedness and understanding of the approach and the way to implement lean |
| 3 |
Lean philosophies take time to be embedded within the organisation culture. |
| 4 |
Lean application requires the commitment and support of HCW in their day-to-day work |
| 5 |
Lean implementation is considered a change project, so it will face the same difficulties and obstacles for any change project |
| 6 |
It is not implemented in a holistic way to gain its full potential and results |
| 7 |
As it is a contextual philosophy, the adoption and adapting of the tools must meet the culture and the environment where it is implemented |
| 8 |
Most of the initiatives were implemented on a specific service and in a specific period and as lean philosophy is not an on and off concept it requires a continuous improvement culture in order to achieve a sustainable improvement. |
| 9 |
It needs to create a culture of continuous improvement in order to gain the promised benefit from lean philosophy. |
| 10 |
The way that lean is translated and implemented within healthcare could explain the delays and the variations to gain successful results |
In order to address the previous limitation, it is beneficial to pilot lean adoption in Kuwait to enhance the flow of patients with diabetes in PHC.
Conclusion
This review article critically examined the literature for the potential of lean in Kuwait’s HCS. It found that lean has the potential yet inconsistent benefits on process outcomes like patient flow; lacks rigorous evaluation with missing the control group; superficial input from patients; narrow technical application with limited organisational reach. The other finding was that lean was not explored in primary care and there is a deficiency in projects within developing countries. Lean appears to have the potential for providing benefits to healthcare in Kuwait and there is a shortage of extensive research in that context. The key findings are from literature driven researchers and organisations undertaking further research on the use of lean in healthcare. In light of the above, it is worthful exploring the case for adopting lean in Kuwait to enhance the flow of patients with diabetes in PHC.
26638
References
- Poksinska B (2010) The current state of Lean implementation in health care: literature review. Qual Manag Health Care 19: 319-329.
- Kohn LT, Corrigan JM, Donaldson MS (2000) To err is human: building a safer health system. Washington (DC), National Academy Press.
- Ruiz U (2004) Quality management in health care: a 20-year journey. International Journal of Health Care Quality Assurance 17: 323-333.
- Kaplan GS, Patterson SH, Ching JM, Blackmore CC (2014) Why Lean doesn't work for everyone. BMJ Qual Saf 23: 970-973.
- Womack JP, Jones DT (2003) Lean thinking: banish waste and create wealth in your corporation. Revis and updated. London: Simon & Schuster.
- de Souza LB (2009) Trends and approaches in lean healthcare. Leadership in Health Services 22: 121-139.
- Andersen H, Rovik KA, Ingebrigtsen T (2014) Lean thinking in hospitals: is there a cure for the absence of evidence? A systematic review of reviews. BMJ Open 4: e003873.
- de Silva D (2013) Improving patient flow across organisations and pathways. The Health Foundation.
- Mazzocato P, Savage C, Brommels M, Aronsson H, Thor J (2010) Lean thinking in healthcare: a realist review of the literature. Qual Saf Health Care 19: 376-382.
- Woodnutt S (2018) Is Lean sustainable in today's NHS hospitals? A systematic literature review using the meta-narrative and integrative methods. International Journal for Quality in Health Care 30: 578-586.
- Moraros J, Lemstra M, Nwankwo C (2016) Lean interventions in healthcare: do they actually work? A systematic literature review. Int J Qual Health Care 28: 150-165.
- Houchens NW, Kim CS (2014) The Application of Lean in the Healthcare Sector: Theory and Practical Examples, in Lean Thinking for Healthcare pp: 43-53.
- Joosten T, Bongers I, Janssen R (2009) Application of lean thinking to health care: issues and observations. International Journal For Quality In Health Care: Journal Of The International Society For Quality In Health Care 21: 341-347.
- D'Andreamatteo A, Ianni L, Lega F, Sargiacomo M (2015) Lean in healthcare: A comprehensive review. Health Policy 119: 1197-1209.
- Abuhejleh AA, Dulaimi M, Ellahham S (2016) Using Lean management to leverage innovation in healthcare projects: case study of a public hospital in the UAE. BMJ Innovations 2: 22-32.
- Radnor Z, Osborne SP (2013) Lean: A failed theory for public services? Public Management Review 15: 265-287.
- Radnor ZJ, Holweg M, Waring J (2012) Lean in healthcare: the unfilled promise? Soc Sci Med 74: 364-71.
- Poksinska BB, Fialkowska-Filipek M, Engström J (2017) Does Lean healthcare improve patient satisfaction? A mixed-method investigation into primary care. BMJ Qual Saf 26: 95-103.
- Plytiuk CF, da Costa SG, de Lima EP (2013) Lean in healthcare: a systematic literature review and social network analysis. in POMS 25th Annual Conference, Atlanta, GA, USA. 20. Costa LBM, Filho MG (2016) Lean healthcare: review, classification and analysis of literature. Production Planning & Control 27: 823-836.
- Hallam C, Contreras C (2018) Lean healthcare: scale, scope and sustainability. International Journal of Health Care Quality Assurance 31: 684-696.
- Matt DT, Arcidiacono G, Rauch E (2018) Applying lean to healthcare delivery processes-a case-based research. International Journal on Advanced Science, Engineering and Information Technology 8: 123-133.
- Mazzocato P, Stenfors-Hayes T, Schwarz UT, Hasson H, Nyström ME(2016) Kaizen practice in healthcare: a qualitative analysis of hospital employees' suggestions for improvement. BMJ Open 6: e012256.
- Parkhi SS (2019) Lean management practices in healthcare sector: a literature review. Benchmarking: An International Journal 26: 1275-1289.
- Breuer DJ (2013) Lean implementation in healthcare-the challenged transformation. in IIE Annual Conference. Institute of Industrial and Systems Engineers (IISE).
- Machado CM, et al. (2015) Healthcare lean operations: Building an effective management framework. Organization 1: 4.
- da Silva IB, Seraphim EC, Agostinho OL, Lima OF (2015) Lean office in health organization in the Brazilian Army. International Journal of Lean Six Sigma 6: 2-16.
- de Souza LB (2009) Trends and approaches in lean healthcare. Leadership in health services 22: 121-139.
- Fillingham D (2007) Can lean save lives? Leadership in health services 20: 231-241.
- Costa LB, Filho MG, Rentes AF, Bertani TM, Mardegan R (2015) Lean healthcare in developing countries: evidence from Brazilian hospitals. Int J Health Plann Manage 32: e99-e120.
- Plytiuk CF, et al. (2012) Lean Thinking in Health care: An overview of the research characteristics, themes and knowledge groups (1998-2011). in IIE Annual Conference. Proceedings. 2012. Institute of Industrial and Systems Engineers (IISE).
- Magalhães ALP, Erdmann AL, da Silva EL, dos Santos JLG (2016) Lean thinking in health and nursing: An integrative literature review. Revista Latino-Americana de Enfermagem 24.
- Shah R, Ward PT (2003) Lean manufacturing: context, practice bundles, and performance. Journal of operations management 21:129-149.
- Kelendar H (2017) The Future of Kuwait Healthcare System Challenges and Aspirations: Can Lean Management be the solution. Conference: Kuwait conference on quality in healthcare, At Kuwait
- Daultani Y, Chaudhuri A, Kumar S (2015) A Decade of Lean in Healthcare: Current State and Future Directions. Global Business Review 16: 1082-1099.
- Hasle P, Nielsen AP, Edwards K (2016) Application of Lean Manufacturing in Hospitals-the Need to Consider Maturity, Complexity, and the Value Concept. Human Factors and Ergonomics in Manufacturing & Service Industries 26: 430-442.
- Roberts S, Singh S (2009) Implementing lean in primary care. British Journal of Healthcare Management 15: 380-386.
- Dickson EW, Singh S, Cheung DS, Wyatt CC, Nugent AS. (2009) Application of lean manufacturing techniques in the Emergency Department. J Emerg Med 37: 177-182.
- Gupta D, Denton B (2008) Appointment scheduling in health care: Challenges and opportunities. IIE Transactions 40: 800-819.
- Holden RJ (2011) Lean Thinking in emergency departments: a critical review. Ann Emerg Med 57: 265-278.
- King DL, Ben-Tovim DI, Bassham J (2006) Redesigning emergency department patient flows: application of Lean Thinking to health care. Emerg Med Australas 18: 391-397.
- Rutman L, Stone K, Reid J, Woodward GA, Migita R(2015) Improving patient flow using lean methodology: an emergency medicine experience. Current Treatment Options in Pediatrics 1: 359-371.
- Fillingham D (2016) The challenge and potential of whole system flow. Health Foundation.
- Kuwait Ministry of Health, Annual Health Report (2015) National Center of Health Information, Ministry of Health: Kuwait.
- Conway N, et al. (2014) The Kuwait–Scotland eHealth Innovation Network (KSeHIN): a sustainable approach to quality improvement in healthcare. Quality in primary care 22: 43-51.
- Al-Adsani AMS, Abdulla KA (2015) Reasons for hospitalizations in adults with diabetes in Kuwait. International Journal of Diabetes Mellitus 3: 65-69.
- Aherne J, Whelton J (2010) Applying lean in healthcare: a collection of international case studies. CRC Press.
- Bercaw RG (2013) Lean leadership for healthcare: approaches to lean transformation. CRC Press.
- Black JR, Miller D (2008) The Toyota way to healthcare excellence: increase efficiency and improve quality with LEAN. Health Administration Press.
- Blumenthal D, Kilo CM (1998) A report card on continuous quality improvement. The Milbank Quarterly 76: 625-648.
- Joosten T, Bongers I, Janssen R (2009) Application of lean thinking to health care: issues and observations. International Journal for Quality in Health Care 21: 341-347.
- Øvretveit J, Gustafson D (2002) Evaluation of quality improvement programmes. BMJ Quality & Safety 11: 270-275.
- Liker J, Rother M (2011) Why lean programs fail. Lean Enterprise Institute 2011: 45-79.
- Mann D (2014) Creating a lean culture: tools to sustain lean conversions. CRC Press.
- Pay R (2008) Everybody’s jumping on the lean bandwagon, but many are being taken for a ride. Industry Week.