Keywords
Epidural hematoma; Lonomia Obliqua; Antilonomic serum antidote
Introduction
Accidents with bristles of Lonomia (or commonly known as the Taturana) are often associated with a coagulation disorder and a hemorrhagic syndrome [1]. It was first described by Arocha – Pinango in Venezuela in 1967 [2]. After 24 hours, a severe bleeding disorder ensues, leading to ecchymoses, pulmonary and intracranial hemorrhages [3,4] was well as acute renal failure [2,5]. Since 1989 accidents by Lonomia have been reported in the southern region of Brazil [6], with an incidence of 1.1 to 24.6 cases for one hundred thousand inhabitants [7]. Envenoming Lonomia has a reported fatality rate of approximately 1.7% [8] to 2.5% [7]. In the present report, we describe a rare case of severe coagulation disorder in a 2.5 year old female child who came in contact with bristles of the caterpillar Lonomia obliqua, (Figure 1) having received specific anti-lonomic antidote serum and neurosurgical evacuation of a massive epidural hematoma, as well as performed a systematic literature review.

Figure 1: Image of a specimen of Lonomia obliqua, demonstrating the numerous distinct bristles that are usually the first parts of the caterpillar to come in contact with the patient and from which the toxin is liberated.
Case Presentation
A 2.5 year old female child, previously healthy, accidentally came into contact with a caterpillar in the anterior surface of the right thigh, initially presenting erythema at the site of contact. Three days after the accident she developed oral mucosa bleeding. Approximately ninety-six hours later she presented headache, nausea and vomiting, as well as rapid progression of decrease in level of consciousness. Five days after the accident, she presented generalized tonic-clonic seizures, being then transferred to Intensive Care Unit (ICU) of São Vicente de Paulo Hospital.
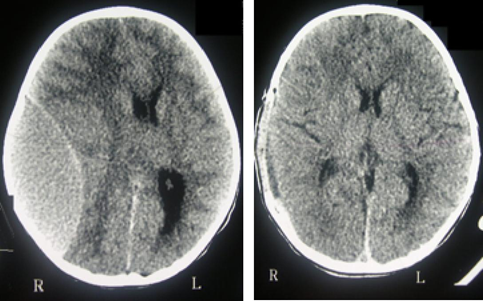
On admission, she was comatose, presenting GCS (Glasgow Coma Scale) of seven, right pupil dilatation, as well as bilateral Babinski sign. Oro-tracheal intubation was performed and appropriate clinical support immediately initiated. CT-scan Imaging revealed a right Epidural Hematoma causing important mass effect, with median line deviation (Figure 2).
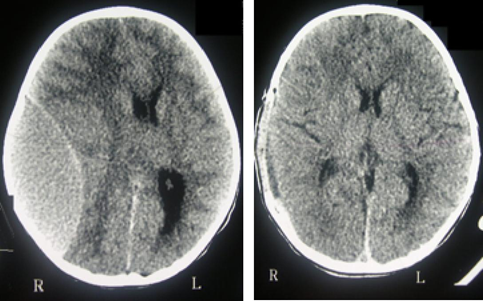
Figure 2:(a) Pre-operative CT-scan of a two-year five-month female patient, victim of direct skin contact with bristles of the Lonomia obliqua and a right fronto-parietal epidural massive hematoma, with important mass effect and midline deviation. 2(B) Post-operative CT-scan of the same patient after red blood cell infusion, anti lonomic antidote administration and neurosurgical evacuation of the epidural hematoma.
Laboratory examination exhibited thrombin time of 31.5 seconds, International Normalized Ratio (INR) of 2.71, activated partial thromboplastin time of 51.2 seconds, incoagulable clot time, a result of zero of fibrinogen, hemoglobin level of 8.2 g percentage, and normal platelets count. Subsequent laboratory testing showed no significant alterations.
She received anti lonomic antidote serum, divided in two doses, red blood cell infusion, mannitol, and then underwent neurosurgical treatment for evacuation of the epidural hematoma. Surgery elapsed without complications; hematoma was completely evacuated, and hemostasis was adequately performed, with special care due to coagulopathy of the case in stake. The patient evolved well after the procedure, remaining clinically stable.
On first post-operative day, the patient exhibited a clinically stable course, but later on presented fever, being opted to initiate antibiotic treatment with a third generation cephalosporin for respiratory infection, based on radiographic and laboratory findings. The subsequent laboratory testing demonstrated the subsequent improvements: thrombin time of 15.6 seconds, an INR of 1.31, activated partial thromboplastin time of 29 seconds, clot time of 5 minutes, fibrinogen of 360 mg% and a hemoglobin level of 9.7 g%.
The patient gradually improved clinically, with visible neurological improvement, normal laboratory testing on the ninth post-operative day and a modified Ranking Scale of 2. She was discharged from the hospital on the sixteenth postoperative day, with a GCS of 15 and mRS of 2, partial recovery of the right third and seventh cranial nerve palsies, with later follow-up demonstrating total recovery of the CN palsies (Table 1).
| |
Post-incident day |
| Parameter |
5 |
6 |
9 |
14 |
Normal |
| Hemoglobin |
8.2 |
9.7 |
11.2 |
11.4 |
12-16 g/dL |
| Hematocrit |
25 |
29 |
34 |
34 |
37-42% |
| Platelets |
260 |
220 |
183 |
895 |
140-400 × 103/mm3 |
| Urea |
15 |
10 |
- |
18 |
15-45 mg% |
| Creatinine |
0.51 |
0.55 |
0.36 |
0.46 |
0.60-1.40 mg% |
| TB |
0.5 |
- |
- |
- |
0.0-1.0 mg/dL |
| PTT |
51.2 |
29 |
41.1 |
21 |
20.0-34.0 sec |
| PT INR |
2.71 |
1.31 |
1.19 |
1 |
1 |
| PT Activity |
23.7 |
61.7 |
73 |
100 |
70-100% |
| Fibrinogen |
0 |
360 |
- |
- |
150-450 mg% |
| CT |
Incoagulable |
5 |
- |
- |
5-10 sec |
*TB = Total Bilirubin; PTT = Partial Thromboplastin time; PT = Prothrombin time; CT = Clot time.
Table 1: Composition of diets.
Discussion
Responsible for severe hemorrhagic accidents in Southern states of the country, the caterpillar of the species Lonomia obliqua, also known commonly as the Taturana, in its larval stage and through its bristles, releases a toxin with anticoagulant properties, which, in contact with the skin may produce symptoms ranging from local cutaneous irritation and subcutaneous hemorrhages to more severe hemorrhages that can affect vital organs. The caterpillar Lonomia obliqua is a known parasite of Araticum, Cedro and Ipe, native southern Brazilian trees, but appears to have adapted to fruit trees of the regions of occurrence, such as peach, avocado and plum trees, among others.
The seasons of greater occurrences of accidents are in the spring and summer (peaks in February and March), periods that correspond to the maggot stage of the insect. Most of the accidents occur in the rural area, next to residencies and in the working places, and the upper limbs are the places more commonly injured. There is a reported predominance in the middle-south, southwest and southeast regions of Brazil.
In vitro studies of the Lonomia crude bristles extract have demonstrated that this toxin induces clot formation by triggering activation of both prothrombin and Factor X [9]. The toxin exerts procoagulant activity consumption coagulopathy leading to a hemorrhagic state induced by fibrinogen depletion and secondary fibrinolysis.
The consumptive coagulopathy associated with Lonomia seems to be different from that observed in Disseminated Intravascular Coagulation (DIC), since that in the former there is no reduction of factors XII, II and X, and the platelet number remains unaltered.
The coagulopathy here can last for two to five weeks [8].
Envenoming occurs when a person touches or smashes the Lonomia, breaking the spicules and releasing the venomous secretions on the victim’s skin [10].
Presentation of the symptoms of Lonomia envenoming may generally be classified as follows: Erucism (a local inflammatory reaction characterized by localized, pruritic maculopapular to bullous contact dermatitis and urticaria caused by contact with or airborne exposure to Lonomia urticating hairs, spicules or toxic hemolymph [11]), Lepidopterism (systemic reactions), Dendrolimiasis (a chronic form of lepidopterism), Ophthalmia nodosa, and consumptive coagulopathy with secondary fibrinolysis [3].
Severity of manifestations depends on the number of larvae, larval stage, and surface extension of the patient’s skin involved. Initial symptoms are pain, burning sensation, hyperemia, edema, headache, nausea and vomiting. These symptoms are generally followed by systemic reactions associated with a severe coagulopathy and bleeding manifestations, and usually occur during the first twelve hours after the accident [12].
Laboratory findings include a normal platelet count, anemia, a prolonged prothrombin time, and decreased fibrinogen, plasminogen, factor V and factor XIII levels associated with increased fibrin degradation products [13]. Therapy with whole blood or fresh frozen plasma are contraindicated because results in a sharp decrease in platelet count, leading to renal insufficiency and death [3]. Aspirin–containing drugs are contraindicated in potential Lonomia envenomings [11].
In recent years, Butantan Institute, from São Paulo, Brazil, developed anti-lonomic serum for specific treatment of envenomation caused by contact with Lonomia. Early diagnosis and an adequate treatment, particularly within the first 12 hours, could prevent severe coagulopathy. After the introduction of Lonomia toxin antidote, no more deaths were reported [12].
The general management of Lonomia envenoming is clinical treatment and anti-lonomic antidote. Immediate water washing of the sting site, in order to remove toxic hemolymph and any loose urticating hairs are of utmost importance as to attempt reduction of toxin spread [11].
Conclusion
Although cases of Lonomia envenoming have previously been reported, the case reported here was a severe case of epidural hematoma related to coagulopathy induced by caterpillar contact that evolved surprisingly well after clinical support and neurosurgical treatment, enabled by the administration of the specific antidote, the anti-lonomic serum.
9745
References
- Veiga ABG, Ribeiro JMC, Guimarães JA (2005) A catalog for the transcripts from the venomous structures of the caterpillar Lonomiaobliqua: Identification of the proteins potentially involved in the coagulation disorder and hemorrhagic syndrome. Gene 355: 11-27.
- Malaque CMS, Andrade L, Madalosso G (2006) Short report: A case of hemolysis resulting from contact with aLonomiacaterpillar in Southern Brazil. American Journal of Tropical Medicine and Hygiene 74: 807-809.
- Kowacs PA, Cardoso J, Entres M (2006) Fatal intracerebral hemorrhage secondary to LonomiaObliquacaterpillar envenoming. ArquivosNeuropsiquiatria 64: 1030-1032.
- Cardoso AEC, Haddad Junior V (2005) Accidents caused by lepidopterans (moth larvae and adult): study on the epidemiological, clinical and therapeutic aspects. AnaisBrasileiros de Dermatologia 80: 571- 578.
- Fan HW, Cardoso JLC, Olmos RD (1998) Hemorrhagic syndrome and acute renal failure in a pregnant woman after contact with Lonomiacaterpillars. A case report. Revista do Instituto de Medicina Tropical de São Paulo 40.
- Garcia CM, Danni Oliveira IM (2007) Occurrence of accidents caused by Lonomia oblique walker, in the state of Paraná between 1989 and 2001. Revista da SociedadeBrasileira de Medicina Tropical 40: 242-246.
- Correa MS, Siqueira BR, Gomes AP (2004) Lonomiaerucismin Teresópolis, Rio de Janeiro State, Brazil. Report of a probable case and review. Revista da SociedadeBrasileira de Medicina Tropical 37: 418-421.
- Norris R (2007) Caterpillar envenomations. Disponívelem: https://www.emedicine.com/EMERG/topic794.htm.
- ChudzinskiTavassi AM, Flores MPA (2005) Exploring new molecules and activities from Lonomiaobliquacaterpillars. Pathophysiology of Haemostasis and Thrombosis 34: 228-233.
- Veiga ABG, Pinto AFM, Guimaraes JA (2003) Fibrinogenolytic and procoagulant activities in the hemorrhagic syndrome caused by Lonomiaobliquacaterpillars. Thrombosis Research 111: 95-101.
- Diaz JH (2005) The evolving global epidemiology, syndromic classification, management, and prevention of caterpillar envenoming. American Journal of Tropical Medicine and Hygiene 72: 347-357.
- ChudzinskiTavassi AM, CarrijoCarvalho LC (2006) Biochemical and biological properties of Lonomiaobliquabrisltle extract. Journal of Venomous Animals and Toxins including Tropical Diseases 12: 156-171.
- ArochaPinango CL, Marchi R, Guerrero B (1999) Inventory of exogenous hemostatic factors derived from arthropods. Thrombosis Haemostasis 81: 647-656.