Keywords
myocardial infarction, risk factors, educational stragety, quality of life, symptomatology, cholesterol.
Introduction
Myocardial infarction (MI) is the condition of irreversible necrosis of the heart muscle that results from prolonged ischemia, approximately mainly when the coronary arteries that supply blood to heart become completely obstructed. This obstruction is usually caused by the build?up of plaque in the artery walls or a thrombus in a coronary artery that has developed over the years. A decreasion in the amount of oxygen in the blood or in the body’s organs can also trigger a heart attack. A healthy coronary artery spasm, which leads to the decreasion of blood flow to the heart, may rarely be a cause of myocardial infarction (MI). Moreover, recent research suggests that myocardial infarction may also occur as the result of an inflammation of the heart, which is thought to be the easiest way for the formation of a clot [1,2].
A number of different risk factors, contribute to coronary artery disease and therefore to myocardial infarction. These factors can be modifiable, such as smoking, hypertension, diet high in fat, poor blood cholesterol levels, particularly a high LDL value combined with a low HDL level and nomodifiable such as the gender with males at higher risk, the age and the heredity [3,4,5].
After World War II coronary heart disease (CHD) assumed epidemic proportions in western countries. In many countries the peak of the epidemic occurred in 1968. Nowadays, myocardial infarction is the leading cause of death in developed countries and the induced ?disability and loss of productivity are the most frequent reslults of the disease. M.I represents a high economic burden, as the costs increase with the disease progression. Although the incidence?rates of the manifestation of the disease have significantly declined during recent decades, myocardial infarction still remains the first cause of death in U.S. It is estimated that, every year close to 1.5 million Americans sustain a myocardial infarction (MI). Nearly 1 million patients are anually admitted to the hospitals and the event proves fatal in approximately one third of patients. In Greece, coronary diseases are responsible for the one third of mortality annually, approximately 30.000 individuals [6,7,8].
It is widely accepted that cardiac rehabilitation following myocardial infarction reduces subsequent mortality and for this reason emphasis must be given to educational programmes which highlight the importance of motivating behavour change. Although conventional medical treatments may help an individual recover from a heart attack, an educational strategy may be required to improve knowledge about a wide range of issues concerning myocardial infraction and thus initiate a new life style adjusted to the demands of the disease [9,10].
Statistical analysis was performed with SPSS 10 and t?test value.
Results
Descriptive results
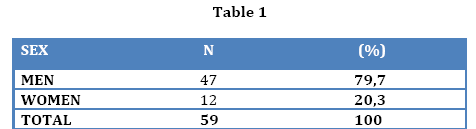
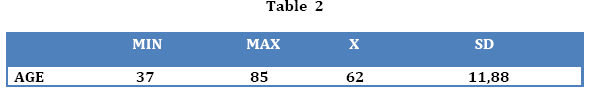
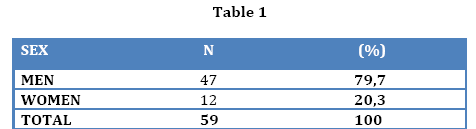
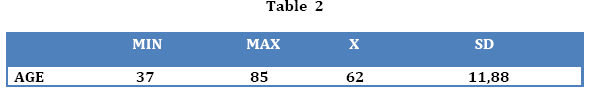
The data analysis has shown that 79.7% were men and 20.3% were women (Table 1) with a mean age of 62 years old (Table 2). The patients’ weight ranged from 45 to 125 kgr, with a mean body weight of 77.05 kgr and standard deviation ±13.49 (Table 3).

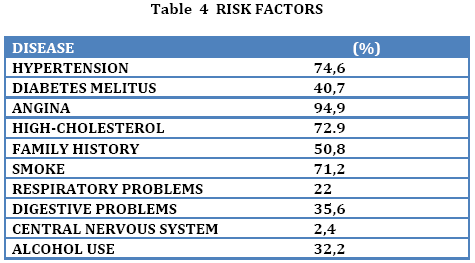
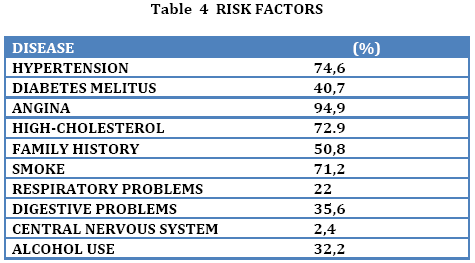
Among the risk factors, 74.6% of patients were hypertensive, whereas 40.7% suffered from diabetes mellitus. 50.8% of the patients demonstrated a family history of coronary artery disease, whereas in 94.9% of the patients angina pectoris co?existed. Regarding the nervous system 2.4% had suffered a stroke and 72.9% of patients showed an increased level of cholesterol prior to the MI. 71.2% of the patients were smokers, whereas alcohol was consumed by 32.2% of the patients (Table 4).
Regarding the administration of antihypertensive medication treatment and the type of medication, 27.1% of patients received no medication, whereas the remaining 63.6% was already receiving medication. As regards the antilipidemic treatment, only 55.8% received medication.
The majority of the sample showed a total lack of physical exercise at a rate of 59.3%, versus 40.7% of those who exercised, with variations in the kind and frequency of exercise.
Comparative results
Comparing the results of the first to those of the second interview, it was revealed that the mean value of cholesterol during the first assessment was 216.14 with standard deviation ±43,43, and at the second assessment the mean value of cholesterol was 195.31±31.69, with a statistically significant difference p=<0,001. The mean value of HDL at the first evaluation was 46.23±13.08 and the mean value of the second evaluation was 53.69±11.83, with a statistically significant difference p=<0,001. The mean value of LDL at the first evaluation was 144.60 ±46.17 and the mean value of LDL 131.47 ± 58.41 during the first re?evaluation, with a statistically significant difference p=<0,004.
The mean value of TG displays a reduction between the two assessments. At the first assessment, the mean value of TG was 157.83 ± 95.56 and at the second assessment the mean value of TG was 155.02 ± 124.69, with a statistically significant difference p=<0,021(Table 5).

Discussion
It is shown from the present study that men prevailed in number at a percentage rate of 79.7% versus 26.3% in women, supporting the aspect that women are protected from myocardial infarction due to the presence of cardioprotective estrogens [11,12].
Other research studies prove that the percentage of women who suffer from acute myocardial infarction is constantly increasing13, without however the post?menopausal women reaching the frequency rate of men [14].
A family history of coronary artery disease (CAD) existed in 50.0% of the study population and from similar studies it has been found that, the family history of CAD, prior to the age of 50 in first?degree relatives, increases the risk by two to four times [14]. Furthermore, the aggravating effect of heredity may originate from the hereditary transfer of hypercholesterolemia, hypertension and diabetes [15].
Hypertension is one of the most important independent risk factors for the development of CAD since it promotes atherosclerosis and leads to degenerative lesions at a cellular and vascular level [16,17,18].
Diabetes mellitus is a risk factor for the development of coronary artery disease (CAD). The mechanism through which it predisposes to coronary disease may possibly relate to the accelerated arteriosclerosis, which leads to lesions at the arterial walls. The risk is higher in insulin?dependent individuals for the reason that they frequently demonstrate vasculopathies. The metabolic X syndrome also represents a risk factor, a main characteristic of which is hyperinsulinemia and the reduced tolerance to glucose [19,20,21,22].
Another significant factor for acute myocardial infarction (MI) is smoking and at the present trial the individuals who smoke represent a percentage of 71.2%. The pathophysiological effects of smoking are multifactorial and affect the systemic vascular blood flow and the walls of the vessels. More specifically, smoking is associated with high levels of fibrinogen, resulting in an increased tendency for thrombosis of the blood and coronary artery disease. In addition, it is associated with high levels of hematocrit, with an increased possibility of platelet agglutination and with reduced HDL levels. In accordance to a study conducted by the Cardiology Clinic of the University of Athens, the fibrinogen levels that are co?related with the occurrence of MI are significantly higher in smokers, in comparison to non?smokers. Trials have shown a decrease in the risk of heart attack with the discontinuation of smoking [23-25]. The Framingham trial showed that discontinuation of smoking after an acute MI is accompanied by a reduction in mortality by 60% within the first 6 months [15].
Physical exercise reduces hypertension, diabetes mellitus, body weight, and is associated with lower LDL cholesterol and triglyceride levels. The beneficial effects of physical exercise concerning the reduction in the risk for coronary artery disease have been fully verified. Other mechanisms which are related to physical exercise are the decrease in fibrinogen and the decrease in platelet activity [26-28].
A physical exercise recovery program may lead to a reduction in total and cardiovascular mortality by 20?25% [28]. In the United States of America, two trials, one trial concerning the dock workers of San Francisco (1957?1972) and the other trial concerning Harvard University graduates (1962?1972), showed a lower mortality rate in those who exercised more often. In a similar way in the United Kingdom, the civil servants who regularly participated in rigorous sports presented half the incidence of coronary artery disease, in comparison to their colleagues who held a sitting mode of life [15].
Atheromatosis is the most frequent disease of the vascular system and the main cause of mortality in the Western world. According to the World Health Organization (W.H.O), atherosclerosis is a combination of changes in the tunica intima of the arteries, which consist of an aggregation of lipoid substances, fibrin and other factors. The disorders of the triglycerides, total cholesterol, HDL and LDL are responsible for atherosclerosis of the coronary vessels. The relationship between the increased values of lipids and coronary artery disease is very close. This risk is better evaluated when considering the plasma concentrations of HDL and LDL cholesterol [29-31] Epidemiological data show that there are geographical variations in the incidence of coronary disease, which may be due to dietary habits and are attributed to the difference in the ratio of saturated to unsaturated fatty acids in the individual’s diet [15,32-36].
Medication treatment improves prognosis and the course of the patients. The first choice of medication is the use of b?blockers, for the reason that they reduce the energy needs of the myocardium and have a particular efficacy in men of middle age, especially in patients with anxiety and in patients with high renin levels [37-40].
Regarding the anti?lipidemic treatment, we observe that the study population received medication treatment at a 55.8% rate, and, to be more specific, they received statins. The prevalence of statins in comparison to the other hypolipidemic drugs is justified due to their effectiveness, which is established through a great number of research trials, with the prevalence of this statin, that is atorvastatin. According to another recent study, Statins can lower cholesterol concentration by an average of 1.8mmol/L which reduces the risk of ischaemic heart disease (IHD) events by about 60% [41,42].
The Scandinavian Simvastatin Survival Study (45) is the first great trial which confirmed the efficacy of statins in the secondary prevention of acute cardiovascular episodes. The results of this study were later on confirmed by the CARE study (Cholesterol and Recurrent Events) [43].
According to a recent study, national service framework targets for cardiac rehabilitation and secondary prevention can be achieved in patients who survive a myocardial infarction by integrating rehabilitation services (home and hospital). Nurses in primary care facilitate long term structured care and optimal secondary prevention [44].
Conclusions
Myocardial infarction is major public health problem associated with high mortality, disability, financial cost and requires systematic approach. Apart from the significant impact on human health, it is a matter of great concern to society in all countries. Cardiac rehabilitation programmes following myocardial infarction can reduce subsequent mortality, when information about recovery is provided to the patients by health professionals. The provided?information plays a central role in people's understandings about the nature of the disease and the future risks. Adherence to such interventionprogrammes is really effective and can improve health outcome. It is essential to enforce people’s willingness to adopt lifestyle change after myocardial infraction as a rational action to prevent a further cardiac event.
3683
References
- Kanonidis E.I. Myocardial infraction in elderly. Cardiology 1998; 183‐191.
- Ivanusa M., Ivanusa Z. Risk factors and in hospital outcomes in stroke and myocardial infarction patients. BMC Public Health. 2004; 4:26.
- Mozaffarian D., Fried LP., Burke GL.,et al. Lifestyles of older adults: can we influence cardiovascular risk in older adults? Am J Geriatr Cardiol 2004; 1 3:153‐160.
- Simons LA., Simons J., Friedlander Y., et al. Risk factors for acute myocardial infarction in the elderly (The Dubbo study). Am J Cardiol 2002; 89:16‐19.
- Jamrozik K.,Dobson A., Hobss M., et al. Monitoring the incidence of cardiovascular disease in Australia. Canberra: Australian Institute of Health and Welfare, 2001; AIHW Cat.No CDV 16; Cardiovascular disease, Series No 17.
- Reddy K., Rao A., Reddy Th. Socioeconomic status and the prevalence of coronary heart disease risk factors. Asia Pacific J Clin Nutr. 2002;11(2): 98‐103.
- Keil U. The Worldwide WHO MONICA Project: Results and Perspectives. Gesundheitswesen. 2005 Aug; 67 Suppl 1:38‐45.
- Akosah O., Larson E., Brown M., et al. Using a systemwide care path to enhance compliance with guidelines for acute myocardial infarction. Jt‐Comm‐J‐Qual‐Saf. 2003 May; 29(5): 248‐59
- Spencer A., Salami B., Yarzebski J., et al. Temporal trends and associated factors of inpatient cardiac rehabilitation in patients with acute myocardial infarction: a community‐wide perspective. J‐Cardiopulm‐Rehabil. 2001 Nov‐Dec; 21(6): 377‐84.
- Roeters Van Lennep JE., Westerveld HT., Erkelens DW., et al. Risk factors for coronary heart disease : implications of genger. Cardiovasc Res.2002 Feb; 15;53(3):538‐49.
- Collins P., Stevenson JC., Mosca L. Spotlight on gender. Cardiovasc Res.2002 Feb;15;53(3):535‐7.
- Ahimastos A. Heart coronary protection –Indications and evidences for the blockers of the receptors of the AGGEIOTENSINIWS 2 2nd Pannelinium Symposium – Arterial High Blood Pressure Thessalonica 2000 Mar;p. 4.
- Toutouzas P., Pitsavos H‐Farmer J. New curatives to the confronting of the upper cholesterol with statines. Medical Opportuneness. Book 1, Part 2. April 1998, pp. 28‐29.
- Wood D. et al. Clinical manual for the confronting of total danger. Athens, Edition Bogianaki 2001; 105‐119.
- Gurevich MA. Characteristic features of the pathogenesis and treatment of coronary heart diseases, heart failure and arterial hypertension in patients with diabetes mellitus. Klin Med (Mosk). 2005; 83(1):4‐9.
- Wolf P A. Cerebrovascular risk. In: Izzo JL Jr, Black HR, Goodfriend TL, et al. Hypertension Primer: The Essentials of High Blood Pressure. Baltimore, Md: Lippincott Williams & Wilkins; 1999.
- Joint National Committee. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997; 57:2413‐2446.
- Garvey WT., Hermayer KL. Clinical Implications of the insuline esistance syndrome. Clin Cornerstone.1998; 1:13‐28.
- Baillie GM., Sherer JT., Weart CW. Insuline and coronary artery disease: is syndrome X the unifying hypothesis? Ann Pharmacother.1998; 32:233‐247.
- Todaro JF, Con A, Niaura R, et al.Combined effect of the metabolic syndrome and hostility on the incidence of myocardial infarction (the normative aging study). Am J Cardiol. 2005 Jul 15;96(2):221‐6.
- Cao JJ, Hudson M, Jankowski M, et al.Relation of chronic and acute glycemic control on mortality in acute myocardial infarction with diabetes mellitus. Am J Cardiol. 2005 Jul; 15;96(2):183‐6.
- Lopez Garcia‐Aranda V., Garcia Rubira JC.,Calvo Jambrina R., et al. Influence of coronary risk factors in secondary prevention: tobacco. Rev Esp Cardiol.1998; 51Suppl 6:10‐7.
- Bolego C., Poli A., Paoletti R. Smoking and gender.Cardiovasc Res.2002 ;53 :568‐576
- WORLD HEART FEDERATION. Tobacco, Heart Disease and Stroke. Bonita R., et al..Tob Control. 1999; 156‐160.
- Hedblad B., Orgen M., Isacsson SO, et al. Reduced cardiovascular mortality risk in male smokers who are physically active. Results from a 25‐year follow‐up of the prospective population study men born in 1914. Arch Intern Med 1997; 157:893‐99.
- Ferrucci L.,Izmirlian G., Leveille S., et al. Smoking, physical activity and life expectancy. Am J Epidemiol 1999; 149:645‐653.
- Braunwald E., Fauci A., Kasper D., et al. Harrison’s 15th edition. Principles of Internal Medicine. Volume 2. 2001; 2370‐2375.
- Williams PT. High‐density lipoprotein cholesterol and other risk factors for coronary heart disease in female runners. N Engl J Med. 1996; 334: 1298‐1303.
- Kotchen Τ., Kotchen J. Nutrition and cardiovascular health. In Nutritional Aspects and Clinical Management of Chronic Disorders and Diseases, Bronner F ed. CRC Press. London, 2003.
- Schlitt A, Blankenberg S, Bickel C, et al. Prognostic value of lipoproteins and their relation to inflammatory markers among patients with coronary artery disease.Int J Cardiol. 2005 Jul ;20;102(3):477‐85.
- Virgil Brown, W., Smith D. Nutrition and Heart Disease. In Total Nutrition. Herbert V., and Subak‐Sharpe G ed. St Martins Griffin. New York 1995.
- Chahoud G., Aude VW., Mehta JL. Dietary recommendations in the prevention and treatment of coronary heart disease: do we have the ideal diet yet? Am J Cardiol. 2004 Nov; 15; 94(10):1260‐7.
- Khor GL. Dietary fat quality: a nutritional epidemiology’ view. Asia Pac J Clin Nutr. 2004. Aug; 13 Suppl:S22.
- Wahrburg U. What are the health effects of fat? Eur. J. Nutr. 2004 Mar; 43 Suppl 1:I/6‐11.
- Couvedenos A.I. Do all patients with acute infarction take A‐MEA? Athens 21ο Hellenic Cardiologic Convention. 2000 Νov.
- Tsioufis P.K. Treatment of hypertension. Athens Ε.Κ.Ε. 5‐7 February 1998.
- Brown V. Contemporary tretment of upper‐cholesterol. Médical Opportuneness, Vol 1, Issue 8, Ed. Dictinna. E.P.E. Athens, January 1998.
- Barter P.New treatment with statins. Médical Opportuneness Vol 3, Issue 8, Ed. Dictinna. E.P.E. Athens, January 1998.
- Andrikopoulos GK.Medical treatmentof dislipidemea.Chronicals,Vol,65, supplement 2003, Athens 13‐15 February 2003; 312‐15.
- Amarenco P., Lavallee Ph., Touboul P‐J. Stroke prevention, blood cholesterol and statins. Neurology. 2004 May; 3 (5):271‐8.
- Beijing Neurologist Club.BNC Practise Guidelines of Cerebrovascular Diseases.Beijing : People Medical Publishing House;2002; 41‐66.
- Alan Sourline – « The use of statins to transplant recipients» Médical Opportuneness Athens, 1998 Oct ;2(5):179
- Datal HM., Evans PH. Achieving national service framework standards for cardiac rehabilitation and secondary prevention. BMJ. 2003 Mar 1;326(7387):481‐4.