Ali Rashidi1, Walid Albanna1, John Jairo Gomez Gallego1, Josef Weyer2 and Ralf Buhl1*
1Department of Neurosurgery, Städtisches Klinikum Solingen, Solingen, Germany
2Department of General and Abdominal Surgery, Städtisches Klinikum Solingen, Solingen, Germany
*Corresponding Author:
Dr. Ralf Buhl
Department of Neurosurgery
Städtisches Klinikum Solingen
Solingen, Germany
Tel: 00492125472471
Email: buhl@klinikumsolingen.de
Received Date: February 06, 2018; Accepted Date: February 16, 2018; Published Date: February 20, 2018
Citation: Rashidi A, Albanna W, Gallego JJG, Weyer J, Buhl R (2019) Two Cases of Pneumorrhachis with Different Causes. Ann Clin Lab Res Vol.6: No.1: 220. DOI: 10.21767/2386-5180.1000220
Keywords
Pneumorrhachis; Case study; Two cases; Different causes; Pneumocephalus
Introduction
Pneumorrhachis (air within the spinal canal) is extremely rare. There are different causes described in the literature. There is traumatic origin and spontaneous development described. Also infectious association is reported. Prompt evaluation and diagnosis is very important [1]. In our Department of Neurosurgery within the last 2 years we treated 2 patients with pneumorrhachis who had a different origin of this rare disease.
Case Study
Case 1
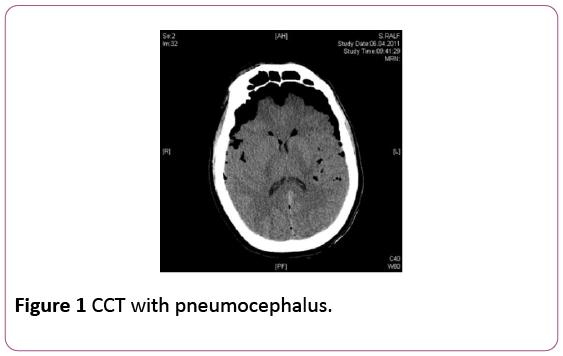
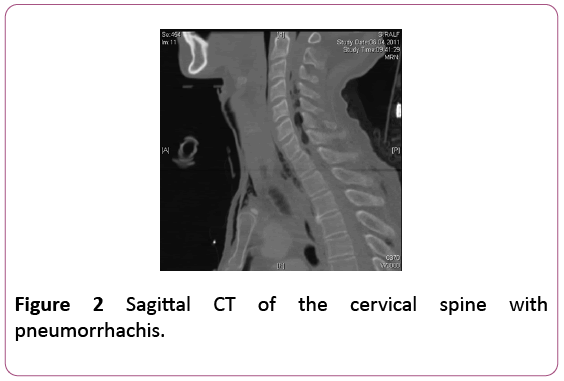
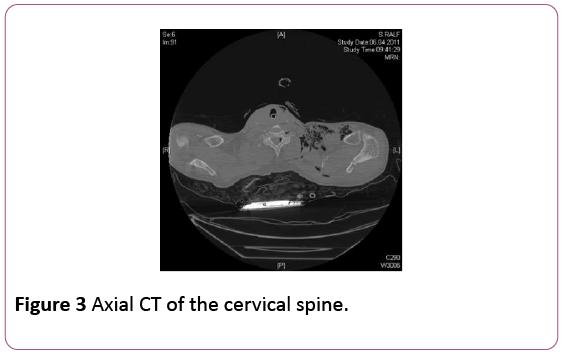
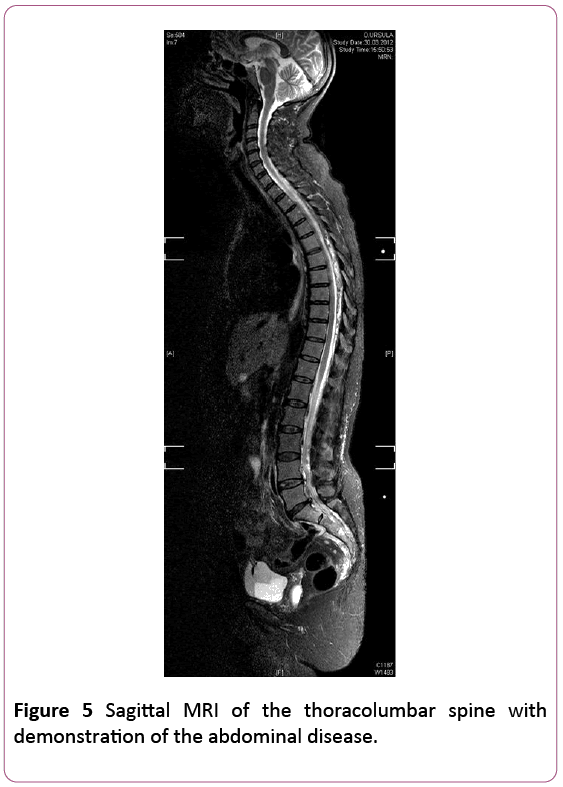
A 43-year-old male patient had a motor accident as a truck driver. He was fixed within the car about hours after the accident in an upright position. In the primary CT of his head and spine there was impressive pneumocephalus and pneumorrhachis within the cervical spinal canal (Figures 1-3).
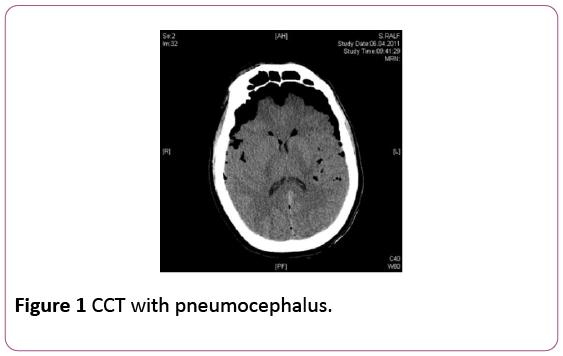
Figure 1: CCT with pneumocephalus.
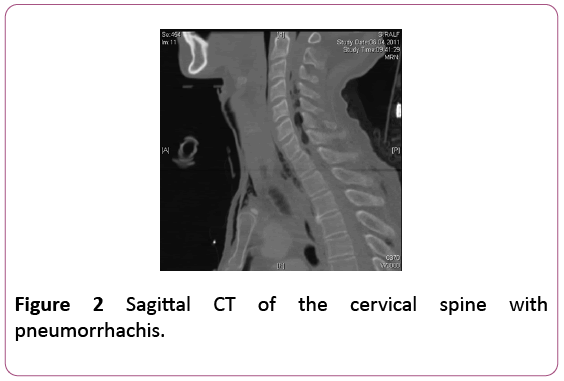
Figure 2: Sagittal CT of the cervical spine with pneumorrhachis.
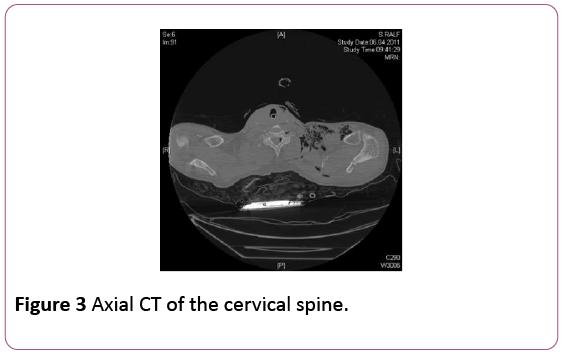
Figure 3: Axial CT of the cervical spine.
The treatment was conservative on Intensive Care Unit. 5 days after the accident he could be extubated. MRI of his cervical spine showed nerve root avulsions at C6 and C7 on the left side. Neurologically he showed a brachial plexus lesion on the left. The intracranial and intraspinal air resolved completely and the patient could be discharged to a rehabilitation center after 4 weeks.
Case 2
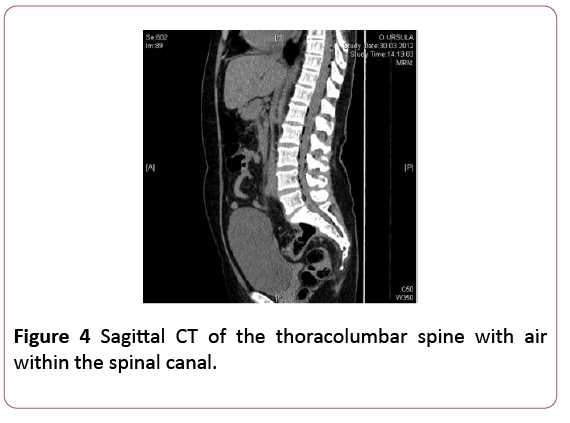
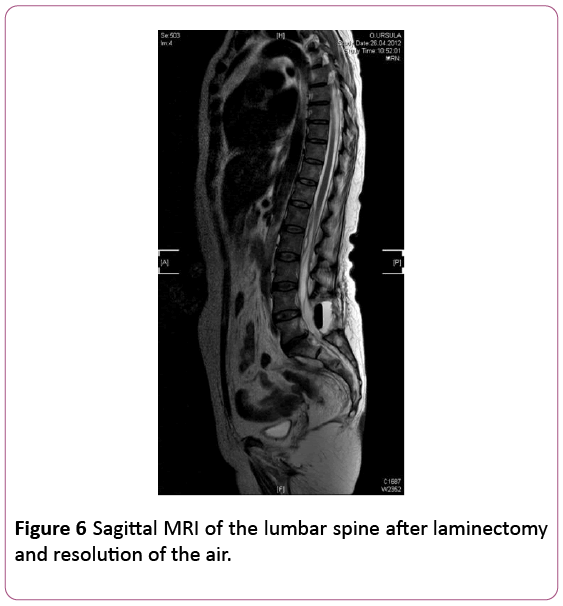
A 60-year-old female patient was admitted in our hospital with acute low back pain, radicular pain and bladder dysfunction. The neurological examination showed a tibialis anterior paresis (MRC grade 4) on the left side. On admission the patient had pyrexia, a GCS of 15. Her blood tests showed a raised C-reactive Protein of 29.9. She had a past surgical history of sigmoidal diverticulitis. A CT-Scan (Figure 4) and MRI-scan (Figures 5 and 6) of her spine showed extensive intracranial intraspinal air. A MRI-scan demonstrated also a large collection of gas in the presacral space which tracked into the intraspinal space.
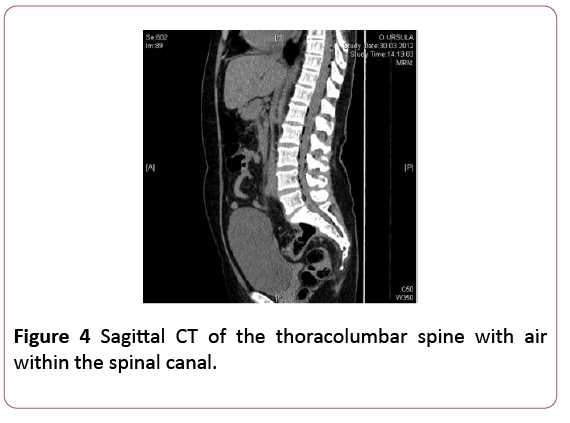
Figure 4: Sagittal CT of the thoracolumbar spine with air within the spinal canal.
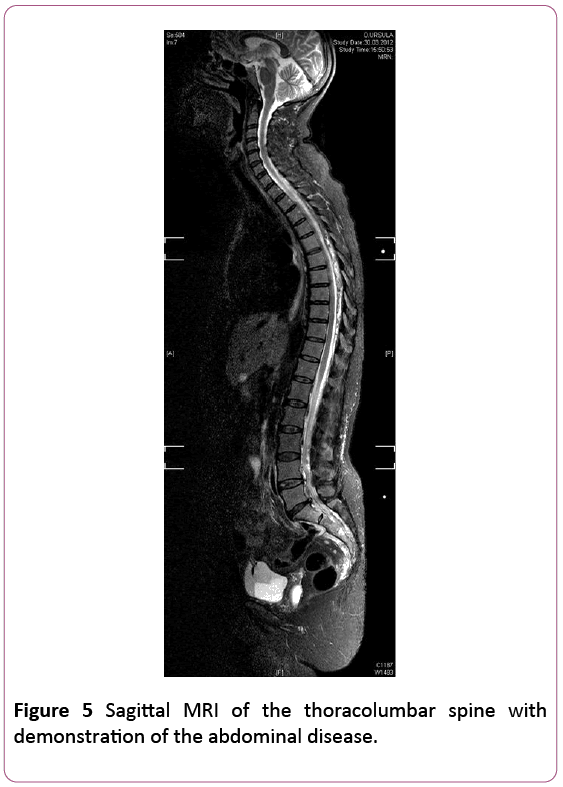
Figure 5: Sagittal MRI of the thoracolumbar spine with demonstration of the abdominal disease.
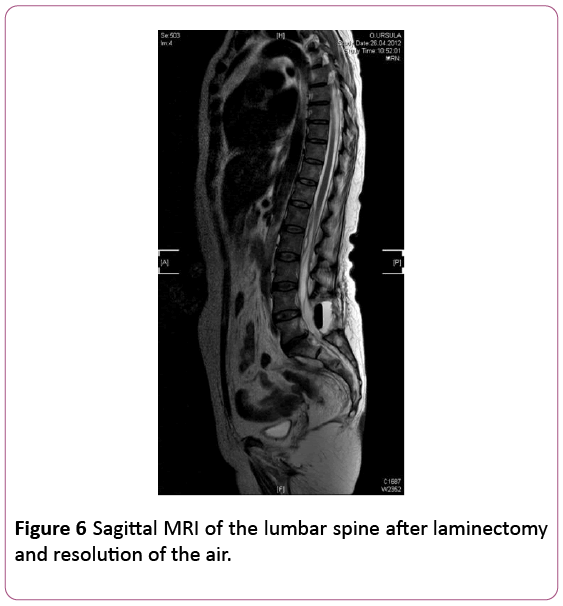
Figure 6: Sagittal MRI of the lumbar spine after laminectomy and resolution of the air.
On the next day the neurological deficit worsened to paraplegia of the lower extremities. MRI of the lumbar spine showed an abscess in the retroperitoneal space with intraspinal extension. The patient was immediately operated on in a combined setting of neurosurgeons and abdominal surgeons; a laminectomy L4 was performed to drain the intraspinal abscess, anterior rectum resection with a colostomy and an appendectomy were performed. The patient was treated antibiotically. Two weeks later massive pus came out of the lumbar wound. She was therefore operated once more, whereby the pus collection was drained and a drain was left behind to be flushed over regularly. In the following days the patient improved clinically and neurologically. Follow-up imaging demonstrated improvement of the inflammatory changes.
The patient was transferred to a rehabilitation center specialized in spinal cord injuries. By discharge she had a paresis of the right leg MRC grade 2 and could move her toes on the left side. At follow-up examination six months later she is able to walk with assistance.
Discussion
Pneumorrachis is a rare phenomenon, where air enters the spinal canal. Free air surrounding the dura mater spinalis (pneumorrachis) present in the intradural or extradural compartments is a rarely described phenomenon [2,3]. Pathogenesis and aetiologies of pneumorrhachis are multifold and can be a diagnostic challenge. It is a rare and exceptional finding. Usually the treatment is conservative [4]. Oertel et al. also presented a patient with cervical pneumorrhachis after head injury. In our first case also the patient had a motor accident as a truck driver. He was fixed within the car about hours after the accident in an upright position so the air might have distributed during that time. Gelalis et al. [5] performed a systematic review of the literature (37 articles with 44 cases). Treatment is individual. Subarachnoid pneumorrhachis is a marker of severe injury.
Pneumorrachis can rarely cause symptoms of spinal cord compression and may require urgent decompressive surgery [6]. Song and Lee performed a laminectomy of C7 in a patient with progressive weakness of his legs [7].
Intraspinal air can be divided into primary and secondary pneumorrachis, classified into extra- or intradural pneumorrachis and aetiologically subsumed into iatrogenic, traumatic and nontraumatic [6,8-12]. Pneumorrachis is thought to be associated with an increased morbidity and mortality [13]. The condition could also be seen after traumatic brain injury, especially with skull base and sinus fractures. Pneumorrhachis after skull base fracture is described by Inamasu et al. [14], Bozkurt et al. [15] and Arora et al. [16]. Pneumorrhachis can be classified as epidural or subarachnoid space pneumorrhachis [17,10]. Goh and Yeo [10] presented a case of entire pneumorrhachis due to isolated head trauma. Cayli et al. [18] described air within the cervical subarachnoid space due to traumatic pneumocephalus. Harandou et al. [2] described a 37 year old patient with a motor vehicle accident. CT showed bilateral hemothorax, rib fractures and fracture of the 4th vertebra associated with air in the spinal canal extending from T6 to L2. Chibbaro et al. [19] reported pneumorrhachis extending through the entire spinal canal in a patient who was involved in a road traffic accident who had no apparent major bone and soft tissue injuries. These cases show the different individual findings.
Also pediatric cases are published. Silver et al. [20] presented a 3 weeks old girl after an automobile accident. In this case pneumorrhachis developed after jejunal entrapment by a fracture dislocation of L2.
Derner et al. [21] published an interesting case of a 41-yearold man with thoracic trauma and avulsion of brachial plexus. On admission they found pneumorrhachis at the cervicothoracic transition with normal skull and brain. After 5 days CT Scan showed right frontal pneumocephalus and MRI on the 10th day showed nerve root pneumomeningocele at the level of C7 and C8.
Less common causes included primary spinal sources, visceral injuries, and fulminant infections. Kirzner et al. [22] found air within the spinal canal of a diabetic woman who had fever and back pain. With the help of CT there was detection of de novo gas formation within an epidural abscess. Rehman et al. [23] presented 2 cases with abdominal emergencies (emphysematous pyelonephritis and bowel gangrene). In these cases they stated that pneumorrhachis could be a sign of poor prognosis. Amit et al. [24] presented a 60-year-old man with meningism and reduced conscious level. Imaging demonstrated a perforated sigmoid colon with retroperitoneal air associated with pneumorrhachis and pneumocranium. He required a Hartmann´s procedure and broad spectrum intrathecal antibiotics which led to resolution of the pneumorrhachis and pneumocranium. In our second case also a perforation of sigmoid diverticulitis and fistula led to the development of intraspinal air and spinal abscess.
Conclusion
In most published cases, pneumorrachis was not associated with any spinal cord symptoms, not tend to migrate and reabsorbs spontaneously.
Intraspinal gas can be found in combination with associated gas distribution in other compartments of the body such as pneumocephalus, pneumothorax, pneumomediastinum, pneumopericardium or subcutaneous emphysema [6,8,11,13]. Ristagno et al. [25] presented a case of pneumorrhachis following resection of lung carcinoma. Intraspinal epidural air collection developed following a sudden resolution of subcutaneous emphysema.
Another route of intraspinal entry outside of traumatic and iatrogenic cause may be due to gas dissecting indirectly between the paraspinal soft tissues into the epidural space of the spinal canal via the neural foramina and along the vascular and nerve root sheaths [16,24].
The therapy of pneumorrachis is in most cases conservative or treatment of underlying causes. Oxygen therapy was sometimes used with the concept that oxygen may facilitate air absorption [6].
21886
References
- Chaichana KL, Pradilla G, Witham TF, Gokaslan ZL, Bydon A (2010) The clinical significance of pneumorachis: A case report and review of the literature. J Trauma68: 736-744.
- Harandou M, Khatouf M, Kanjaa N, Adnet F, Lapostolle F (2005) Intraspinal air, a rare complication of blunt chest trauma. Ann Fr Anesth Reanim 24: 421-424.
- Hasni Bouraoui I, Gamoun W, Mrad Dali K, Boughammoura H, Hmila S, et al. (2010) Pneumorachis: report of three rare causes. J Radiol 91: 495- 499.
- Oertel MF, Korinth MC, Reinges MHT, Krings T, Terbeck S, et al. (2006) Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J 15:636-664.
- Gelalis ID, Karageorgos A, Arnaoutoglou C, Gartzonikas D, Politis A, et al. (2011) Traumatic pneumorrhachis: Etiology, pathomechanism, diagnosis and treatment. Spine J 11:153-157.
- Al-Mufarrej F, Gharagozloo F, Tempesta B, Margolis M (2009) Spontaneous cervicothoracolumbar pneumorrhachis, pneumomediastinum and pneumoperitoneum. Clin Respir J 3:239-243.
- Song KJ, Lee KB (2009) Spontaneous extradural pneumorrhachis causing cervical myelopathy. Spine J 9:16-18.
- Belotti EA, Rizzi M, Rodoni-Cassis P, Ragazzi M, Zanolari-Caledrerari M, et al. (2010) Air within the spinal canal in spontaneous pneumomediastinum. Chest 137: 1197-1200.
- Dimar JR 2nd, Smail J, Carreon LY (2010) Traumatic pediatric pneumorachis: case report and review of the literature. Spine 35:E860-863.
- Holton LH, Migaly J, Rolandelli RH (2002) Pneumorrhachis, subcutaneous emphysema, pneumomediastinum, pneumopericardium, and pneumoretroperitoneum after proctocolectomy for ulcerative colitis: report of a case. Dis Colon Rectum 45:567-570.
- Yousaf I, Flynn P, McConnell R (2003) Symptomatic intraspinal pneumocele resulting from closed head injury. Br J Neurosurg 17: 248-249.
- Coniglio M, De Santis M, Pizzi G, Francioni F, Ricci P (1997) Pneumorachis associated with spontaneous pneumomediastinum. A case report. Radiol Med 94: 531-532.
- Inamasu J, Nakamura Y, Saito R, Kuroshima Y, Ichikizaki K (2002) Air in the spinal canal after skull base fracture. Am J Emerg Med 20: 64-65.
- Bozkurt G, Turk CC, Ayhan S, Akbay A, Palaoglu S (2011) Cervical pneumorrhachis caused by impact loading forces after skull base fracture: case report and review of the literature. Cent Eur Neurosurg 72: 215-218.
- Arora S, Aggarwal P, Cheema GS, Singla J (2011) Pneumorachis of the cervical spine with associated pneumocephalus and subcutaneous emphysema. Indian J Orthop 45: 372-375.
- Coskun S, Sahin M, Cobanoglu M, Kilicaslan I (2009) Entire pneumorrhachis due to isolated head trauma. Am J Emerg Med 27: 902-906.
- Cayli SR, Kocak A, Kutlu R, Tekiner A (2003) Spinal pneumorrhachis. Br J Neurosurg 17: 72-74.
- Chibbaro S, Selem M, Tacconi L (2005) Cervicothoracolumbar pneumorachis. Case report and review of the literature. Surg Neurol 64: 80-82.
- Silver SF, Nadel HR, Flodmark O (1988) Pneumorrhachis after jejunal entrapment caused by a fracture dislocation of the lumbar spine. AJR 150: 1129-1130.
- Derner M, Drugova B, Horejsi L, Skvara D, Druga R (2011) Massive pneumorrhachis, pneumocephalus and pneumoopticus following thoracic trauma and avulsion of the brachial plexus: Case report and review of the literature. Prague Med Rep 112: 56-66.
- Kirzner H, Oh YK, Lee SH (1988) Intraspinal air: A CT finding of epidural abscess. AJR 151: 1217-1218.
- Rehman TA, Mammen T, Thaj J, Cherian RS (2009) Is pneumorrachis a poor prognostic sign in acute gangrenous abdominal emergencies? Emerg Radiol 16: 151-154.
- Amit A, Toll EC, Siddique S, Nelson RJ (2011) Pneumorrhachis with pneumocranium: An unusual complication of intra-abdominal sepsis. Br J Neurosurg 25: 111-112.
- Ristagno RL, Hiratzka LF, Rost RC Jr (2002) An unusual case of pneumorrhachis following resection of lung carcinoma. Chest 121: 1712-1714.