Keywords
Adult males; Bladder outlet obstruction; Rethrograde urethrography; Ultrasonography
Introduction
Bladder outlet obstruction (BOO) is a urological condition where the urine flow from the urinary bladder through the urethra is impeded. The hallmark of bladder outlet obstruction is urinary retention which may be acute or chronic. Urinary retention is a common urological problem seen worldwide, predominantly in the elderly [1,2]. The incidence increases with age so that a man in his 70s has 10% chances and a man in his 80s has more than 30% chances of having episode of acute urinary retention [1,2].
The burden of BOO is high in Africa with attendant poor quality of life. World Health Organization (WHO) in 2011 presaged that by 2018 about 2.3 billion individuals worldwide would be affected by Lower Urinary Tract Symptoms (LUTS) and 1.1 billion men would have symptoms of bladder outlet obstruction (BOO) [3,4]. It was further postulated that the greatest burden of BOO associated LUTS would be in the developing regions of Africa with a projected increase of 31.1% between 2008 and 2018 [3,4].
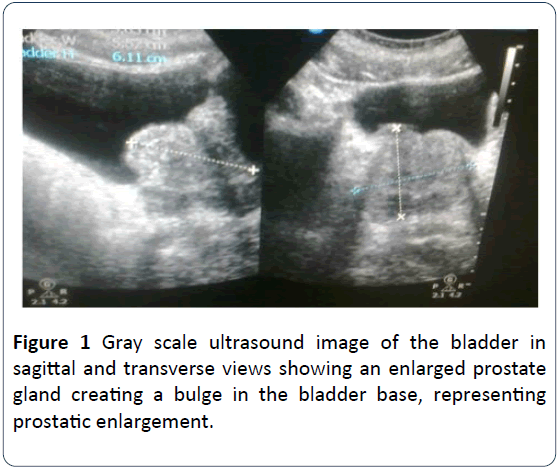
A considerable number of aetiologies are responsible for bladder outlet obstruction in men and these may include anatomical obstructions from benign prostatic hyperplasia (BPH) (Figure 1), carcinoma of the prostate, bladder cancer, urethral stricture, iatrogenic causes such as intraurethral injection of bulky agents in the treatment of intrinsic sphincter deficiency (ISD) and also psychogenic causes [5,6]. Other aetiological causes include bladder calculi, urethral calculi, cystocele, posterior urethral valves, urethral spasms, urethral diverticulum and neurogenic bladder.
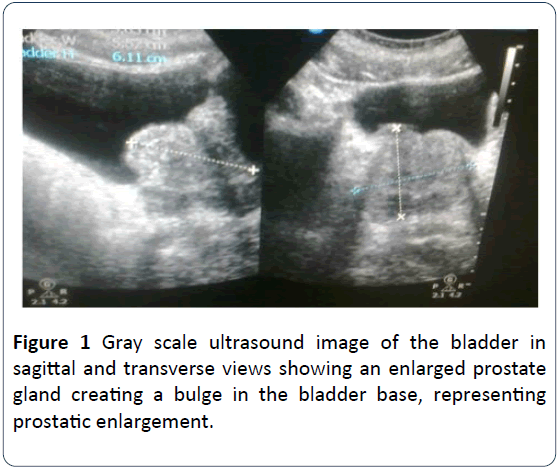
Figure 1: Gray scale ultrasound image of the bladder in sagittal and transverse views showing an enlarged prostate gland creating a bulge in the bladder base, representing prostatic enlargement.
The issue of how to accurately evaluate BOO in men with LUTS has been debated for decades because of its complex aetiological factors [7-9]. A number of studies have suggested that a considerable proportion of men presenting with suspected outflow obstruction are not obstructed as determined by pressure flow criteria [10]. Thus when considering management of men with LUTS suggestive of BOO, it is important to take into account the aetiological entities of BOO.
BOO induced LUTS may be predominantly obstructive, irritative, or often a combination of both. Typically obstructive symptoms include hesitancy, incomplete bladder emptying, poor urinary stream and post voidal urinary dribbling. Irritative complaints include urinary urgency, frequency of urination, occasional dysuria, and nocturia. Obstruction can be functional due to Detrusor-Sphincter Dyssynergia (DSD). BOO may also occur in the complete absence of symptoms and can manifest for the first time as urinary retention or decompensation of the upper urinary tracts [11].
Increased outlet resistance as seen in patients with bladder outlet obstruction is the commonest mechanism of urinary retention. It may result in bladder hypertrophy, dilatation, trabeculations, sacculations and diverticulations. Bladder changes may also result in functional failure of ureterotrigonal complex, resulting in vesicoureteric reflux, with the resultant back pressure on the ureters and collecting system leading to the development of hydroureters and hydronephrosis. With time, persistently elevated intrarenal pressure may lead to tubular epithelial atrophy and eventual nephron loss. The functional consequence is impaired glomerular function and eventual chronic renal failure [11]. Long term or high grade bladder outlet obstruction can permanently damage all parts of the urinary system. The incidence and economic burden is not known in our setting, yet, it is a common urologic problem [3,12,13].
Early diagnosis of the cause and treatment of BOO is necessary to avert its long term complications. Despite the advances in cross sectional imaging such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI), Ultrasonography remains a first line modality for imaging the pelvic structures such as the urinary bladder and its base. Ultrasound is the most commonly used diagnostic imaging modality, accounting for approximately 25% of all imaging examinations performed worldwide at the beginning of the 21st century [14]. The success of ultrasound may be attributed to a number of attractive characteristics, including the relatively low cost and portability of an ultrasound scanner, the non-ionizing nature of ultrasound waves, the ability to produce real time images of blood flow and moving structures such as the beating heart, and the intrinsic contrast among soft tissue structures that is achieved without the need for an injected contrast agent [14]. There are many imaging tools for the assessment of the bladder outflow tract (Urethra) but retrograde urethrography is considered first in the imaging armamentarium.
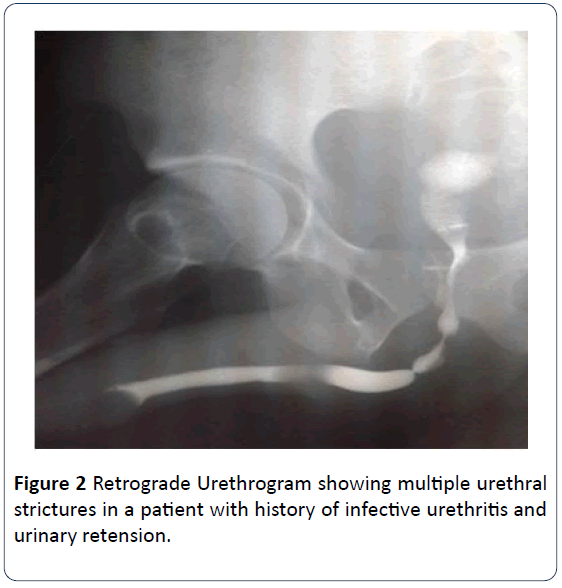
Retrograde urethrography (RUG) and voiding cystourethrography (VCUG) are the modalities of choice for imaging the urethra. Retrograde urethrography a time-tested imaging technique remains the best initial investigation for urethral and periurethral imaging in men and is indicated in the evaluation of urethral injuries, strictures (Figure 2), and fistulas [15,16]. It facilitates proper definition of the location, length, number, and degree of strictures as well as the periurethral abnormality. The sensitivity of RUG in the evaluation of urethral strictures is about 75–100% with specificities in the range of 72–97% [17]. Retrograde urethrography is a straightforward easy to perform, readily available, reproducible and cost-effective examination that can detect clinically relevant strictures involving the anterior urethra as well as those with extension into the membranous urethra [18-20]. RUG may be combined with Voiding Cystourethrography (VCUG) for the evaluation of posterior urethra.
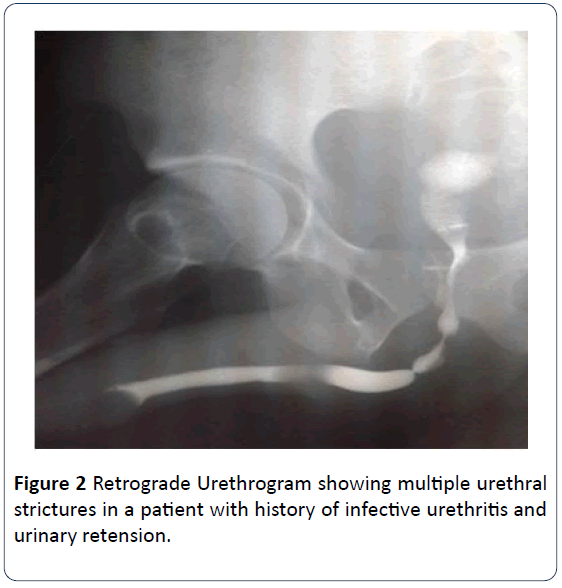
Figure 2: Retrograde Urethrogram showing multiple urethral strictures in a patient with history of infective urethritis and urinary retension.
A considerable number of aetiological factors are responsible for BOO in males, some of which depend on the age and others varies from place to place. Understanding and categorizing these factors are crucial for Clinicians especially surgeons in resource limited environment to be conversant with the pattern of bladder outlet obstruction in their setting so as to rationally approach the differential diagnosis as well as offer appropriate management. To the best of our knowledge, there is paucity of studies on BOO in our setting. This study was designed to assess the aetiological factors of Bladder Outlet Obstruction (BOO) using ultrasonography and retrograde urethrography, in adult males in Port Harcourt Rivers State, Nigeria.
Materials and Methods
Study design
A prospective cross sectional approach was adopted for this study, which lasted for a period of one year from February 2014 to January 2015.
Study setting
The study was conducted in the department of radiology of Braithwaite Memorial Specialist Hospital, currently known as Rivers State University Teaching Hospital, Port Harcourt.
Sample size and sampling technique
The sample size was determined using the standard sample size estimation formula (Kish formula) [21].
N= Z2PQ/D2
Where N= sample size
Z= standard normal deviation=1.96, corresponding to 95% confidence level.
P= prevalence of population possessing attribute of interest (15%).
15%= 0.15
Q= 1-p Hence Q=1-0.15=0.85.
D= tolerable error (usually 0.05)
N=((1.96)²X0.15X0.85)/(0.05)²=196
Therefore, N=196
In order to allow for attrition, a sample size of 216 was used.
A purposive sampling technique was used for selection of 216 adult male patients aged between 20 to 80 years referred from Urology Department and other peripheral hospitals to the Department of Radiology for investigation on account of obstructive urinary symptoms based on the inclusion and exclusion criteria set for this study.
Inclusion Criteria and Ethical Considerations
All adult males with age range 20-80 years that presented with symptoms of BOO were included in this study, while all those that have acute urethritis, diabetic conditions and paraplegic were excluded, including those that do not meet the aforementioned inclusion criteria.
Prior to this study, ethical approval was obtained from the Ethical Review Committee (ERC) of Braithwaite Memorial Specialist Hospital, Port Harcourt, and Rivers State, Nigeria. Informed consent was also taken from all the patients who participated in the study they were reassured about the confidentiality of the data and in order to protect their rights, the names of the volunteers were not required. They were also informed that they reserve the right to withdraw from the study at any time if the so decide.
Methodology
All procedures for the investigations were adequately explained to the participants, and then the age and indication for the study were recorded. The ultrasound investigations were performed using standard protocols and techniques for transpubic scans using Real time GE Logic P6 PRO gray scale, 3D machine fitted with a 3.5 MHz sector transducer. All patients had transpubic ultrasound scan to identify the anatomic causes of BOO and where no obvious cause was found but post-voidal residual urine volume was significant. The volume of residual urine considered to be significant in this study was 50 ml, which is obtainable in other literature [21,22]. Standard protocols and techniques were adopted for Retrograde Cystourethrography (RUG) investigation for the evaluation of the urethra in patient with suspicious urethral pathology and there was significant post-voidal residual urine volume on ultrasound scan.
Data Collection and Analysis
Data such as age and radiological findings were collected using a structured proforma. Descriptive (mean, standard deviation, frequency table and percentage) statistic was used for statistical analysis using statistical package for social sciences (SPSS) version 21(SPSS Inc Chicago., ILL USA).
Results
Out of 216 adult male patients with mean age of 62.3 ± 11.23 years (range 20-79 years) included in this study, 64% (n=138) had prostatic enlargement as highest, followed by urethral stricture 17.12% (n=37) and the least were adult posterior urethral valve (APUV) and diverticulum, which is 0.5% (n=1) each respectively (Table 1).
Table 1 Summary of findings on ultrasound and retrograde urethrogram.
| Disease Condition |
Frequency |
Percentage (%) |
| Prostatic enlargement |
138 |
63.9 |
| Bladder calculi |
10 |
4.6 |
| Bladder tumor |
4 |
1.9 |
| Urethral structure |
37 |
17.1 |
| APUV |
1 |
0.5 |
| Urethral diverticulum |
1 |
0.5 |
| Normal RUG |
25 |
11.6 |
| Total |
216 |
100 |
Of the total subjects studied, 39.35% (n=83) were within age group 60-69 years of age as highest, followed by age group 70-79 years 29.17% (n=65) and the least were within age group 20-29 years, which is 1.85% (n=4) (Table 2). Out of 83 subjects within age group 60-69 years, 72.3% (n=60) had prostatic enlargement as highest, followed by urethral stricture 8.43% (n=7) and none had APUV as causes of BOO in our study (Table 2).
Table 2 This table illustrates the distribution of aetiological factors of BOO with age.
| Disease Conditions |
| Age |
Prostatic Enlargement |
Bladder Calculi |
Bladder Tumor |
Urethral Stricture |
APUV |
Urethral Diverticulum |
Normal RUG |
Total |
Percentage |
| 20-29 |
|
1 |
|
3 |
|
|
|
4 |
1.85% |
| 30-39 |
|
|
|
5 |
1 |
|
|
6 |
2.78% |
| 40-49 |
6 |
1 |
|
10 |
|
|
|
17 |
7.87% |
| 50-59 |
26 |
1 |
1 |
10 |
|
|
3 |
41 |
18.98% |
| 60-69 |
60 |
4 |
3 |
7 |
|
1 |
8 |
83 |
39.35% |
| 70-79 |
46 |
3 |
|
2 |
|
|
14 |
65 |
29.17% |
| Total |
138 |
10 |
4 |
37 |
1 |
1 |
25 |
216 |
100 |
Discussion
In this study, the most common cause of BOO in adult men is enlargement of the Prostate, which is also known as Benign Prostatic Hyperplasia (BPH). This corroborates the findings from other parts of Nigeria and the world [11,23-28]. It is a highly prevalent disease of older men and is the result of unregulated neoplastic growth of the prostate gland. Prostate size taken as significant in this study is 40 cm3. This is in keeping with findings of previous studies conducted by Elterman et al. [29], Rosier et al. [30] and Rosier et al. [31], which documented that men with prostate volumes >40 cm3 have a 70% chance of being diagnosed with BOO. Prostate volume as a predictor of BOO in men with glands <40 cm3 is not helpful [26]. Also in this study, urethral stricture as an aetiological cause of BOO accounted for 17.12%. There is currently progressive increase in the incidence of BOO due to urethral strictures. This was attributed to the increased trauma related urethral strictures [32], number of permanent catheter bearers, the surge of sexually transmitted disease (STDs) incidence, and misuse of transurethral diagnostic or therapeutic instrumentation [18,33-35].
In our study, majority of the subjects were within the sixth and seventh decades of ages, which accounted for 68.52%. The age of the patient found with significant prostate size causing BOO ranges from 40years and above. This is similar to the study conducted by Briganti et al. [36], which also noted that the incidence of BPH as well as the presence of bothersome lower urinary tract symptoms (LUTS) increase with age and these conditions are highly prevalent as early as beyond the fourth decade. In this study, urethral strictures as a cause of BOO was found highest within age groups 40-49 and 50-59 years. This is in similar with the finding of a study conducted by Ahidjo et al. [18], which also reported urethral stricture as a cause of BOO to be more common among males within the age group 40-45 years.
In this study, adult posterior urethral valve is one of the least causes of BOO, which accounted for only 0.5% and it was noted in a patient within age group 30-39 years. Although, Young et al. [37], reported that exact age of presentation is not known and varies greatly. Posterior Urethral valve is a rare cause of BOO in adults and it has been estimated that it accounts for 10% of PUV cases. Posterior Urethral valves are the commonest cause of urinary obstruction in neonates, but when detrusor contraction overcome obstruction it may remain silent until later life [38,39]. Recurrent UTI and obstructive uropathy are sequelae of adult posterior urethral valve. Cases of urethral diverticulum are rare in males [40-42]. Most urethral diverticuli (90%) are acquired while less than 10% are truly congenital in origin [42]. Urethral Diverticulum was seen in 1 patient accounting for 0.5% in this study.
Study Limitations
All cases of enlarged prostate were considered to be benign prostatic hyperplasia because biopsy was not done in any of them. No patient diagnosed with BPH on transpubic ultrasound scan had the privilege of having retrograde urethrogram done as well.
Conclusion
Bladder Outlet Obstruction is multi-aetiological and prostatic enlargement tops the list of pathologies causing BOO in adult male patients, followed by urethral structure. The aetiologies of BOO varies with age as shown in this study; while benign prostatic enlargement was commonly found in elderly patients and urethral structure was predominant in younger adults.
Recommendations
Transpubic Ultrasonography and Retrograde urethrography are recommended for the initial investigation of adult males presenting with symptoms of urinary obstruction. It is recommended that various strategies for the prevention of the causes of BOO should be formulated especially for those common causes that could be easily prevented. Considering the magnitude of BOO in the society with its resultant complications, further studies may be required to document its incidence and burden.
24701
References
- Kapln SA, Wein AJ, Staskin DR, Roehrborn CG, Steer WD (2008) Urinary retention and post void residual volume in men: separating truth from tradition. J Urol 180: 47-54.
- Mitchel JP (1984) Management of chronic urinary retention. Br Med J Clin Res Ed 289: 515-516.
- Irwin D, Kopp ZS, Agatep B, Milsom I, Abrams P (2011) Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction Br J Urol Int 108: 1132-1138.
- Wei JT, Calhoun E, Steven J (2008) Urologic diseases in America project: benign prostatic hyperplasia. J Urol 179: S75-80.
- Jacobson SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, et al. (1997) Natural history of prostatism: Risk factors for acute urinary retention. J Urol 158: 481-487.
- Tanagho EA, Bella AJ, Lue TF (2008) Neuropathic bladder disorders. In Smiths general urology. (17th edn.). Tenagho E A, McAninch J W, (Eds). San Fransisco Lange Medical Books/ McGraw-Hill pp: 438-453.
- Boormans JL, van Venrooij GE, Boon TA (2007) Invasively estimated International Continence Society obstruction classification versus noninvasively assessed bladder outlet obstruction probability in treatment recommendation for LUTS suggestive of BPH. Urology 69: 485-490.
- Ozawa H, Chancellor MB, Ding YY, Nasu Y, Yokoyama T, et al. (2000) Noninvasive urodynamic evaluation of bladder outlet obstruction using Doppler ultrasonography. Urology 56: 408-412.
- Nitti VW (2005) Pressure flow urodynamic studies: the gold standard for diagnosing bladder outlet obstruction. Rev Urol 6: S14-S21.
- Reynard JM, Abrams P (1995) Bladder outlet Obstruction assessment of symptoms. World J Urol 13: 3-8.
- Dmochowski RR (2005) Bladder outlet obstruction: etiology and evaluation. Rev Urol 6:S3-S13.
- World Health Organization (2002) The world health report 2002: Reducing risks, promoting healthy life. World Health Organization.
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (2006) Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 367: 1747-1757.
- Dance DR, Christofides S, Maldment ADA, Mclean ID, Ng KN (2014) Diagnostic radiology physics: A handbook for teachers and students; International atomic energy agency, Vienna. pp: 291-293.
- Amis ES, Newhouse JH, Cronan JJ (1988) Radiology of male periurethral structures. AJR Am J Roentgenol 151: 321-324.
- Sandler CM, Corriere JN (1989) Urethrography in the diagnosis of acute urethral injuries. Urol Clin North Am 16: 283-289.
- Angermeier KW, Rourke KF, Dubey D, Forsyth RJ, Gonzalez CM (2014) SIU/ICUD Consultation on Urethral Strictures: Evaluation and follow-up. Urology 83: S8-17.
- Ahidjo A, Abdulkadir AY, Gadams IA, Saad ST (2012) Evaluation of radiographic pattern of male urethral strictures in Nigeria: A preliminary report of a proposed new scoring system for developing countries. Iran J Radiol 9: 60-62.
- Goldman SM, Sandler CM, Corriere JN, McGuire EJ (1997) Blunt urethral trauma: a unified, anatomical mechanical classification. J Urol 157: 85-89.
- Gupta SK, Kaur B, Shulka RC (1991) Urethro-venous intravasation during retrograde urethrography (report of 5 cases). J Postgrad Med 37: 102-104.
- Araoye MO (2004) Research methodology with statistics for health and social sciences; (1st edn.). Nathadex: pp: 1-286.
- Stevens E (2005) Bladder ultrasound: avoiding unnecessary catheterizations. Med Surg Nurs 14: 249-253.
- Kolman C, Girman CJ, Jacobsen SJ, Lieberman MM (1999) Distribution of post-void residual urine volume in randomly selected men. J Urol 169: 122-127.
- Min-Yong K, Ku J, Seung-June O (2010) Non-invasive parameters predicting bladder outlet obstruction in korean men with lower urinary tract symptoms. J Korean Med Sci 25: 272-275.
- Gyasi-Sarpong CK, Ta-angYenli EM, Idriss A, AppiahArhin A, Aboah K, et al. (2012) Bacterial urinary tract infections among males with lower urinary tract obstruction at komfo anokye teaching hospital, Kumasi, Ghana. Open J Urol 2: 131-136.
- Muhammed A, Abubakar A (2012) Pathophysiology and management of urinary retention in men Arch Int Surg 2: 63-69.
- Stamatiou K (2009) Management of benign prostatic hypertrophy-related urinary retention, current trends and perspective. Urol J 6: 237-244.
- Shimizu N, Matsumoto S, Yoshioka N, Hanai T, Sugiyama T, et al. (2006) Clinical study of Acute Urinary Retention. Japanese J Urol 97: 839-843.
- Elterman DS, Chughtai B, Lee R, Te AE, Kaplan SA (2013) Non-invasive methods to evaluate bladder outlet obstruction in men. Int Braz J Urol 39: 1-10.
- Rosier PF, de Wildt MJ, Wijkstra H, Debruyne FF, de la Rosette JJ (1996) Clinical diagnosis of bladder outlet obstruction in patients with benign prostatic enlargement and lower urinary tract symptoms: development and urodynamic validation of a clinical prostate score for the objective diagnosis of bladder outlet obstruction. J Urol 155: 1649-1654.
- Rosier PF, de La Rossette (1995) Is there a correlation between prostate size and Bladder Outlet Obstruction? World J Urol 13: 9-13.
- Mbaba AN, Ogolodom MP, Abam R, Wekhe C, Akhigb RO, et al. (2019) Pattern of urethral stricture disease in adult males referred for retrograde urethrography in Port Harcourt metropolis, Rivers State, Nigeria. IJBPAS 8: 1545-1556.
- Romero PP, Llinares MA (2004) Male urethral stenosis: review of complications. Arch Esp Urol 57: 485-511.
- Steenkamp JW, de Kock ML (1994) Epidemiology of urethral stricture at Tygerberg Hospital. S Afr Med J 84: 267-268.
- Kochakarn W, Muangman V, Viseshsindh V, Ratana-Olarn K, Gojaseni P (2001) Stricture of the male urethra: 29 years’ experience of 323 cases. J Med Assoc Thai 84: 6–11.
- Briganti A, Capitano U, Suardi N, Gallina A, Salonia A et al. (2009) Benign prostatic hyperplasia and its aetiologies. Eur Urol Suppl 8: 865-871.
- Young HH, Frontz WA, Baldwin JC (2002) Congenital obstruction of the posterior urethra. J Urol 167: 265-268.
- Atwell JD (1983) Posterior urethral valves in the British Isles. A multicenter BAPS review. J Padiatr Surg 18: 70-74.
- Opsomer RJ, Wese FX, Dardenne AN, Van Caigh PJ (1990) Posterior urethral valves in adult males. Urology 36: 35-37.
- Karanth KS, Yeluri SV, Desai RM, Shah SC (2003) Congenital anterior urethral diverticulum with stone: a unique presentation. Urology 61: 837-839.
- Mutlu N, Calla M, Mutlu B, Acar O, Turcan S, et al. (1998) Cobbs collar and syringocele with stone. Int J Clin Practice 52: 352-353.
- Gonzalvo PV, Botella AR, Canto FE, Gasso MM, Liopis GB, et al. (1998) Urethral diverticulum complicated with giant lithiasis. Actas Urol Esp 22: 250-252.