Keywords
Peutz-Jeghers syndrome;Abdominal pain;Oral mucosal lesions;Intestinal hamartomatous polyps
Case Report
A 9 year-old male child (Master X) was admitted to Pediatric ward, recurrent third admission in the hospital. Presenting complaints were colicky abdominal pain lasting for 6 to 8 hours, oral lesions which were causing discomfort and child was refusing to take anything orally, constipation since last 4 days. On physical examination his abdomen was diffusely tender, laboratory tests were normal and blood cells count showed 21,000 WBC/mm3. Abdominal ultrasonography on admission was normal with some gut gases. Child was complaining of severe weakness and abdominal discomfort.
Birth history of Master X - Second child of parents, normal birth history, no any previous hospitalization.History of febrile convulsions at the age of 8 months.
History during first hospitalization
8 months back; came with complaints of severe abdominal pain, chronic constipation and loss of appetite. On examination oral lesions were seen and abdomen was distended. Blood investigations showed Hemoglobin level of 8.3 mg% and WBC 26000 WBC/mm3, CT scan of abdomen revealed a small bowel intussusceptions and multiple polyps. During Laparotomy an intraluminal bowel polyp was detected, therefore resection of a short length of intestine (about 2.5 cm) followed by anastomosis was performed.
Histological examination of the polyp showed proliferation of the mucosal epithelium.
Post operatively, child was kept Nil per Oral, then liquid diet was started, bowel sounds were present and constipation was relieved. Child got discharged on 12th day of hospitalization and advised for follow up.
History of second hospitalization
After 6 weeks of previous hospitalization, Child complaining of persistent abdominal pain lasting for long period of time. Loss of appetite, presenting with oral lesions on inner cheeks and lips. Discomfort not relieved on any position given to the child. On physical examination abdomen was mild tender, on auscultation gases sound present, not gaining weight due to poor intake, irritable. Parental anxiety was noticed, even after the surgical management child was sick. Abdominal CT Scan not revealing any pathological changes. On blood investigations, Hb was 8.6 mg%, child was put on liquid diet, preferably bland, intake output monitoring, analgesics, oral laxative once at night, flatus tube and observation for any abdominal signs. Child was discharged after 5 days of hospitalization.
History of third hospitalization
After 2.4 weeks of previous hospitalization, child complaining of abdominal discomfort with severe gaseous distention, loss of appetite, irritable and depressed. Oral lesions were worsened compared to previous signs. Child was unable to take orally. Child was managed with oral intake to be taken with the help of oral straw, local application for oral lesions and laxatives for abdominal complaints. Child was discharged after his nutritional improvement, after 7 days of hospitalization.
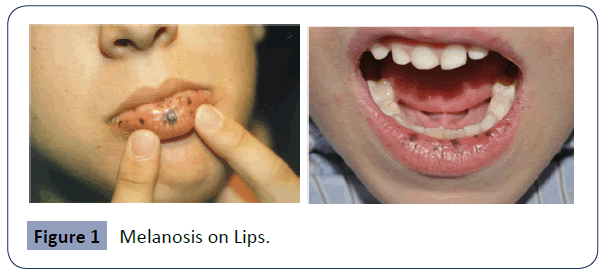
Definition of PJS
Peutz-Jeghers syndrome (abbreviated asPJS) is an autosomal dominant disease, with an incidence of 1/150,000, characterised by hamartomatous polyps of the gastrointestinal tract, mucosal macular melanin deposition in the lips, buccal mucosa, perioral area, hyperpigmented macules on the lips and oral mucosa (melanosis) and/or facial skin, and family history of PJS [1].
It is linked to a variety of intestinal and extraintestinal neoplasms with a cumulative lifetime risk for cancer of 93%, 18 times greater than expected in the general population. According to the WHO criteria the diagnosis of PJS can be made when the presence of mucocutaneous pigmentation, bowel hamartomatous polyps and family history of PJS are found simultaneously.
The syndrome was described in 1921 by Jan Peutz (1886-1957), a Dutch physician who noted a relationship between the intestinal polyps and the mucocutaneousmacules in a Dutch family [2]. The dermatologic component had previously been reported by John McHutchinson in 1896 in identical twins, one of who subsequently died from intussusception [3].
Harold Jeghers (1904-1990), an American physician, then made definitive descriptive reports of the syndrome when he published "Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits," in 1949, with McKusick and Katz. The eponym Peutz-Jeghers syndrome was introduced by the radiologist Andre J Bruwer in 1954 [4].
Epidemiology
Peutz Jeghers syndrome is a rare disorder that affects males and females in equal numbers and can occur in any racial or ethnic group. The birth prevalence of PJS is estimated to be between 1/50,000 and 1/200,000 [5].
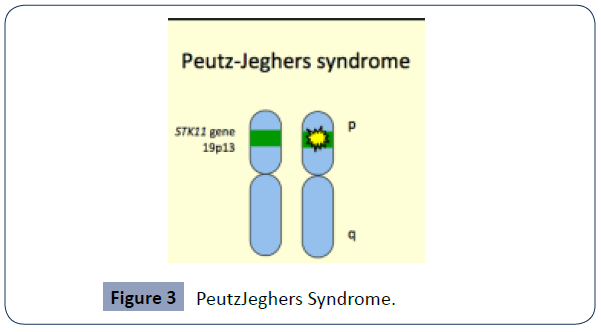
Pathogenesis of peutz-Jeghers syndrome
PJS is the first cancer susceptibility syndrome identified those results from inactivating mutations of protein kinase [6], an autosomal dominant syndrome with incomplete and variable penetrance. About 50% of PJS patients have loss-of-function heterozygous mutations in a tumor suppressor gene STK11 (also known as LKB1 - Liver Kinase B1) on short arm of chromosome 19 p (19p13.3) [6]. It codes for serine/threonine kinase 11, an enzyme that has a role in cell polarity, regulates cell growth and anabolism, and promotes apoptosis (programmed cell death). The loss of second (normal) copy of the gene via somatic mutations leads to uncontrolled cell growth and results in cancers seen in PJS. The absence of STK11 mutation does not exclude the possibility of PJS [7] (Figure 1).
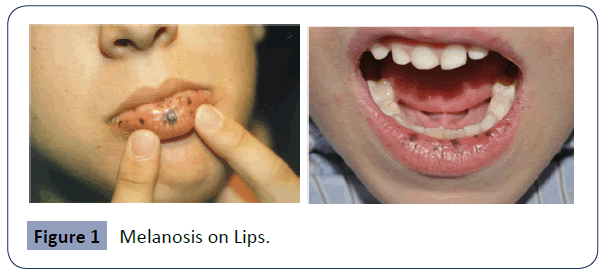
Figure 1 Melanosis on Lips.
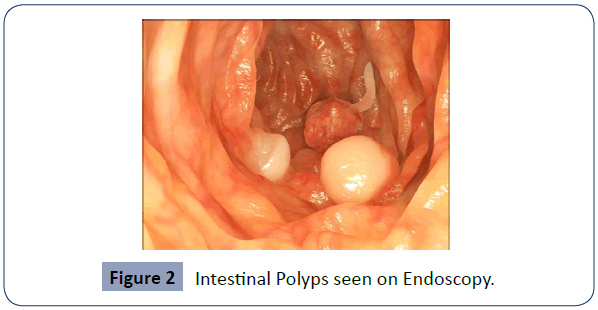
Microscopic (histologic) description: The polyps in patients with PJS have a distinct histological appearance benign hamartomas characterized as’ Frond like’ cores of stromal tissue and smooth muscles surrounded by normal appearing intestinal epithelium [6]. Smaller polyps or those from the stomach and colon, may lack the prominent arborizing smooth muscle. Dysplasia and adenocarcinoma can develop within polyps [8].
• The dark pigmented spots (melanocytic macules) are thought to be caused by inflammation and blockage of melanin migration from cells where it is produced (melanocytes) to cells forming the outermost layer of the skin (keratinocytes) [5].
Causes: Mutation of tumor suppresser gene: PJS is caused by mutations in the STK11/LKB1 gene. Dominant genetic disorders occur when only a single copy of an abnormal gene is necessary for the appearance of the disease. The abnormal gene can be inherited from either parent, or can be the result of a new mutation (de novo) in the affected individual. The risk of passing the abnormal gene from an affected parent to an offspring is 50% for each pregnancy [5,9].
Clinical features
How is PJS diagnosed?
Individuals with at least 2 of the following characteristics may be considered to have PJS:
• At least 2 PJ type hamartomatous polyps in the small intestine
• Characteristic freckling of the mouth, lips, fingers, or toes
• At least 1 relative diagnosed with PJS [10]
The melanocytic macules can be identified with a physical examination,
Polyps can be detected by, x-ray examination, an upper gastrointestinal endoscopy, colonoscopy or wireless capsule endoscopy and are classified as PJS polyps by microscopic examination.
CBC, Stool for occult blood, Carcinoma screening tests (Table 1 and Figure 2).
| From the literatures |
Seen in Master X |
| Abdominal pain |
Recurrent abdominal pain |
| Vomiting, diarrhea [5] |
Constipation |
| Blood in stools |
Not present in this child |
| Gastrointestinal polyps |
Multiple polyps of small intestine |
| Small bowel obstruction, Intussusception |
CT Scan revealed Intussusception |
Hamartomatous polyps - Most common in small bowel 60-90% especially jejunum. Stomach 15-30%, Colon 50% - 50% asymptomatic at diagnosis.
Can present with bleeding, obstruction, intussusception (in upto 70%) [9] |
Intraluminal bowel polyp, showed proliferation of the mucosal epithelium |
| Unusual skin freckling (pale brown spotting on skin) |
Not present in this child |
| Mucocutaneous pigmentation – Seen in 95% patients - 1mm to 5mm in size. – Appears by 1 or 2 years of age. Fades after puberty except buccal mucosa. |
Melanosis seen on lips then inner cheek in oral cavity |
| Anemia. |
Hemoglobin was 8.6mg% |
| Exostosis (bone spur) |
Not seen in child |
Table 1 Comparison of what is normally found in books and what was seen in Master X.
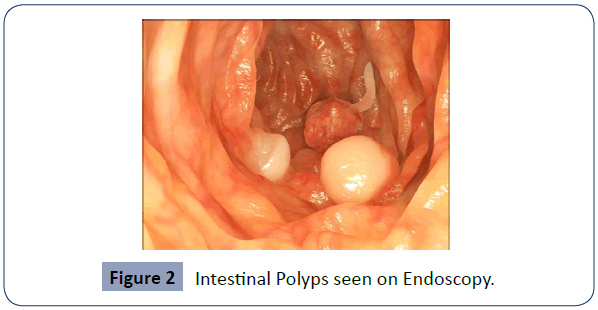
Figure 2 Intestinal Polyps seen on Endoscopy.
Genetic testing for the identification of disease-causing (pathogenic) mutations in the STK11 gene is recommended when any one of the above criteria is present.
Double contrast gastrointestinal studies followed by MRI are considered the gold standard to detect small bowel polyps. Capsule endoscopy is a very sensitive procedure as it allows the detection of polyps <1.5 cm and is useful in the follow-up of PJS patients [11].
In Master X, histology studies, CBC, stool occult was done, parents of the child were unwilling for undergoing any genetic screenings due to financial constraints (Figure 3).
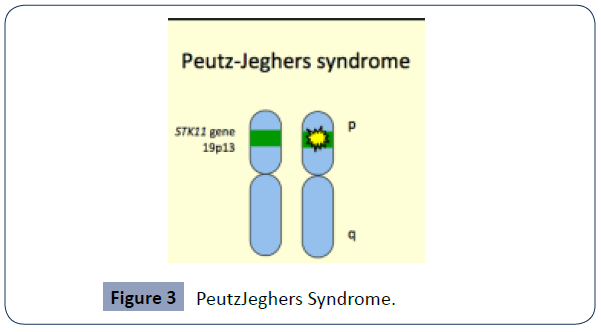
Figure 3 PeutzJeghers Syndrome.
Differential diagnosis:
Literature has presented several differential diagnosis, most common ones identified are-
Enteritis cysticaprofunda
Invasive carcinoma
Henoch-Schonleinpurpura(HSP) [12]
Complications: Intestinal blockage, CA Stomach, CA pancreas, CA breast
An estimated 18-21% risk of ovarian cancer, 9% risk of endometrial cancer, and 10% risk of cervical cancer [13]. Breast cancer 30 to 50%, Colorectal cancer 40%, Pancreatic cancer 10 to 35%, Stomach cancer 30%, Ovaian cancer 20%, Lung cancer 15%, Small intestine cancer 13%, Cervical adenoma malignum cancer 10%, Uterine cancer less than 10%, Testicular cancer less than 10%.
Management
Treatment is mostly focused on surveillance and control of symptoms.
Scientific evidence recommends, after initial diagnosis in children older than 8 years undergo endoscopic and small bowel examination with Magentic Resonance Enterography (MRE) or by video capsule endoscopy (VCE) [5,14], as it is non invasive and painless in children.
• DBE is a new enteroscopy method - consists of a 200-cm enteroscope and a 145-cm over-tube which have soft latex balloons at their tips. These balloons allows gripping the intestinal wall and so the endoscope can be inserted further without forming redundant loops of intestine [15].
• IOE is a combination of laparotomy (or laparoscopy) with endoscopy that allows manipulation and ensures complete small bowel visualization and chances of removal of nearly all polyps in an endoscopic or surgical manner [16] (Table 2).
| Routine endoscopic surveillance with polypectomy |
Decreases the frequency of emergency laparotomy and bowel loss resulting from intussusception. |
| Polyps over 1 cm in size |
Endoscopic removal of polyps (polypectomy) is performed.This avoids polyps-related complications such as bleeding and intussusception. |
| Open Surgery |
To reduce the risk of recurrence of complications and surgery [9] |
| Intra-operative enteroscopy (IOE) |
For small bowel hamartomas |
| Intraoperative enteroscopy with enterotomy is needed occasionally |
Removal of large distal small-bowel polyps [9] |
| Double balloon enteroscopy (DBE) [14] |
Allows examination and treatment of the jejunum and ileum and for removal of deep small-bowel polyps |
| Chemoprevention |
Recent modality |
Table 2 Various management techniques practiced for PJS treatment.
• Chemoprevention: Some recent studies have demonstrated the chemopreventive efficacy of rapamycin on PJS in a mouse model [17,18]. Rapamycin (sirolimus) is a macrolide compound with immunosuppressant properties that is obtained from Streptomyces hydroscopicus. Rapamycin treatment led to a dramatic reduction in polyp burden and size. A significant reduction in microvessel density was seen in polyps from the rapamycin-treated mice compared to those from the control group. The antiangiogenic effect of rapamycin may play a role in polyp reduction [18].
• Laser treatment i.e multiple lasers is an option for clients with dark pigmented spots (melanocytic macules) which is causing psychologically negative impact on them [5,6].
• In Master X, the line of management followed was:
• Surgical treatment – Laporotomy done
• Conservative management – Pain management, liquids with bland diet was followed for nutrition care and oral glycerine for lip and cheek lesions.
To parents - Psychological support and education related to the disease condition of their child.
Nursing management
Assessment: On history taking - No any significant family history, Detailed physical examination done.
On examination- abdomen was tensed, oral lesions seen (Table 3).
| Nursing Diagnosis |
Nursing care provided |
| Acute abdominal pain related to the intestinal dysfunction evidenced by Wong Baker – FACES scale, |
Provided comfort position, changed frequently 2 hourly, along with parents soothing communication as diversion therapy. |
Disturbed bowel elimination related to gastrointestinal problem evidenced by constipation,
Imbalanced nutrition related to disease evidenced by oral lesions, |
Provided liquid diet, encouraged mobilization nearby the ward unit, laxatives given at night Followed diet chart and provided timely food and fluids, followed Intake-output monitoring |
| Impaired skin integrity on oral lips related to the disease evidenced by melanosis on the lips and oral cheeks. |
Mouth care provided with soothing lotion and emollient applied – oral glycerine on lips and inner cheeks lesion. |
| Disturbed family environment related to the child’s pain and appetite evidenced by the parents anxiety and unhappiness |
Health education regarding disease condition, care about their child at home, suggested genetic screening if affordable.
Psychological support provided by convincing and positive thinking. |
Table 3 Nursing care for child with PJS
Child was irritable, depressed,
Evaluation: Master X’s oral intake was improving, pain was decreased, gradually the irritation was decreasing, child was unhappy in hospital environment, wanting to be at his home at earliest.
Prognosis: Most people with Peutz-Jeghers syndrome will have developed some form of neoplastic disease by age 60. Cumulative risks by age 70 for all cancers 85%, gastrointestinal cancers (GI) 57% and pancreatic cancer are and 11% [19].
Master Xwas hospitalized recurrently, abdominal pain was persistent, appetite was deteriorating, child was showing irritation and depression, uninterested in the hospital environment.
Prevention:
• Genetic counseling - Consultation with a clinical genetic specialist and counselor, Prevention of primary manifestations- based on the family history or other clinical factors. Genetic testing to be done at-risk relatives, so as for early treatment and management [5,9]
• Diagnostic tests - endoscopy, colonoscopy, and small bowel examination to be done every 2-3 years to detect polyps and related potential tumors.
Gynecologic and breast examination with mammography, Papanicolaou smear (Pap smear) annually for females beginning at age 18-20 [13]. Prophylactic mastectomy and prophylactic hysterectomy and bilateral salpingo-oophorectomy to manage high risk for breast cancer and gynecologic malignancy respectively after 35 years of agefor males - Testicular examination.
Radiology screening- USG, Esophago-gastro-duodenoscopy and colonoscopy, CT scan or MRI – for assessing gastrointestinal condition, preferably every 2 years.
Surveillance - Protocols have been suggested for monitoring stomach, small and large bowel, breasts, testicles, ovaries, uterus, and pancreas by various procedures as early as birth and as frequently as once a year [5,9].
Conclusion
Peutz_Jeghers Syndrome is a rare autosomal dominant disorder characterized by intestinal hamartomatous polyps, mucocutaneousmelanotic pigmentation and predisposition to malignancies. Although the incidence of PJS is low, it is important for nurses to gain knowledge about this rare condition in children. Since it is a chronic illness with future complications in further life of the child, a comprehensive care needs to be practiced for making child live with the condition in better situation. An holistic approach towards the child and family should be practiced by utilizing holistic nursing theory application, appropriate guidance regarding genetic screening and counseling to be encouraged for the risk families. Financial implications needs to be understood. So can contribute in preventing morbidity and mortality in the children.
Ethical Consideration
Permission obtained from hospital authorities.
Parents of Master X consented for taking the case but not for the personal details and related photography of their child. Copyright clinical pictures attached to this report for clear view of the disease condition.
Conflict of Interest
Nil
37654
References
- Achatz Mi, Porter CC, Brugieres l, Druker H, Frebourg T, et al. (2017) Cancer screening recommendations and management of inherited gastrontestinal cancer syndromes in childhood. Clin Cancer Res 23: e107-114.
- John Hopkin University, booklet on PJS, Internal Medicine, Springer Link site.
- To BAT, Geneesk NM (2018) Case of familial polyposis of mucous membrane of intestinal tract and nasopharynx accompanied by peculiar pigmentations of skin and mucous membrane. N Engl J Med 10: 134-146.
- Jeghers H, McKusick VA, Katz KH (1949) Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits; a syndrome of diagnostic significance. N Engl J Med 241:1031-1036.
- Leveille E, McGarrity TJ, Amos CI, Baker MJ (2020) NORD -National organization of rare disease. 2019 Peutz-Jeghers Syndrome.
- Kliegman RM, Behram RE, Jenson HB, Stanton B (2007) Nelson Textbook of Pediatrics, 18e 18th Edition, Kindle Edition.
- Ramnani D (2020) High Quality Pathology Images of Benign and Malignant Neoplasms and Related Entities. Web pathology.
- TseJY, Wu S, Shinagare SA, Lauwers GY, Yilmaz O, et al. (2013) Peutz-Jeghers syndrome: a critical look at colonic Peutz-Jeghers polyps. Mod Pathol 26:1235-1240.
- 9.Radio FC, Grammatico P (2016) Peutz- Jeghers syndrome. Atlas Genet and Cytogenet Oncol and Hematol 20:583-586.
- SkolarusTA, Wolf AMD,ErbNL, Brooks DD, et al. (2014) American Cancer Society prostate cancer survivorship care guidelines. American Cancer Society J 64: 225-249.
- Kurugoglu S, Aksoy H, Kantarci F, Cetinkaya S, Mihmanli I, et al. (2003) Radiological work-up in Peutz-Jeghers syndrome. Pediatr Radiol 33: 766–771.
- RingKL, Garcia C, Thomas MH, Modesitt SC(2017) Current and future role of genetic screening in gynecologic malignancies. Am J Obstet Gynecol 217:512-521.
- Kopacova M, Tacheci I, Rejchrt S, Bures J (2009) Peutz-Jeghers syndrome: Diagnostic and therapeutic approach. World J Gastroenterol 15: 5397–5408.
- Yano T, Yamamoto H (2009) Vascular, polypoid, and other lesions of the small bowel. Best Pract Res Clin Gastroenterol 23: 61–74.
- Fraser JD, Briggs SE, St Peter SD, De Petris G, Heppell J (2009) Intussusception in the adult: an unsuspected case of Peutz-Jeghers syndrome with review of the literature. Fam Cancer 8:95–101.
- 17 Wei C, Amos CI, Zhang N, Zhu J, Wang X, et al. (2009) Chemopreventive efficacy of rapamycin on Peutz-Jeghers syndrome in a mouse model. Cancer Lett 277:149–154.
- Robinson J, Lai C, Martin A, Nye E, Tomlinson I, et al. (2009) Oral rapamycin reduces tumour burden and vascularization in Lkb1(+/-) mice. J Pathol219: 35–40.
- Riegert-Johnson D, Gleeson FC, Westra W, Hefferon T, Song LMWK, et al. (2001) Peutz-Jeghers Syndrome. National Center for Biotechnology Information (US); 2009-2008 July.