Keywords
Paramedic; Transitional care; Heart failure
Introduction
Trinitas Regional Medical Center (TRMC) developed a program that utilizes paramedics with additional training as community health workers (CHWs), advanced practice nurses (APN), and emergency medical technician trained dispatchers, with physician oversight focusing on reducing readmissions in the heart failure (HF) population. The program provides an innovative, cost-effective solution to support the heart failure community in the city of Elizabeth, New Jersey. The HF readmission rate at TRMC was higher than the national and state average. Root causes of elevated HF rates at TRMC include poor access to health care, health literacy, and understanding the lifestyle changes needed to maintain health.
Background
Heart failure impact
Heart failure (HF) results in more hospital admissions than any other medical condition in older Americans [1]. According to the American Heart Association, there is a growth in HF cases that is projected to affect approximately 8 million Americans by 2030 [1]. Direct HF costs are expected to rise from $21 billion in 2012 to an estimated $53 billion in 2030 [1]. This growth is due to an aging population at a higher risk of developing HF through the co-morbid conditions of hypertension and coronary artery disease [2]. There is a 20% lifetime risk of developing HF with a five-year mortality rate higher than many cancers [3].
Transitional care models
There are high levels of readmissions following index admissions from HF for various reasons, including poor access to health care, health literacy, and understanding the lifestyle changes needed to maintain health [4]. Due to high rates of readmissions, care models, known commonly as transitional care models, are being developed to understand the reasons for readmission, and to address these issues on an individual basis through self-management and support posthospitalization [4]. Nurse led transitional care programs have shown success improving the HF patient’s quality of life while reducing readmissions. Through readmission reduction, there is an associated reduction in overall cost of caring for this vulnerable population [4]. Different transitional care programs have many similar traits, including establishing hospital and home follow-up visits to coordinate care [5]. These programs have shown some benefits to patients in a short time frame. One such example is a study of 172 high-risk patients through a managed Medicare health plan that reduced rehospitalizations and total hospital days. That study resulted in an annual per-capita savings of $2,170 in the first year [6]. Other studies have shown an all-cause reduction in readmissions and mortality for HF patients in a transitional care program [7].
Community health worker models
Community health workers (CHWs) are traditionally lay members of a community that have been trained in health education and disease specific intervention. They act as patient navigators, health promoters, and advocates. The goal of CHWs is to improve the reach of health knowledge thereby improving the overall health of the population [8]. These programs have been effective in addressing chronic diseases [9] and have been successfully implemented on an international level [10]. The CHW programs in the United States have struggled due to the lack of reimbursement for services in the fee-for-service model [8]. Nevertheless, with the increase of population health programs, there may be increased opportunity for future funding.
Mobile integrated health services
In their traditional roles, EMS providers are called to assess and intervene for often complex medical conditions [11]. Request for EMS services are often identified as emergent. Such interactions require high levels of trust between the public and EMS services. These interventions are under the direction of a physician via on-line and off-line medical direction [11]. Medical direction standards require that paramedics have the ability to communicate with physicians in a clear and appropriate manner.
Mobile Integrated Health Services (MIHS) is the use of prehospital care providers, primarily paramedics, in nontraditional roles for EMS. MIHS utilizes the resources of EMS systems and integrates them in the greater local health system. MIHS resources are then used to target the health needs of the community similar to a CHW model. Oversight is generally provided by physicians. MIHS has received increased attention as legislative changes encouraged health care organizations to attempt innovative models of care delivery to prevent unnecessary hospital readmissions [12]. MIHS programs hold the potential to improve outcomes in chronic disease populations [13] with associated cost reductions [12]. As MIHS is a new role for EMS, there are areas that require additional research including clinical effectiveness and operational sustainability [12]. Research does show promise regarding paramedics having a knowledge base and positive attitude to potentially work with a chronic diabetic population [13].
Pilot MIHS programs located in San Francisco, San Diego, and Washington, D.C. were focused on reducing unnecessary utilization by high frequency EMS and Emergency Department patients [14]. The programs had shown positive outcomes in utilization reduction. The MIHS program in San Francisco reduced emergency “911” requests within a target group by 75% in 18 months [14]. These pilot programs were nonrevenue producing, and because they were financially unsustainable [14], they were disbanded.
Elizabeth, New Jersey demographics
Elizabeth is a city of 124,969 residents [15] with 9.2% of the population older than age 65. Elizabeth is a diverse community with 59.5% of the population of Hispanic origin and 21.1% African-American. Foreign born make up 47.4% of the population, with 73.8% speaking a language other than English as the primary language at home. The per-capita income is $19,061 with 18.4% of the population living below the poverty level [15].
Trinitas regional medical center
Trinitas Regional Medical Center (TRMC) located in Elizabeth was established in January 2000 after the merger between Elizabeth General Hospital and St. Elizabeth’s Hospital. TRMC is a full-service health care facility serving Eastern and Central Union County. Operating on two major campuses, TRMC has 551 beds and treats more than 17,000 inpatients annually, 70,000 emergency patients, and several hundred thousand outpatients. It is the sole inpatient acute care hospital for the city.
Purpose
Compared to the rest of the country and state, residents of Elizabeth have higher rates of cardiovascular disease [16]. The 2014 baseline HF readmission rate at TRMC is above the national and state average. Root causes of the elevated HF readmission rates at TRMC include poor access to health care, medication management, health literacy, and understanding the lifestyle changes needed to maintain health. This issue has prompted TRMC to look at innovative methods to deliver coordinated post-discharge care to HF patients.
Hypothesis
EMS resources can work with a multidisciplinary integrated care team to intervene on HF patients post-discharge with patient education and non-emergent interventions resulting in reduced 30-day readmissions.
Program design
TRMC developed a Mobile Integrated Health Service Program (MIHS) staffed by Community Health Integrated Practitioners (CHIPs). CHIPs are allied health practitioners trained as paramedics, who have undergone additional training in HF specific community health work. The program has medical oversight provided by two physicians—one an emergency physician and the other a primary care physician.
The training program content for CHIPs is based off a gap analysis between the paramedic training standards and training programs for CHWs. There are no standards for a national CHW program curriculum. Four states in the United States have established certification for CHWs; New Jersey does not have any standards for CHWs. The MIHS training program curriculum includes the background and purpose of community health programs, HF pathophysiology, comorbid conditions, pharmacology of chronic HF, HF diet requirements, patient history and physical exam, patient education, the teach-back method, and psycho-social care considerations. Didactic training was a combination of classroom lectures, Internet-based programs, and self-directed learning. Clinical training was provided by the TRMC transitional care APN. Total training time for each CHIP was 56 hours.
The MIHS program is part of the HF continuum of care at TRMC, which is based on the Wagner Chronic Care Model [17]. The model is a partnership between primary care, cardiology, the translational care team (including the CHIP), and the patient. There is a strong health information technology infrastructure, high touch delivery system, and specialty care referral base.
The CHIP receives a referral to the MIHS program from the TRMC transitional care advanced practice nurse (APN) or through a HF screening administered by EMS dispatchers seven days post-discharge. The CHIP visit is scheduled by the TRMC-EMS dispatch center with the patient. The CHIP reviews the patient’s electronic medical record and performs a structured visit. The CHIP documents the visit in a chart, and then reports to the transitional care APN to determine if additional resources are needed. Physicians are available as a resource to both the CHIP and APN. If after evaluation of the CHIP and direction by the designated physician it is determined that the patient requires transportation to the emergency department, standard activation of EMS resources occurs.
A structured CHIP visit consists of a three-tiered approach. First is a basic patient assessment. This would consist of blood pressure, pulse, respiratory rate, pulse oximetry, lung sounds, edema assessment, and weight. The second tier is a review of the home and environmental factors. Areas of assessment include living conditions, family support, fall risk assessment, potential depression, knowledge of home medical equipment (such as home oxygen), smoking, and appropriate temperature regulation in the home. The third tier is patient education, which includes medication reconciliation and education, symptomatology and etiology, warning signs with an understanding of when to contact the patient’s care team, and appropriate diet choices. Each visit can take between one to two hours.
Quality control of the MIHS program is provided monthly with the care teams, APN, physicians, and administrators. The quality program is based on predetermined key performance indicators. The overall measure of success is the 30-day readmission rate for HF. This rate is defined for the purposes of the MIHS as the number of patients that are readmitted within 30 days of the index HF admission divided by the overall HF patients that enter into the program.
Material and Methods
Research design
The researchers performed a descriptive study to address the hypothesis through program evaluation and comparison to a random like group of patients. Data collection required a retrospective data review from three sources. There was minimal risk to participants, as participant risk was not greater than risks encountered ordinarily in daily life, or psychological examinations or tests.
Study participants
The scope of the program is limited to patients with an index HF admission located within the geographic confines of the city of Elizabeth, NJ and discharged from TRMC between July 2014 and May 2016. The HF admission is defined by ICD-9 code for HF as defined by Centers for Medicare & Medicaid Services [9]. A control group was chosen randomly of patients that met the above criteria and were not included in the program.
Evaluation/measurement methods
The researchers used data elements from the study participants’ electronic medical records, TRMC-EMS Dispatch HF Screening tool, and CHIPs chart review. The control group data were established from billing data information. All data elements were reviewed retrospectively. Data elements were placed in a Microsoft Excel Spreadsheet. The data were then analyzed by Analyse-it software.
Results
The program identified a total of 53 patients of which 43 had successful interactions with the MIHS program. Of the nine patients that did not enter the program, 11.5% (n=6) did not respond on the date of the scheduled visit and could not be contacted, 3.8% (n=2) canceled the scheduled visit, and 3.8% (n=2) refused to schedule the visit, as they had other resources.
Of the 43 patients that interacted with the MIHS program, there was a majority of males (n=22, 51.2%) over females (n=21, 48.8%). Race was predominantly Hispanic (n=26, 60.5%), followed by African American (n=15, 34.9%), and white (n=2, 4.7%). The age range was between 36 years and 95 years. The majority of patients fell between the ages of 50 and 89 years, with the largest groups being patients 60–69 years (n=13, 30.2%) and 80–89 years (n=9, 20.9%).
The physical examination findings collected information on blood pressure, pulse rate, respiratory rate, blood oxygen saturation level (SPO2) readings, and lung sounds. The blood pressure of the group was primarily within normal limits (58.1%), however, 30.2% of the participants had high blood pressure. The pulse rates were 83.7% normocardic, with 7% revealing bradycardia, and 9.3% revealing tachycardia. A high percentage of patients (97.7%) had normal respiratory rates, with only one patient showing signs of tachypnea. This one patient was one of the patients that was readmitted within 30 days. There were 81.4% of patients with SPO2 percentages > 95%, and 11.6% had a reading <90%. The majority of patients had lung sounds that were clear to auscultation (76.7%), with the remaining patients having clinical presentations with rales, wheezes, and rhonchi (Table 1).
Table 1 Physical examination findings.
| Variable |
Segment |
Frequency |
Percentage |
| Blood Pressure |
High |
13 |
30.20% |
| |
Low |
5 |
11.60% |
| |
Normal |
25 |
58.10% |
| Pulse Rate |
Bradycardic |
3 |
7.00% |
| |
Normocardic |
36 |
83.70% |
| |
Tachycardic |
4 |
9.30% |
| Respiratory Rate |
Mild Tachypnea |
1 |
2.30% |
| |
Normal |
42 |
97.70% |
| SPO2 Range |
<90% |
5 |
11.60% |
| |
>95% |
35 |
81.40% |
| |
UTO |
3 |
7.00% |
| Lung Sounds |
Clear |
33 |
76.70% |
| |
Diminished |
1 |
2.30% |
| |
Rales |
3 |
7.00% |
| |
Rales& Rhonchi |
1 |
2.30% |
| |
Rhonchi |
2 |
4.70% |
| |
Wheeze |
3 |
7.00% |
A review of the symptomology of the patients in the MIHS program revealed patient complaints around dyspnea on exertion, orthopnea, episodes of dyspnea, chest pain, palpitations, poor appetite, and cough. There were 18.6% of patients who reported that they experienced dyspnea while resting; 48.8% reported that they experienced dyspnea on exertion; 37.2% reported experiencing orthopnea; 20.9% reported experiencing periods of dizziness; 16.2% reported episodes of chest pain; 11.6% experienced palpitations; 32.6% reported experiencing a chronic cough; and 79.1% felt they had a normal appetite (Table 2).
Table 2 Symptomology.
| Variable |
Segment |
Frequency |
Percentage |
| Dyspnea |
Yes |
8/43 |
18.60% |
| No |
35/43 |
81.40% |
| Dyspnea on Exertion |
Yes |
21/43 |
48.80% |
| No |
22/43 |
51.20% |
| Orthopnea |
Yes |
16/43 |
37.20% |
| No |
27/43 |
62.80% |
| Dizziness |
Yes |
9/43 |
20.90% |
| No |
34/43 |
79.10% |
| Episodes of Chest Pain |
Yes |
7/43 |
16.30% |
| No |
36/43 |
83.70% |
| Palpitations |
Yes |
5/43 |
11.60% |
| No |
38/43 |
88.40% |
| Appetite |
Normal |
34/43 |
79.10% |
| Poor |
9/43 |
20.90% |
| Cough |
Yes |
14/43 |
32.60% |
| No |
19/43 |
44.20% |
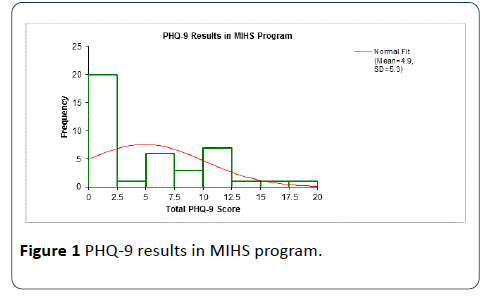
A review of social factors was also included in the MIHS program assessment. All of the patients had full service heat and electricity in the home. There were 95.3% (n=41) of patients who had a telephone; and 81% (n=35) had air conditioning. In the majority of cases, the environmental factors were not identified as an issue of concern. There were 93.0% (n=40) of patients who did not smoke; 95.3% (n=41) did not report using alcohol; and 97.7 (n=42) denied using recreational drugs. Of the patients, 86% (n=37) reported having access to adequate and appropriate food. A Patient Health Questionnaire (PHQ-9) for signs of depression was administered at the time of the MIHS home visit. The PHQ-9 scoring revealed that 46.5% (n=20) scored a zero, with the median score being 2.5, and the mean score 4.9. There was evidence of some severity of depression in the majority of the group (Figure 1).
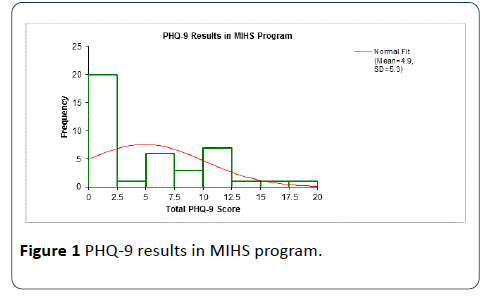
Figure 1: PHQ-9 results in MIHS program.
The MIHS program used identified issues in the social, symptomology, and physical assessments to educate patients. There were 90.7% (n=39) of patients who received general education on their disease; 79.1% (n=34) received education on food choices; 60.5% (n=26) received symptom management education; 65.1% (n=28) received education on weighing themselves daily; and 60.5% (n=26) received education on appropriate exercise.
Of the patients, 39.5% (n=17) needed additional follow up with the advanced practice nurse; and 23.3% (n=10) requested additional social service resources. Only 18.6% (n=8) of the patients accepted referrals to behavioral health resources (Figure 2).

Figure 2:MIHS – Days from discharge to MIHS visit.
MIHS visits occurred between four and 29 days postdischarge. The mean was 13.22 days (median=13.5, SD 5.056). Of the 43 MIHS program patients, three were readmitted for any cause within 30 days post-discharge from index HF admission for a rate of 6.9%. The readmission rate for a random control sample of 48 patients from the same geographic area during the same time period with the same index admission identified as HF was 22.9% (n=11/48). The MIHS sample was compared to the control sample using an independent t-test (95% CI). The results showed a mean difference of -0.2, SE.07, t statistic -2.19, DF=78.7, and twotailed p-value of .0316. There was no statistical difference for age, gender, or race.
Discussion
The data show that the influence of the MIHS program had a statistically significant effect as compared to the sample group. Although the concept of community paramedics is relatively new, the concept of community health workers is not. The CHW concept has shown positive clinical, cost effective results in multiple disease processes [8-10]. The potential of cross training EMS personnel as CHWs is feasible in a chronic disease population. The use of an existing resource supports the goals of the triple aim—better care, improved population health, and lower costs. The research also highlighted the effectiveness of interdisciplinary collaboration [18].
The clinical and social factors gathered and analyzed provided insight into the HF group. Many of the findings support what would be expected of the general HF population. One of the findings on the social assessment that stood out was the result of the PHQ-9. The findings that more than half of the MIHS HF population showed some level of depression highlighted an opportunity for behavioral health to interact with this group.
One of the limitations of this study was the small sample size. The researchers recommend continued study at a larger level. A second limitation of the study was the geographical constraints. The study was performed in an urban area with defined geographic boundaries. The geographical constraints also influenced the participants by race. The researchers suggest that the study be replicated in other geographic and racially diverse communities and groups.
Conclusion
The research supports the hypothesis that Emergency Medical Service resources can work on a multidisciplinary integrated care team to intervene for heart failure patients post-discharge with patient education and non-emergent interventions resulting in reduced 30-day readmissions. Further research is needed to ensure that the program is replicable and scalable and effective in different geographic and ethnic settings. The incidence of some form of depression in over half the HF population indicates the need for further research on the prevalence, incidence, and impact depression has on patients with HF.
Acknowledgements
The program was funded through a grant by Verizon.
Conflicts of Interest
The authors deny any conflicts of interest in regard to this research, authorship, or publication of this project/study.
Consent to Publish
The authors provide their consent to publish this manuscript.
11313
References
- Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, et al. (2013) Forecasting the impact of heart failure in the United States: A policy statement from the American heart association. Circ Heart Fail 6: 606-619.
- Vigen R, Maddox TM, Allen LA (2012) Aging of the United States population: Impact on heart failure. Curr Heart Fail Rep 9: 369-374.
- Bui AL, Horwich TB, Fonarow GC (2011) Epidemiology and risk profile of heart failure. Nat Rev Cardiol 8: 30-41.
- Stamp KD, Machado MA, Allen NA (2014) Transitional care programs improve outcomes for heart failure patients: An integrative review. J CardiovascNurs 29: 140-154.
- Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB (2011) The importance of transitional care in achieving health reform. Health Aff 30: 746-754.
- Naylor MD, Bowles KH, McCauley KM, MacCoy MC, Maislin G, et al. (2013) High value transitional care: Translation of research into practice. J EvalClinPract 19: 727-733.
- Stauffer BD, Fullerton C, Fleming N, Ogola G, Herrin J, et al. (2011) Effectiveness and cost of a transitional care program for heart failure: A prospective study with concurrent controls. Arch Intern Med 171: 1238-1243.
- Singh P, Chokshi D (2013) Community health workers: An opportunity for reverse innovation – Authors’ reply. The Lancet 382: 1327.
- Bhutta ZA, Lassi ZS, Pariyo G, Huicho L (2010) Global experience of community health workers for delivery of health related millennium development goals: A systematic review, country case studies, and recommendations for integration into national health systems. Global Health Workforce Alliance.
- Singh P, Sachs JD (2013) 1 million community health workers in sub-Saharan Africa by 2015. The Lancet 382: 363-365.
- National Highway Traffic Safety Administration (2007) National EMS scope of practice model [PDF].
- Misner D (2005) Community paramedicine: Part of an integrated healthcare system. EMS 34: 89.
- McTernan JL, Matthews E (2015) Measuring paramedics’ understanding of and attitude towards chronic diabetes care: A bridge to community health. J Community Med Health Educ 5: 328.
- Johnson K, (2011) Responding before a call is needed. New York Times pp A12.
- Wagner EH, Austin BT, Von Korff M (1996) Organizing care for patients with chronic illness. Milbank Q74: 511-544.
- Saczynski JS, Andrade SE, Harrold LR, Tjia J, Cutrona SL, et al. (2012) A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf 21: 129-140.